The state of alarm was declared in Spain due to the COVID-19 epidemic on March 14, 2020, and established population confinement measures. The objective is to describe the process of lifting these mitigation measures.
MethodsThe Plan for the Transition to a New Normality, approved on April 28, contained four sequential phases with progressive increase in socio-economic activities and population mobility. In parallel, a new strategy for early diagnosis, surveillance and control was implemented. A bilateral decision mechanism was established between the Spanish Government and the autonomous communities (AC), guided by a set of qualitative and quantitative indicators capturing the epidemiological situation and core capacities. The territorial units were established ad-hoc and could be from Basic Health Zones to entire AC.
ResultsThe process run from May 4 to June 21, 2020. AC implemented plans for reinforcement of core capacities. Incidence decreased from a median (50% of territories) of 7.4 per 100,000 in 7 days at the beginning to 2.5 at the end. Median PCR testing increased from 53% to 89% of suspected cases and PCR total capacity from 4.5 to 9.8 per 1000 inhabitants weekly; positivity rate decreased from 3.5% to 1.8%. Median proportion of cases with traced contacts increased from 82% to 100%.
ConclusionSystematic data collection, analysis, and interterritorial dialogue allowed adequate process control. The epidemiological situation improved but, mostly, the process entailed a great reinforcement of core response capacities nation-wide, under common criteria. Maintaining and further reinforcing capacities remained crucial for responding to future waves.
El 14 de marzo de 2020 España declaró el estado de alarma por la pandemia por COVID-19 incluyendo medidas de confinamiento. El objetivo es describir el proceso de desescalada de estas medidas.
MétodosUn plan de transición hacia una nueva normalidad, del 28 de abril, incluía 4 fases secuenciales incrementando progresivamente las actividades socioeconómicas y la movilidad. Concomitantemente, se implementó una nueva estrategia de diagnóstico precoz, vigilancia y control. Se estableció un mecanismo de decisión bilateral entre Gobierno central y comunidades autónomas (CCAA), guiado por un panel de indicadores cualitativos y cuantitativos de la situación epidemiológica y las capacidades básicas. Las unidades territoriales evaluadas comprendían desde zonas básicas de salud hasta CCAA.
ResultadosEl proceso se extendió del 4 de mayo al 21 de junio y se asoció a planes de refuerzo de las capacidades en las CCAA. La incidencia disminuyó de una mediana inicial de 7,4 por 100.000 en 7 días a 2,5 al final del proceso. La mediana de pruebas PCR aumentó del 53% al 89% de los casos sospechosos, y la capacidad total de 4,5 a 9,8 pruebas semanales por 1.000 habitantes; la positividad disminuyó del 3,5% al 1,8%. La mediana de casos con contactos trazados aumentó del 82% al 100%.
ConclusiónLa recogida y análisis sistemático de información y el diálogo interterritorial logaron un adecuado control del proceso. La situación epidemiológica mejoró, pero sobre todo, se aumentaron las capacidades, en todo el país y con criterios comunes, cuyo mantenimiento y refuerzo fue clave en olas sucesivas.
The rapid increase in cases of COVID-19 in Spain, as well as in other European countries, during the first half of March 2020, urged the National Governments to implement sound physical distancing measures to avoid health systems becoming overwhelmed. Spain is a “quasi-federal” country and the most appropriate mechanism allowing the Government to implement generic physical distancing and mobility control measures all over the national territory is the declaration of the state of alarm. It was declared on March 14th, and was coupled with the closure of educational institutions and non-essential stores, events and venues, cancellation of all visits to closed institutions, especially prisons and nursing homes, in addition to a blanket recommendation to work from home and prohibition of non-essential transit.1 This was further reinforced by cancellation of all non-essential economic activities between March 30th and April 8th, followed by Easter holidays from April 9th to 12th.2 These measures managed to rapidly control the growth of the epidemic, with new cases peaking on March 26th at around 10,000 cases per day, and then dropping sharply.3 At this stage, cases corresponded mostly to severe cases who required hospital admission. By late April, new cases were slightly above 1000 per day with a steady decreasing trend.
Mitigation measures have a high social and economic impact and might not be sustainable during a long period of time; however, the process of re-opening the economy, and the increase of human mobility and social life presents many challenges, bearing in mind the risk of a rapid rebound in transmission if restrictions are lifted too quickly.4,5
Lifting of mitigation measures is only possible if adequate case finding, case isolation and contact tracing is in place, as has been demonstrated by different modeling studies6–8 and acknowledged by international organizations.4,9,10 Because of this, as a cornerstone of the deconfinement process, a new Strategy for early diagnosis, surveillance and control of COVID-19 was approved nationally and implemented on May 11th,11 establishing that every suspected case, regardless of severity, needed to be PCR tested and every contact investigated, PCR tested, and put under quarantine. Until then, similarly to other European countries,12 severe cases had been prioritized for PCR testing and mild cases were not routinely tested, due to the limitation in the number of daily PCR tests that could be performed in the early stages of the outbreak and to limitations in the number of PCR testing kits available in the market worldwide during several weeks. In addition, public health services did not have yet the necessary resources to perform contact tracing of every case during the ascending phase of the outbreak with wide, uncontrolled community transmission. With the new strategy, autonomous communities (AC, the first-level territorial divisions within Spain) were required to make the necessary investments to effectively implement the new test, trace & isolate protocols.
The objective of this article is to describe the characteristics of the process of lifting lockdown in Spain, review the evolution of core indicators and provide some reflections on the limitations and challenges posed by this process.
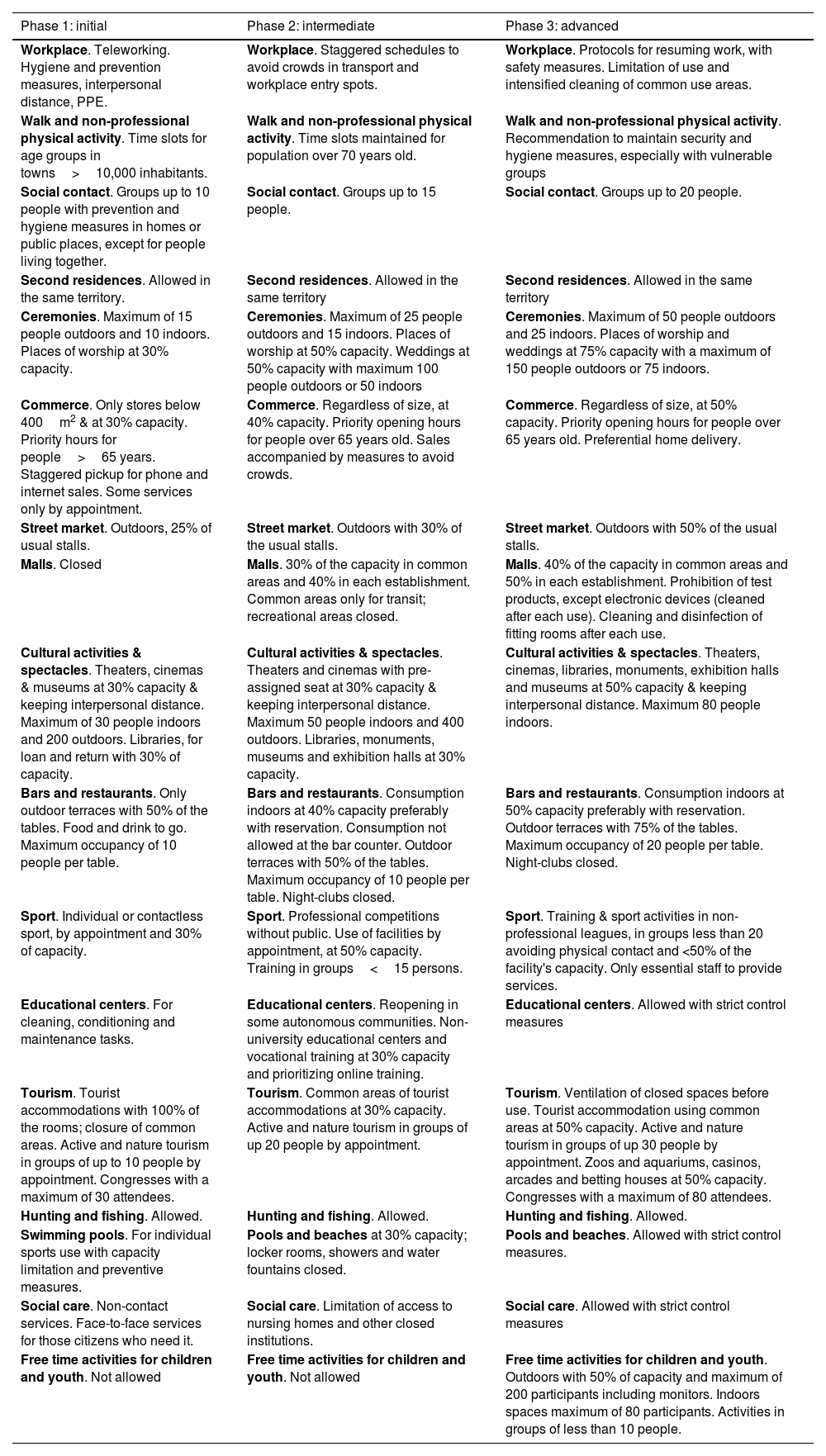
Materials and methodsOn April 28th, the Spanish Government approved the Plan for the Transition to a New Normality (PTNN),13 which refers to a mix of prevention and control measures that are sustainable over time and help keep the COVID-19 epidemic under control until effective tools such as treatments or vaccines become available. The PTNN foresaw four sequential phases (0–3) with a progressive increase in socio-economic activities and population mobility (Table 1). Each phase, in principle, should last at least 14 days to allow observing the effects in the epidemiological situation before progressing further. Additionally, given the high heterogeneity across the territory, the pace of progression should be tailored to the local context, for which different territorial units were established by AC upon epidemiological, geographical, economic and social criteria; these could be as big as AC or as small as Basic Health Zones. The delimitation of the territories that would progress through the phases was defined and rearranged along the process, generally by merging smaller areas, until the territories consisted mostly of full provinces. For the sake of simplicity for this communication, territories that were as small as Basic Health Zones have been regrouped and assigned the date and characteristics at progression of the last territory of their province. No mobility was allowed between different territorial units, except when two neighboring territories were concurrently in phase 3 and was explicitly allowed after a formal request.
Description of the activities allowed in the progressive phases in the Plan for the transition to a new normality.
| Phase 1: initial | Phase 2: intermediate | Phase 3: advanced |
|---|---|---|
| Workplace. Teleworking. Hygiene and prevention measures, interpersonal distance, PPE. | Workplace. Staggered schedules to avoid crowds in transport and workplace entry spots. | Workplace. Protocols for resuming work, with safety measures. Limitation of use and intensified cleaning of common use areas. |
| Walk and non-professional physical activity. Time slots for age groups in towns>10,000 inhabitants. | Walk and non-professional physical activity. Time slots maintained for population over 70 years old. | Walk and non-professional physical activity. Recommendation to maintain security and hygiene measures, especially with vulnerable groups |
| Social contact. Groups up to 10 people with prevention and hygiene measures in homes or public places, except for people living together. | Social contact. Groups up to 15 people. | Social contact. Groups up to 20 people. |
| Second residences. Allowed in the same territory. | Second residences. Allowed in the same territory | Second residences. Allowed in the same territory |
| Ceremonies. Maximum of 15 people outdoors and 10 indoors. Places of worship at 30% capacity. | Ceremonies. Maximum of 25 people outdoors and 15 indoors. Places of worship at 50% capacity. Weddings at 50% capacity with maximum 100 people outdoors or 50 indoors | Ceremonies. Maximum of 50 people outdoors and 25 indoors. Places of worship and weddings at 75% capacity with a maximum of 150 people outdoors or 75 indoors. |
| Commerce. Only stores below 400m2 & at 30% capacity. Priority hours for people>65 years. Staggered pickup for phone and internet sales. Some services only by appointment. | Commerce. Regardless of size, at 40% capacity. Priority opening hours for people over 65 years old. Sales accompanied by measures to avoid crowds. | Commerce. Regardless of size, at 50% capacity. Priority opening hours for people over 65 years old. Preferential home delivery. |
| Street market. Outdoors, 25% of usual stalls. | Street market. Outdoors with 30% of the usual stalls. | Street market. Outdoors with 50% of the usual stalls. |
| Malls. Closed | Malls. 30% of the capacity in common areas and 40% in each establishment. Common areas only for transit; recreational areas closed. | Malls. 40% of the capacity in common areas and 50% in each establishment. Prohibition of test products, except electronic devices (cleaned after each use). Cleaning and disinfection of fitting rooms after each use. |
| Cultural activities & spectacles. Theaters, cinemas & museums at 30% capacity & keeping interpersonal distance. Maximum of 30 people indoors and 200 outdoors. Libraries, for loan and return with 30% of capacity. | Cultural activities & spectacles. Theaters and cinemas with pre-assigned seat at 30% capacity & keeping interpersonal distance. Maximum 50 people indoors and 400 outdoors. Libraries, monuments, museums and exhibition halls at 30% capacity. | Cultural activities & spectacles. Theaters, cinemas, libraries, monuments, exhibition halls and museums at 50% capacity & keeping interpersonal distance. Maximum 80 people indoors. |
| Bars and restaurants. Only outdoor terraces with 50% of the tables. Food and drink to go. Maximum occupancy of 10 people per table. | Bars and restaurants. Consumption indoors at 40% capacity preferably with reservation. Consumption not allowed at the bar counter. Outdoor terraces with 50% of the tables. Maximum occupancy of 10 people per table. Night-clubs closed. | Bars and restaurants. Consumption indoors at 50% capacity preferably with reservation. Outdoor terraces with 75% of the tables. Maximum occupancy of 20 people per table. Night-clubs closed. |
| Sport. Individual or contactless sport, by appointment and 30% of capacity. | Sport. Professional competitions without public. Use of facilities by appointment, at 50% capacity. Training in groups<15 persons. | Sport. Training & sport activities in non-professional leagues, in groups less than 20 avoiding physical contact and <50% of the facility's capacity. Only essential staff to provide services. |
| Educational centers. For cleaning, conditioning and maintenance tasks. | Educational centers. Reopening in some autonomous communities. Non-university educational centers and vocational training at 30% capacity and prioritizing online training. | Educational centers. Allowed with strict control measures |
| Tourism. Tourist accommodations with 100% of the rooms; closure of common areas. Active and nature tourism in groups of up to 10 people by appointment. Congresses with a maximum of 30 attendees. | Tourism. Common areas of tourist accommodations at 30% capacity. Active and nature tourism in groups of up 20 people by appointment. | Tourism. Ventilation of closed spaces before use. Tourist accommodation using common areas at 50% capacity. Active and nature tourism in groups of up 30 people by appointment. Zoos and aquariums, casinos, arcades and betting houses at 50% capacity. Congresses with a maximum of 80 attendees. |
| Hunting and fishing. Allowed. | Hunting and fishing. Allowed. | Hunting and fishing. Allowed. |
| Swimming pools. For individual sports use with capacity limitation and preventive measures. | Pools and beaches at 30% capacity; locker rooms, showers and water fountains closed. | Pools and beaches. Allowed with strict control measures. |
| Social care. Non-contact services. Face-to-face services for those citizens who need it. | Social care. Limitation of access to nursing homes and other closed institutions. | Social care. Allowed with strict control measures |
| Free time activities for children and youth. Not allowed | Free time activities for children and youth. Not allowed | Free time activities for children and youth. Outdoors with 50% of capacity and maximum of 200 participants including monitors. Indoors spaces maximum of 80 participants. Activities in groups of less than 10 people. |
Although the state of alarm contemplates the designation of a sole command, a bilateral decision mechanism was established between the Spanish Government and the regional Governments of each AC with continuous dialogue and a weekly high-level progress-review meeting regulated by Ministerial Order SND/387/2020.14 An evaluator team formed by 14 public health professionals coordinated by the General Director for Public Health and the Director of the Coordinating Centre for Health Alerts and Emergencies was appointed at the Ministry of Health. Each AC appointed a focal point to act as the lead of the process in its territory; they were in charge of requesting the progression of all or part of their territory weekly, preparing the necessary data and documentation, and maintaining continuous communication with their counterparts in the Ministry.
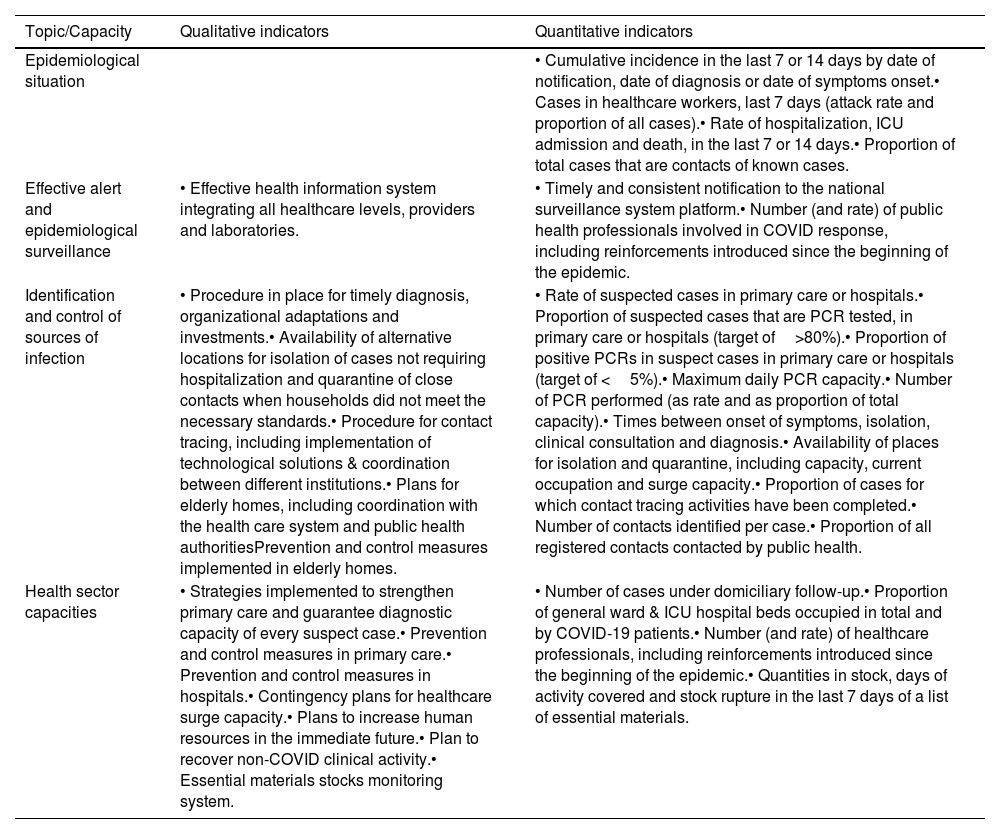
The decision to progress from one phase to the next was guided by a set of specific indicators that captured both the epidemiological situation and core health sector capacities of the territories, namely, a reinforced capacity to provide health-care to COVID-19 cases, an effective epidemiological surveillance system, and rapid identification and control of sources of infection (Table 2). A standardized application template was issued for each AC to provide and reflect upon a set of indicators and qualitative information on these core capacities. Case-definitions followed the common framework of the new Strategy for early diagnosis, surveillance and control of COVID-19.13 Each AC provided indicators’ values from their own available data sources, which were compared to equivalent indicators calculated with information available centrally, to achieve an agreement on the status of each indicator in the panel. Centrally available data sources included: comprehensive case notifications from epidemiological surveillance departments in the AC to the national surveillance platform (SiViES – managed by the National Centre of Epidemiology – Institute of Health Carlos III) which also contained information on the number of contacts identified per case; the national database of laboratory tests (SERLAB), receiving all PCR tests performed in public and private laboratories; and the information system on hospital capacity (CMC), receiving direct notification from public and private hospitals on admitted and discharged patients, active beds, and beds occupied by COVID-19 patients. All databases were updated daily and have national coverage. Qualitative elements, such as established diagnostic circuits, surge capacity activation plans, procedures to resume non-COVID healthcare activities safely, or health-care facilities plans, among others (Table 2) were also discussed and reviewed during the process. No strict cut-offs were set, except for health-care surge capacity, which required that every territory was able to, within 5 days, reach, at minimum, 37 hospital beds and 1–2 ICU beds per 10,000 inhabitants. This capacity could be implanted in their own territory, or be reached through procedures for transfer of patients to other territories with exceeding capacity. Provision of additional data, discussions and clarification of details were part of the dialogue between counterparts at the Ministry and the Autonomous Communities, which had the objective of building consensus. In case of non-agreement, the last decision on whether a territory could progress to the next phase was with the Minister of Health.
Indicators for the assessment of the epidemiological situation and the health core capacities to decide the progression from one phase to the next one.
| Topic/Capacity | Qualitative indicators | Quantitative indicators |
|---|---|---|
| Epidemiological situation | • Cumulative incidence in the last 7 or 14 days by date of notification, date of diagnosis or date of symptoms onset.• Cases in healthcare workers, last 7 days (attack rate and proportion of all cases).• Rate of hospitalization, ICU admission and death, in the last 7 or 14 days.• Proportion of total cases that are contacts of known cases. | |
| Effective alert and epidemiological surveillance | • Effective health information system integrating all healthcare levels, providers and laboratories. | • Timely and consistent notification to the national surveillance system platform.• Number (and rate) of public health professionals involved in COVID response, including reinforcements introduced since the beginning of the epidemic. |
| Identification and control of sources of infection | • Procedure in place for timely diagnosis, organizational adaptations and investments.• Availability of alternative locations for isolation of cases not requiring hospitalization and quarantine of close contacts when households did not meet the necessary standards.• Procedure for contact tracing, including implementation of technological solutions & coordination between different institutions.• Plans for elderly homes, including coordination with the health care system and public health authoritiesPrevention and control measures implemented in elderly homes. | • Rate of suspected cases in primary care or hospitals.• Proportion of suspected cases that are PCR tested, in primary care or hospitals (target of>80%).• Proportion of positive PCRs in suspect cases in primary care or hospitals (target of <5%).• Maximum daily PCR capacity.• Number of PCR performed (as rate and as proportion of total capacity).• Times between onset of symptoms, isolation, clinical consultation and diagnosis.• Availability of places for isolation and quarantine, including capacity, current occupation and surge capacity.• Proportion of cases for which contact tracing activities have been completed.• Number of contacts identified per case.• Proportion of all registered contacts contacted by public health. |
| Health sector capacities | • Strategies implemented to strengthen primary care and guarantee diagnostic capacity of every suspect case.• Prevention and control measures in primary care.• Prevention and control measures in hospitals.• Contingency plans for healthcare surge capacity.• Plans to increase human resources in the immediate future.• Plan to recover non-COVID clinical activity.• Essential materials stocks monitoring system. | • Number of cases under domiciliary follow-up.• Proportion of general ward & ICU hospital beds occupied in total and by COVID-19 patients.• Number (and rate) of healthcare professionals, including reinforcements introduced since the beginning of the epidemic.• Quantities in stock, days of activity covered and stock rupture in the last 7 days of a list of essential materials. |
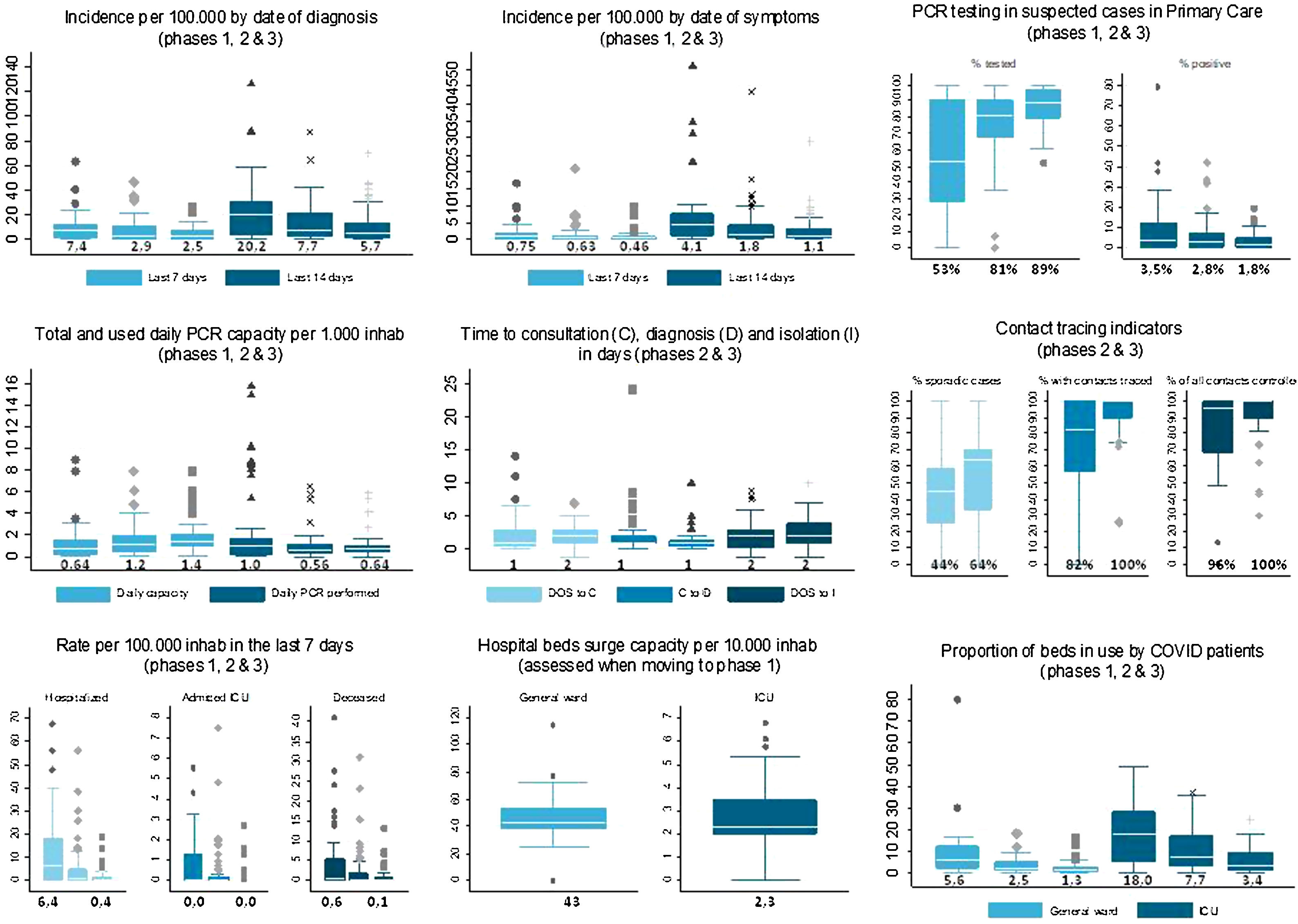
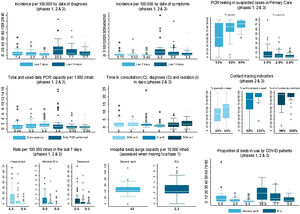
In this article, to summarize the evolution of the different indicators throughout the process, each reference territory has been considered an analysis unit. The distribution of the indicator across the territories at the moment they were approved to progress from one phase to the next has been graphically described using whisker-plots, with the median as the central value and box limits at the interquartile range.
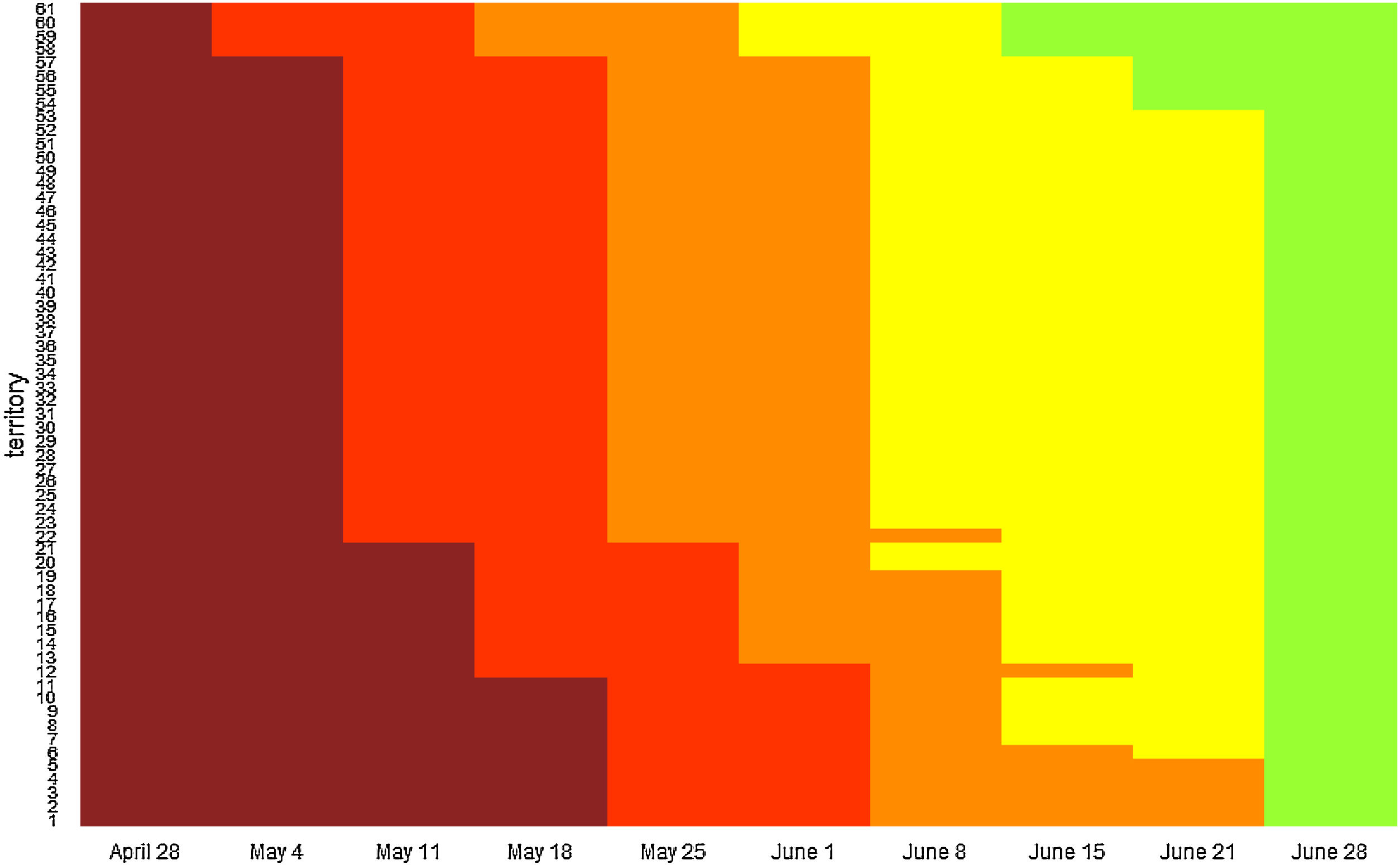
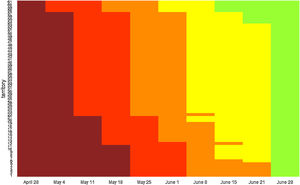
ResultsThe process resulted in the division of Spain into 61 territories (after the regrouping previously explained), with varied administrative delimitations: 6 were sanitary regions (alone or in groups), 12 were islands, 34 were provinces, 7 were complete AC and 2 were autonomous cities. Fig. 1 shows a diagram with the transition of territories through the different phases. The process began on April 28th with the publication of the PTNN, when all territories passed to Phase 0 (preparation), and further on May 4th, with the progression to Phase 1 of Formentera (Islas Baleares), and La Gomera, El Hierro and La Graciosa (Islas Canarias), which had had zero cases diagnosed in the previous 14 days.
Transition of territorial units trough the phases since the beginning of the process on April 28 to the end of the state of alarm on June 21.
Dark red represents dates in which territories were in the preparation phase, red represents time spent in phase 1, orange time spent in phase 2, yellow time spent in phase 3 and green corresponds to the new normality. All territories progressed to new normality on June 21 when the state of alarm ended, regardless the phase achieved. The transition of the specific territories can be found at: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/planDesescalada.htm.
The full process lasted for 8 weeks, during which a total of 215 decisions over territories were made; of them, 190 (88%) were favorable to progression to the next phase. All reports on the decisions to progress to the next phase were made public on real-time.15 The duration of the evaluation process (from the first receipt of the request to the formal decision) had a median of 5 days, with a range of 1–6 days. The process finished on June 21st, when the state of alarm was declared over, and thus restrictions to mobility within Spain ended and physical distancing and other non-pharmaceutical measures were again directly ruled by AC. The territories which remained on Phase 2 by June 21st (AC of Madrid and the provinces of Avila, Salamanca, Segovia and Soria in the AC of Castilla y León) did not maintain mobility restrictions and decided to progress to new normality on that same day.
Fig. 2 shows a summary of key quantitative indicators of the territories at the time of their progression to each Phase. Not all territories provided information for every indicator at every phase. The bilateral efforts to better define the optimal core indicators and adapt the territorial information systems to be able to provide them, increased the availability and quality of the information, which was required as the territories advanced. Decreasing incidence was not a strict requirement to progress from one phase to the next, although it contributed to a favorable decision, and indeed improved from a cumulative incidence of cases diagnosed in the past 7 days of 7.4 (IQR: 1.5–12.5) at progression to phase 1 to a cumulative incidence of 2.4 (IQR: 0.7–7.3) at progression to phase 3. In contrast, an improvement in capacities to reach or come close to the established targets was increasingly important as the territories progressed through the phases. The main focus at all phases was that the capacities installed in the territory needed to be enough to safely cope with estimated degrees of transmission and be enough to ensure adequate detection and response to any increases that may occur in the future. PCR testing in suspected cases in primary care improved from a median (across territories) of 53% (interquartile range, IQR: 28–90) at the moment of progressing to phase 1, to 89% (IQR: 79–96) at phase 3; positivity rate decreased from 3.5% (IQR: 0.6–12) to 1.8% (IQR: 0.3–5.0). As a key indicator, the proportion of cases with contact tracing performed increased from 79% (IQR: 56–100) at the moment of progressing to phase 2, to 100% (IQR: 89–100) at phase 3.
Key indicators and their evolution along the progression of the territories to each phase. Numbers represent the median for each indicator at each phase. Box plots show the median across territories, percentiles 25 and 75, for selected indicators. Each graph contains a set of related indicators. Boxes of similar color within a graph represent the same indicator in successive phases of lifting of control measures, as indicated in the title for each graph between brackets. Boxes of different colors within a graph show different indicators, as indicated in the graph legend. DOS: Date of onset of symptoms.
In summary, a step-wise approach tailored to local contexts and founded on technical advice and a set of core capacities indicators was used in Spain to progressively lift the restrictions that had been implemented in response to the COVID-19 epidemic on mid-March 2020. This was especially challenging in a highly decentralized system such as Spain and under a State of Alarm. In this regard, this process was an innovative experience in our context with regards to shared responsibilities between the central Government and the regions, territorial collaboration and bilateral technical discussions, that resulted in consensus decisions in the large majority of cases and allowed for a coherent and coordinated process nation-wide. Also, we hypothesized that the gradual process helped raise awareness of the population of the precautions needed in their social interactions in the new normality.
Throughout this process, the epidemiological situation improved notably, with all but one territory having an incidence lower than 50 cases, and 50% having less than 6 cases, per 100,000 in 14 days. Similarly, the pressure on the healthcare system was greatly decreased, with a fall in the number of severe cases requiring hospital and ICU admission, and in the occupancy rates. But mostly, the process entailed an intense development of response capacities, such as PCR testing availability, and achieving confirmatory testing in at least 80% of suspected cases and contact tracing of at least 90% of confirmed cases, in 75% of the territories. Such a rapid increase in capacities nation-wide, with homogenous criteria, would have been difficult outside of this process. However, capacity development did not finalize by the end of the state of alarm; on the contrary, all territories were advised to maintain and further strengthen core capacities.
The capacities at the centre of the deconfinement process in Spain have been acknowledged as pivotal to minimize the risk of resurgence by the World Health Organization and the European Commission,5,9,10 which also recommended that lifting restrictions was data-driven and incremental. Many other countries experienced similar processes that coincided in time with Spain, chose similar phased approaches, frequently with two-weeks intervals between phases, and faced shared challenges.6,12,16–18 Capacities achieved in Spain were comparable to those in other countries under similar circumstances.12 A notable difference is that some countries did establish fix thresholds for indicators while in Spain it was allowed that indicators were modulated by qualitative information and context-specific interpretation. For example, where incidence rate could be apparently high, but was mostly related to delimited outbreaks, the risk of onwards community transmission was deemed lower than initially assessed by incidence itself. This detailed assessment could be perceived as discretionary but allowed more accurate risk evaluation.
The increased detection and contact tracing capacities in all AC, allowed for early detection of a much higher proportion of infected individuals than it was possible during the first epidemic wave, and for early isolation of infected people even before the onset of symptoms, reducing their capacity of infecting others. Still, lifting restrictions to mobility at the start of the holiday season was a major challenge for the capacities of the National Health System, as was evidenced by an earlier beginning of the second wave in Spain.19 Subsequent resurgence of transmission in most European countries by September and October 2020 shows that the test, trace and isolate strategy was still insufficient to suppress transmission in the absence of considerable physical distancing measures,20 which has led many countries to implement different degrees of restrictions to contain subsequent COVID-19 waves. The epidemic control in Spain includes, since October,21 the establishment of very sensitive thresholds for rapid decision and implementation of control measures by the AC. The challenge remains to maintain the balance between the social and economic activity and the application of physical distancing and individual protection measures, and to ensure continued risk communication to keep the population engaged and compliant with the recommendations.
Regarding limitations of this study, it uses territories as the analysis unit; therefore, it cannot be used to assess the overall epidemiological situation in Spain, since the size of the different territories would need to be taken into account to draw pooled figures. Importantly, this is an exercise carried out by the appointed focal points that were directly involved in the process, and therefore cannot be interpreted as an external objective evaluation of the process itself. Nevertheless, it may contribute to knowledge sharing and contribute lessons learnt for future similar situations.
As reflections around the limitations of the process itself, it was conceived, organized and carried out with limited available time, as is the case in response to emergency situations. This resulted in a certain degree of heterogeneity in the process for the different territories, driven both by the specificities of the different AC and the reach of the homogenization efforts carried out at the National level; this heterogeneity improved as the process advanced and a good level of standardized, data-driven decision-making was achieved. Also, the relative weight given to the different indicators varied along the process, with more emphasis on full implementation of the test, trace and isolate strategy in the latter phases. Input from non-health sectors and information on other dimensions were brought up during the discussions but could not be systematically incorporated into the technical assessment; for example, analyses of population mobility and use of public transportation, effective availability of masks for the population with a focus on vulnerable groups, or general adherence to existing recommendations. Finally, the whole process was surrounded by heavy media attention, and a more proactive public communication about the process itself and the technical criteria that were being used could have increased community engagement with the process and limited a certain degree of speculation and mistrust that arose in some sectors of the public opinion.
ContributionsSM, PL, BS and FS coordinated the data collection for the purpose of this manuscript. SM and PL produced the first draft under the supervision of BS and FS. All authors made part of the process presented here, collected and analyzed relevant data, and critically reviewed the content of the manuscript.
FundingThis work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestJMC is founder-partner and researcher at APLICA Investigación y Traslación, a company contracted by the Ministry of Health. All other authors declare no conflicts of interest other than their institutional affiliation to the public health administration.