Pneumonitis due to C. trachomatis is one of the most common causes of afebrile pneumonia in early childhood, occurring between the 3rd and 12th week postpartum. Patients present with a runny nose and cough that progressively worsen.1,2 This subtle clinical picture frequently leads to delayed diagnosis, it then being able to evolve into serious forms, and become complicated with apnoea pauses. It is a disease that requires high clinical suspicion, and therefore we consider it of interest to describe the typical form of presentation with the aim of facilitating the diagnostic keys that allow for its detection.
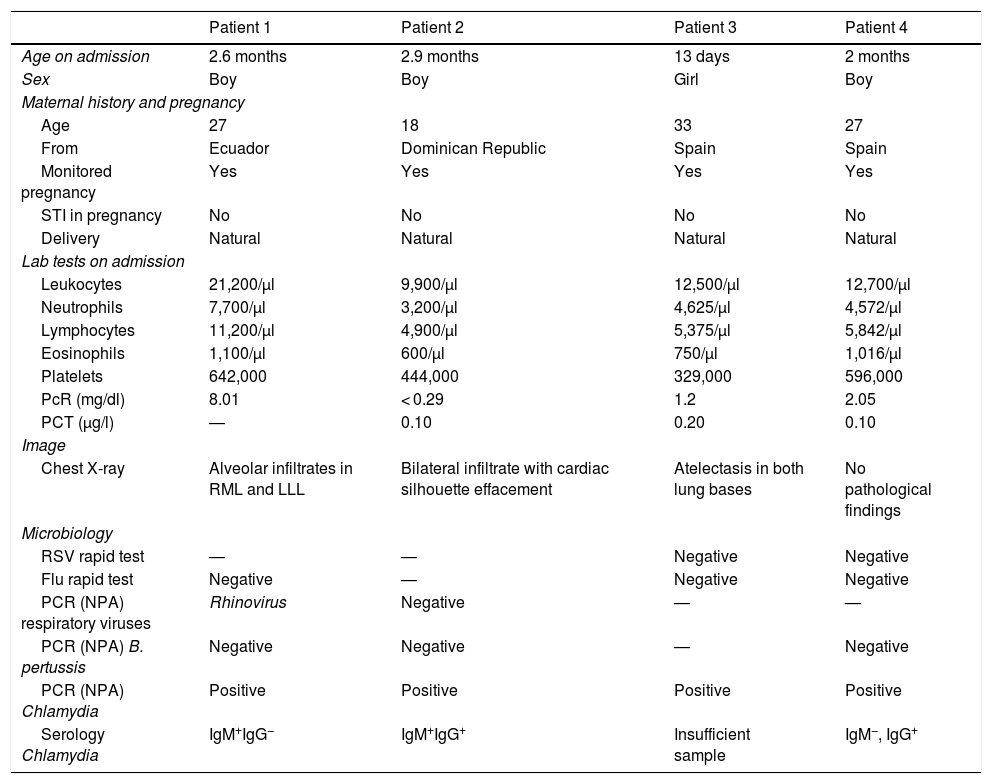
We describe 4 cases of patients admitted with pneumonitis due to C. trachomatis. The epidemiological characteristics are collected in Table 1. Note that they were young mothers, with no record of sexually transmitted disease.
Epidemiological characteristics and summary of additional tests.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
|---|---|---|---|---|
| Age on admission | 2.6 months | 2.9 months | 13 days | 2 months |
| Sex | Boy | Boy | Girl | Boy |
| Maternal history and pregnancy | ||||
| Age | 27 | 18 | 33 | 27 |
| From | Ecuador | Dominican Republic | Spain | Spain |
| Monitored pregnancy | Yes | Yes | Yes | Yes |
| STI in pregnancy | No | No | No | No |
| Delivery | Natural | Natural | Natural | Natural |
| Lab tests on admission | ||||
| Leukocytes | 21,200/µl | 9,900/µl | 12,500/µl | 12,700/µl |
| Neutrophils | 7,700/µl | 3,200/µl | 4,625/µl | 4,572/µl |
| Lymphocytes | 11,200/µl | 4,900/µl | 5,375/µl | 5,842/µl |
| Eosinophils | 1,100/µl | 600/µl | 750/µl | 1,016/µl |
| Platelets | 642,000 | 444,000 | 329,000 | 596,000 |
| PcR (mg/dl) | 8.01 | < 0.29 | 1.2 | 2.05 |
| PCT (µg/l) | — | 0.10 | 0.20 | 0.10 |
| Image | ||||
| Chest X-ray | Alveolar infiltrates in RML and LLL | Bilateral infiltrate with cardiac silhouette effacement | Atelectasis in both lung bases | No pathological findings |
| Microbiology | ||||
| RSV rapid test | — | — | Negative | Negative |
| Flu rapid test | Negative | — | Negative | Negative |
| PCR (NPA) respiratory viruses | Rhinovirus | Negative | — | — |
| PCR (NPA) B. pertussis | Negative | Negative | — | Negative |
| PCR (NPA) Chlamydia | Positive | Positive | Positive | Positive |
| Serology Chlamydia | IgM+IgG− | IgM+IgG+ | Insufficient sample | IgM−, IgG+ |
NPA: nasopharyngeal aspirate: STI: sexually transmitted infection; LLL: left lower lobe; RML: right middle lobe; PcR: C-reactive protein; PCR: polymerase chain reaction; PCT: procalcitonin; IQR: interquartile range; RSV: respiratory syncytial virus.
All presented with runny nose in previous days and respiratory distress, 3/4 patients presented with cough; one related fever and another conjunctivitis, on diagnosis. None presented with apnoea pauses. Table 1 shows the additional tests on admission, with eosinophilia in all infants. Gene amplification was performed in all cases in nasopharyngeal aspirate, with 4/4 positive, thus confirming infection by C. trachomatis. During admission all received treatment with oral azithromycin for 5 days and required respiratory support with nasal cannula for hypoxaemia or respiratory distress, with one of them requiring high flow oxygen therapy. Median hospital stay was 6.5 days, all evolving favourably and without subsequent complications.
The incidence of pneumonitis due to C. trachomatis in infants is unknown, but given the scarce symptomatology that it produces in the pregnant woman (it is the most frequent sexually transmitted infection in our country)3 and the subtle clinical picture presented by the infant, it is probably an underdiagnosed entity.
Our patients had a median age at diagnosis of 2.3 months, similar to published data.4,5 Fever was not a common symptom in these patients, who normally consult for mucus and bouts of cough, with progressive worsening and onset of respiratory distress.6,7 This clinical presentation, typical of a pertusoid picture, justifies the request for microbiological study to rule out infection by B. pertussis, whooping cough being one of the main differential diagnoses. Rapid diagnostic tests for RSV and flu virus were also performed, as well as PCR of other respiratory viruses, only detecting rhinovirus in one patient, this case being considered a coinfection by both agents.
Eosinophilia is one of the main diagnostic keys of this entity. In our cases, all presented with moderate eosinophilia (600-1,100 eosinophils/µl). To confirm infection by C. trachomatis genomic amplification techniques were performed which are approved to be carried out on vaginal, endocervical, urine and urethral samples. In our population the results came from nasopharyngeal samples, whose use is not validated by the FDA, but whose result, interpreted together with the patient's clinical picture and, when possible, with the serological results, would allow for the establishment of the aetiological diagnosis of the infection.
Although we present a limited number of patients, it is useful to highlight the characteristics of this entity, which is potentially serious, and which must be one of the main diagnostic suspicions in infants admitted with lower respiratory tract infections, where microbiological isolation from other species is not obtained and they present with eosinophilia, as well as compatible epidemiological factors.
FundingThe authors declare that they have not received funding to carry out this work.
To Marta Illán Ramos, of the Paediatric Infectology Department of Hospital Clínico San Carlos [San Carlos Clinical Hospital], for her participation and review of the cases described. To Juan-Ignacio Alós Cortés, Head of the Microbiology Department of Hospital Universitario de Getafe [Getafe University Hospital], for his participation as a microbiologist and his collaboration in the review of the article, and to Ignacio Bonilla Hernández, of the Microbiology Department of Hospital Universitario Clínico San Carlos, for his participation in the microbiology section, as well as a review of the article.
Please cite this article as: Berzosa Sánchez A, Kirchschläger Nieto SB, Ruiz Jimenez M, Ramos Amador JT. Infección respiratoria por Chlamydia trachomatis, a propósito de 4 casos. Enferm Infecc Microbiol Clin. 2020;38:454–455.