The evolution of syphilis after treatment could be affected by different factors, for example HIV. In consequence, HIV positive patients are sometimes treated with more doses of penicillin (PBG).
The aim of the study is to describe and compare the serological evolution by different factors in patients with early syphilis in Barcelona.
MethodsThe serological control was made over the following year. A time analysis was performed through the study of Kaplan–Meier curves.
ResultsThe serological control was made in 208 patients, 42.5% of whom were HIV-positive. In a Kaplan–Meier curve the median of days needed to observe the cure was 99 [97–105] without differences depending on HIV, previous syphilis, stage or RPR titters. A better evolution was observed in patients treated with doxycycline p=0.02.
ConclusionsThe serological evolution is similar in HIV-negative and HIV-positive patients treated according to current recommendations, observing the cure at 3 month after treatment.
La evolución serológica de la sífilis se puede ver influenciada por diferentes factores, entre ellos el VIH. Por este motivo en ocasiones los pacientes positivos para el VIH reciben mayor número de dosis de penicilina (PBG).
El objetivo del estudio es describir y comparar la evolución serológica según diferentes factores en pacientes con sífilis precoz en Barcelona.
MétodosEl seguimiento serológico se realizó durante 12 meses. El análisis de la evolución hasta el criterio de curación se realizó mediante curvas de Kaplan–Meier.
ResultadosDe los 208 pacientes incluidos el 97,5% eran HSH y el 42,5% VIH-positivos. La curación se observó a los 99 días de mediana (97–134), sin diferencias según VIH, estadio, títulos de RPR o sífilis previa. Se observó mejor evolución en los pacientes tratados con doxiciclina p=0,021.
ConclusionesLa evolución serológica es similar tanto en pacientes VIH-positivos como en VIH-negativos tratados según las recomendaciones actuales, objetivándose la curación a los 3 meses del tratamiento.
Syphilis is an infection currently on the increase in a number of Western countries, including Spain, particularly among men who have sex with men. Despite epidemiological changes observed over the last few decades, there has been little change in the way it is managed.
From a microbiological point of view, new automated treponemal tests are available which provide good specificity and sensitivity.1 However, the same advances have not been made in the reagin tests; the Rapid Plasma Reagin (RPR) and the Venereal Diseases Research Laboratory tests have been used since the mid-20th century. The serological response pattern of the syphilis is based on these tests, determining adequate response to treatment or the diagnosis of possible re-infections.2 Cure is defined as a decrease by two dilutions in non-treponemal test titres in the 6–12 months following treatment. It is therefore important to have the serology results at the time of diagnosis and to perform serology follow-up after treatment.2
A number of different factors may affect the serological response pattern, such as age, gender, stage, history of syphilis and the RPR titre at the time of diagnosis.3–9 HIV-positive patients have been found to have a slower serological response,10 and a greater likelihood of treatment failure.11 On the basis of these studies, three doses of penicillin benzathine have been given to HIV-positive patients with secondary syphilis,7 and that trend still continues today in some places,12 even though the clinical guidelines no longer recommend it.13
The aim of this study was to describe the serological response pattern in patients diagnosed with early syphilis in Barcelona, and to compare the pattern according to HIV serostatus after receiving the same treatment, extending the study to other factors.
MethodsThis was a prospective, observational study conducted at Vall d’Hebron-Drassanes Sexually Transmitted Infections Unit. Participation in the study was offered to patients seen in the unit from January to October 2015 diagnosed with early syphilis. After they agreed to join the study, they had serological follow-up prospectively for 12 months after treatment. The exclusion criterion was being under 18 years of age.
The diagnosis of early syphilis was based on the European guidelines on syphilis,13 classifying it as primary or secondary syphilis or early latent syphilis after clinical and serological assessment using treponemal tests and non-treponemal tests such as the RPR test (Biokit, Spain). In patients with a history of syphilis, only the RPR test was performed. To monitor the serological response, follow-up was carried out at 3, 6 and 12 months in HIV-negative patients and at 1, 3, 6, 9 and 12 months in HIV-positive patients. One month was defined as 20–60 days from diagnosis, 3 months as 60–150 days, 6 months as 150–240 days, 9 months as 240–330 days and 12 months as 330–444 days. Patients who failed to attend for follow-up at least twice were contacted at 6 and 12 months.
An appropriate response pattern was defined as the RPR becoming negative if the initial titre was <1/4 or a decrease of 2 dilutions in the RPR titre at 12 months after treatment. Patients with negative RPR at the time of diagnosis were not taken into account when conducting the study.
Qualitative variables were described as frequencies and percentages. Mean and standard deviation or median and interquartile range were calculated for quantitative variables. To assess the patients’ cure time, a survival analysis was performed and the Kaplan–Meier curves were plotted and compared with the log-rank test. The statistical analysis was carried out using the R programme version 3.4.1 (The R Foundation for Statistical Computing programme, Vienna, Austria).
The study was approved by Hospital Vall d’Hebron Ethics Committee. Signed informed consent was requested for participation in the study, including a specific section providing permission to contact them in case they did not attend the follow-up.
ResultsOf the 274 cases with early syphilis diagnosed during the study, serological follow-up was performed in 208: 46 (17.2%) did not attend follow-up, and in 20 the initial RPR was negative.
Of the 208 patients, 202 (97.5%) were men who had sex with men, with a median age of 36 (31–44 years); 47.3% had a history of syphilis and 42.5% (88/207) were HIV-positive, with 87% on antiretroviral therapy (ART) with a median CD4 count of 623 [508; 815]. More than half (57%) were diagnosed with secondary syphilis, followed by primary syphilis (22.7%) and early latent syphilis (20.3%). The median of the RPR titres was 1/32 [1/16; 1/64].
The majority of patients (93%) were treated with one dose of penicillin; only 11 (6%) were treated with doxycycline. The remaining 1% received three doses of penicillin with preliminary diagnostic impression of undetermined latent syphilis which, after the microbiological results and the clinical progress, was diagnosed as early syphilis.
After a year of follow-up, 14 patients did not achieve decrease by two dilutions in the RPR titres: two were diagnosed with re-infection; ten did not attend the 12-month follow-up; and two were found to have sero-resistance.
Comparing the changes in RPR in HIV-positive and HIV-negative patients, no significant differences were found in either group after one year. However, cure was detected earlier in HIV-negative patients; 96.5% of patients who attended the three-month follow-up already met the cure criteria, while that figure was 84.4% in HIV-positive patients (p=0.031). The difference had disappeared at six months.
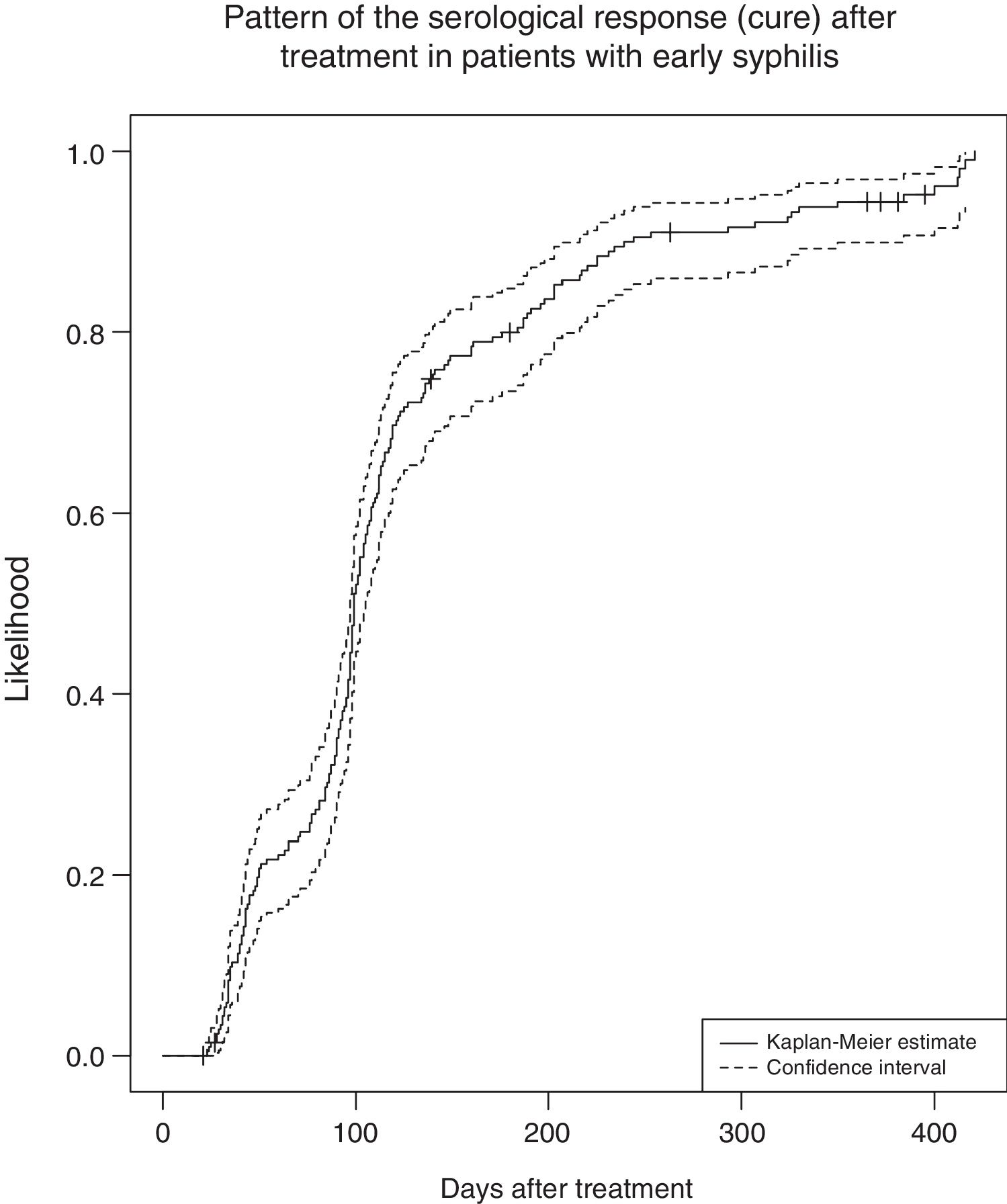
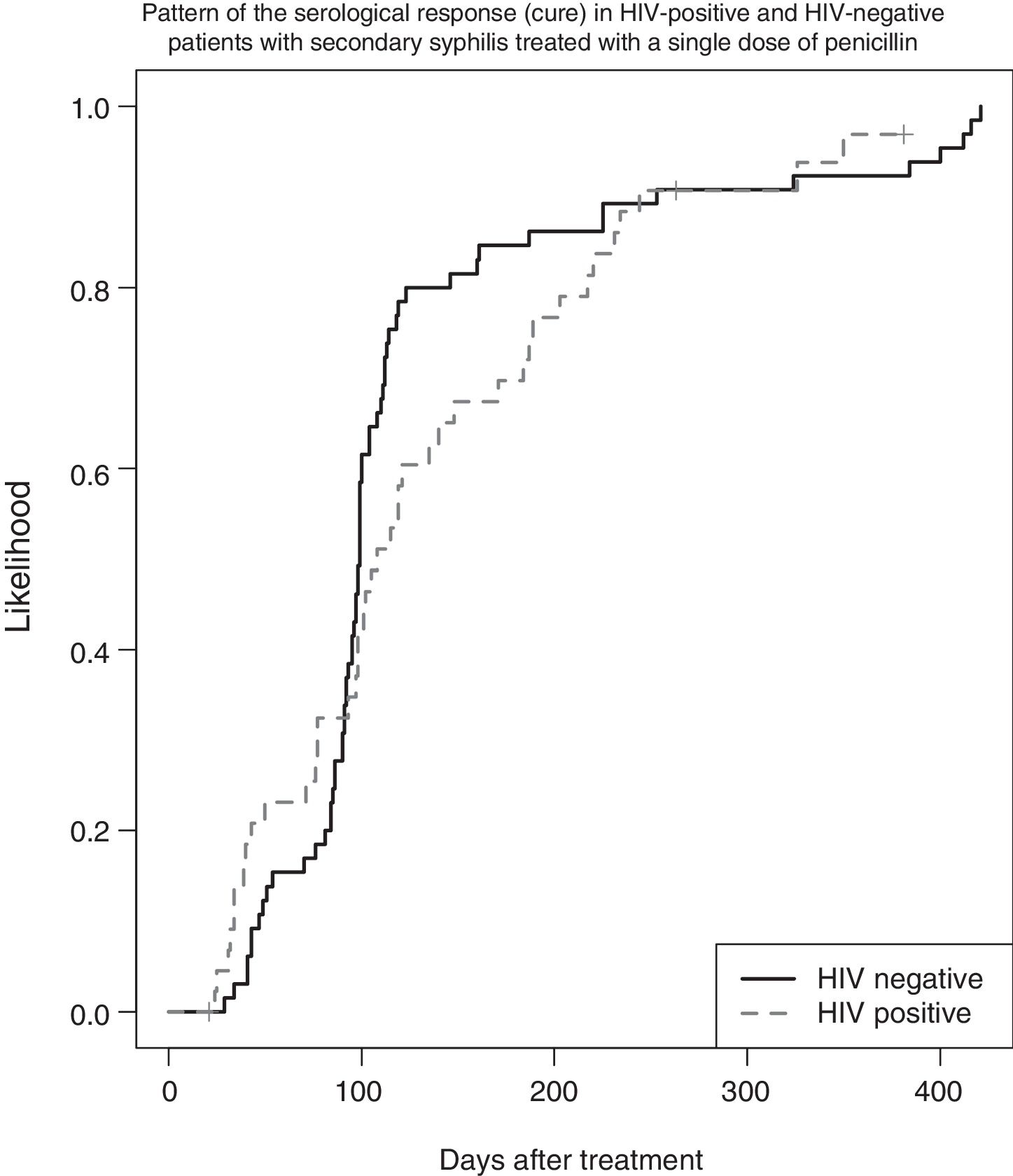
To extend the study, the serological response pattern of all patients was analysed using a Kaplan–Meier curve (Fig. 1). Cure was observed at a median of 99 days (97; 106). When the same analysis was performed according to serostatus, no differences were found: in HIV-positive patients the median was 104 days (97–134), in HIV-negative patients 98 days (96–104, p=0.4). The same analysis on patients with secondary syphilis treated with one dose of penicillin also found no differences (p=0.46) (Fig. 2).
HIV-positive patients were compared according to CD4 count (≥350 vs <350) and whether or not they were on ART, with no differences in either case (p=0.852 and p=0.951, respectively), although the number of patients not on ART was small (only 10).
The same comparative analysis was performed according to other factors such as previous syphilis, RPR titres (RPR≥1/32 vs RPR<1/32) and treatment (penicillin vs doxycycline). Differences were only found in the treatment group, with patients treated with doxycycline having better outcomes than those treated with penicillin; p=0.021.
DiscussionBoth the European and American clinical guidelines advise treating HIV-positive patients in the same way as HIV-negative patients.2,13 Despite that, HIV-positive patients continue to be treated with three doses of penicillin in some places.12 Our study shows that there is no difference in outcome between HIV-positive and HIV-negative patients with secondary syphilis treated with one dose of penicillin. It is important to stress the need for serological follow-up, although this can sometimes be made difficult by the patient's perception of having been cured when the lesions disappear after treatment, and the high degree of mobility between cities and countries meaning that by the time of their appointment, the patient may no longer be in the same place. In HIV-positive patients, the need for follow-up is more important as the decrease in RPR titres can be slower. Gonzalez-Lopez et al.9 found that ART was associated with a better serological response pattern in HIV-positive patients, due to the immunological recovery and the better functioning of B lymphocytes possibly accelerating the decline of the RPR. We found no such association in our study, and nor was there any association according to the CD4 count, partly because of the small number of patients not on ART or with CD4 <350. The fact that ART is now being started when people are diagnosed with HIV may contribute to the influence of this factor having changed.
In our study, the only factor associated with a better serological response pattern was the treatment, but that may have been affected by the limited number of patients treated with doxycycline, as it was only used in patients allergic to penicillin. Other studies have described similar responses in the two groups.5,14,15
ConclusionSerological follow-up in patients diagnosed with syphilis continues to be of paramount importance to assess the response to treatment, facilitate the diagnosis of re-infection and assess for possible sero-resistance (and the consequent risk of asymptomatic neurosyphilis). It is therefore vital that physicians explain and insist on this to patients. The serological response pattern is similar regardless of HIV status, and it is not necessary to treat HIV-positive patients with more doses of penicillin.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Arando M, Mota-Foix M, Armegol P, Barberá MJ, Esperalba J, Vall-Mayans M. La evolución serológica en sífilis precoz. Enferm Infecc Microbiol Clin. 2019;37:183–186.