Sexual violence is a worldwide problem with an impact on health that encompasses medical, legal and psychological aspects. Therefore the management of these patients must be multidisciplinary, and action protocols are compulsory. People who are victims of a sexual assault (SA) are at high risk of acquiring a sexually transmitted infection (STI), which must be prevented, diagnosed, treated and followed up post treatment, according to the established action protocol to prevent potential complications.
La violencia sexual es un problema a nivel mundial con un impacto sobre la salud que engloba aspectos médicos, legales y psicológicos, por lo que el manejo de estos pacientes debe ser multidisciplinar siendo obligado establecer protocolos de actuación. Las personas que son víctimas de agresiones sexuales (AS) tienen un alto riesgo de adquirir infecciones de transmisión sexual (ITS), por lo que se deben prevenir, diagnosticar, tratar y realizar seguimiento postratamiento, según el protocolo de actuación establecido para evitar posibles complicaciones que se pudieran derivar si no se hiciera.
The World Health Organization (WHO) defines sexual violence as “any sexual act, attempt to obtain a sexual act, unwanted sexual comments or advances, or acts to traffic, or otherwise directed, against a person's sexuality using coercion, by any person regardless of their relationship to the victim, in any setting, including but not limited to home and work”.1
Sexual assaults (SAs) include any attack on sexual freedom and sexual indemnity of the other person, carried out with violence or intimidation. This includes rape: where the SA involves vaginal, anal or oral penetration with the penis or the vaginal or anal introduction of any body parts (for example fingers) or objects of any type.2
Sexual abuse also includes any attack on the sexual freedom and sexual indemnity of the other person, carried out without violence or intimidation, but always without the consent of said person.2
Sexual harassment is also a form of sexual violence. It consists of unwanted verbal, non-verbal or physical behaviours of a sexual nature that threaten or are intended to threaten dignity, or create an intimidating, hostile, degrading, humiliating, offensive or unpleasant environment.2
In Spain, crimes against sexual freedom and indemnity are governed by Organic Law 10/1995 of 23 November, of the Criminal Code.
Currently, the age of sexual consent in Spain is 16. For this reason, the performance of sexual acts with minors under 16 years of age is considered to be a crime, except in the case of freely consenting relations between a person close in age, development and maturity to the minor, in which case criminal liability is ruled out (Organic Law 1/2015 of 30 March, amending Organic Law 10/1995 of 23 November, of the Criminal Code).3
Although its true prevalence is unknown, sexual violence is a reality for millions of people, especially women.
In its study “Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence”, published in 2013, the WHO concluded that 35% of women worldwide have been victims of physical and/or sexual violence.4
In Spain, since 2011, a macro-survey has been conducted on violence against women, with the primary objective of finding out the percentage of women resident in Spain who have suffered or are currently suffering some type of violence because they are women. In the latest survey, conducted in 2015, 6.6% of women who have had a partner reported that at least one of the partners during their life had obliged them to have sexual relations when they did not want to.5
Sexual violence in men and boys is also a serious problem. Although it is less common than in women, up to 1.7% of men have been victims of rape, according to data from the National Intimate Partner and Sexual Violence Survey in the United States.6
Studies conducted primarily in developed countries suggest that between 5% and 10% of men have reported having been the victim of sexual abuse in childhood. The majority of experts consider the official statistics to considerably underestimate the number of male rape victims. The evidential data available indicate that the likelihood that a man will report a SA is even lower than for women.4–6
In this review, there is a section on child SA.
Epidemiology of sexually transmitted infections in the context of sexual assaultThe total global prevalence of STIs in the context of sexual assault is unknown. Those most frequently diagnosed are C. trachomatis (CT), N. gonorrhoeae (NG) and T. vaginalis (TV) infections. The STIs included in early detection and prophylaxis protocols for SA are those mentioned, together with human immunodeficiency virus (HIV), hepatitis B virus (HBV) and syphilis infection. According to the prevalence study conducted by Françoise Jauréguy et al., in the period 2012–2013, during which 326 adult SA victims were studied, CT was detected in 15% of those studied, NG in 5% and coinfection in 3%.7 Hagemann CT et al. conducted a study covering the period from July 2003 to December 2010, which included 412 SA victims; 35 had one STI (8.5%), with CT detected in 25 (6.4%).8
Health and social care for adult victims of sexual violenceWhen faced with a situation of sexual violence, a pre-established and coordinated multidisciplinary protocol must be activated, involving different professionals and institutions from the healthcare, judicial, law enforcement and social services sectors, since the consequences on health can be physical, psychological, sexual and/or social.9–11
The sexual assault or abuse may have been2:
- 1.
Recent: when fewer than 120h have elapsed.7 The victim will be assessed in a hospital setting.
- 2.
Not recent: when more than 120h have elapsed.7 It will not be necessary to perform the assessment in a hospital if the victim has attended a health centre. After assessing the patient, the lesions will be recorded where applicable.
This time limit should not be viewed as strict. If the time elapsed is around 120h and there is reason to believe it may be possible to obtain biological samples (for example, in cases of chemical submission12), the sexual assault or abuse should be treated as recent.13
In the medical handling of recent SAs, good coordination with the duty court is essential, in order that the forensic medical examiner, who does not act independently, attend the hospital as soon as possible. This can happen only after the judge handling the case, or the corresponding public prosecution service, has requested an expert report.14 An explicit order to attend the hospital is also required.
In the Emergency Department, the victim should not be made to remain in the waiting room and can be accompanied by a trusted person. They will be told not to wash or change their clothes before the examination, and should also avoid eating and drinking, where possible.13–15
The clinical assessment will be performed by a gynaecologist (if the victim is a woman) or by an emergency department doctor (if the victim is a man), together with the forensic medical examiner. The process must be comprehensive and conducted in an atmosphere that favours communication, always as a single simultaneous and coordinated action, with the aim of reducing as far as possible the psychological blows to the patient following the assault. It will include16:
Medical history and clinical examinationA complete medical history will be obtained, transcribing the facts relating to the assault and the actions performed after it took place and before the examination (personal hygiene, change of clothes, etc.). The genital, anal and perianal area will be explored, describing the existence or otherwise of lesions.
Sexually transmitted infections: collection of genital, extragenital and serology samples and microbiological diagnosisThere are various criteria on whether or not to collect samples for microbiological diagnosis, although the decision to collect genital or extragenital samples, and when to do so, must be made on an individual basis.
If the victim attends a health centre immediately after the SA, there are various options. Various SA programmes in the United States and Canada do not routinely make use of early detection, instead opting for prophylaxis. Others do not collect samples, doing so later only if symptoms appear, do not start prophylaxis, and only start treatment if there are positive cultures.17,18
With regard to SA and STIs, the treatment guidelines of the Centers for Disease Control and Prevention (CDC) focus on identification, prophylaxis and treatment in adults and children,17 recommending early detection and prophylaxis in cases of sexual assault.
A serum sample will be taken immediately to test for HBV (looking for HB surface antigen, HB surface antibodies and HB core total antibodies), syphilis (Treponema pallidum IgG antibodies) and HIV (HIV 1/2 antibodies and p24 antigen, fourth generation tests).17
With regard to the hepatitis C virus (HCV), there are no prevalence studies on SA victims to recommend it for routine early detection as part of the initial evaluation, and its consideration should be based on risk factors.19–21 The Common Protocol for Healthcare Action on Gender-based Violence, 2012, Ministry of Health, Social Services and Equality, does include HCV detection.2
The samples must be taken from the site of the assault:
- -
Vaginal exudate: A vaginal speculum should be used without lubricants. The sample should be taken from the area with the most fluid or from the vaginal fornix. In women who have had a hysterectomy, it should be taken from the posterior fornix.
- -
Endocervical exudate: If there is endocervical mucus, this must first be cleaned away using a dry swab or dressing and disposed of. A swab should then be rotated in the cervical canal to obtain cells.
- -
Urethral exudate: The swab is introduced to a depth of 2cm with a turning motion. Calcium alginate or dacron swabs with a wire shaft are used, with Amies Stuart transport medium.
- -
Anal exudate: The swab is introduced to a depth of 3cm and rotated for 10s.
- -
Pharyngeal exudate: The sample is taken from the posterior pharynx with the help of a tongue depressor.
- -
Urine: Spontaneous urination, obtaining 10ml of urine from the initial portion.
- -
Ulcers: A sample for viral culture or nucleic acid amplification tests (NAATs) should be taken by scraping the base of the lesion to obtain cells. If there are blisters, it will be necessary to burst the blister and collect the sample from its base. If there is scabby area, lift the scab with a sterile needle, wet the swab with physiological serum and scrape the base.22
The swabs indicated by the reference microbiology laboratory should be used for both cultures and NAATs for the diagnosis of NG, CT and TV.
Until 2014, cultures were the only accepted technique for microbiological diagnosis in the context of SA. In 2015, the CDC included the use of NAATs for the diagnosis of NG and CT infection in genital and extragenital (pharyngeal and anal) sites and TV in the diagnosis of STIs associated with SA.17,18
Sexually transmitted infections: prophylaxis(a) Antibiotic prophylaxis of gonorrhoea, chlamydia and trichomoniasis. The recommended regimens are: Intramuscular ceftriaxone 500mg plus oral azithromycin 1g and oral tinidazole 2g. All are administered in a single dose. In those allergic to beta-lactams, oral azithromycin 2g plus oral tinidazole 2g are administered in a single dose. If the woman is pregnant, a single dose of oral metronidazole 2g is used instead of tinidazole.20–23
(b) Post-exposure prophylaxis (PEP) for HIV. SA is a significant public health problem that leaves victims at risk of contracting HIV infection, so prophylactic HIV-prevention treatment must be included.17 It is generally accompanied by multiple factors that increase the risk of HIV transmission if the attacker is infected. Studies of SA, such as that conducted by Grossin et al., show a significant incidence of anogenital trauma, which is the highest-risk practice for sexual transmission of HIV (20–85%).24 In a prospective study of 1.076 people with SA, 20% had been attacked by multiple attackers, 39% had been assaulted by strangers, 17% had had anal penetration and 83% of the women had been penetrated vaginally. Genital trauma was documented in 53% of the victims, and sperm or semen were detected in 48%.25 The risk is even greater if the prevalence of HIV infection in the attacker is perceived as higher than in the general population (intravenous drug use (IVDU), men who have sex with men (MSM) or those from areas with a high prevalence of HIV infection). The study by Digiovanni C, Berlin F, Casterella P, et al. examined the prevalence of HIV infection among sexual offenders, 1% of men convicted of sexual assault in Rhode Island were infected with HIV on entering prison, in comparison with 0.3% of the male population in general.26 An absence of visible trauma does not indicate that a SA has not occurred; microabrasions and haematomas are common although the appearance of these manifestations after a SA may be delayed. Oral trauma can also occur, and finally, bite marks or bruising inflicted during the SA are also indications for prophylaxis if there is the possibility of contact with the blood, semen or vaginal fluids of the presumed attacker.
Although it is difficult to measure the efficacy of PEP, studies in primates have demonstrated that PEP could be effective in humans if started ≤72h after the contact and continued daily for 28 days. In a systematic review and meta-analysis of 25 studies in non-human primates, the use of PEP was associated with an 89% lower risk of seroconversion compared to not using PEP. Moreover, the use of tenofovir in comparison with other drugs was associated with a lower probability of seroconversion.27
In general, there are different levels of risk of transmission in non-occupational PEP. In the event of a SA, however, and given the characteristics of the SA, there are guidelines that recommend PEP for all victims.28 In any case, it must be recommended when there has been significant exposure, defined as direct contact of the vagina, penis, anus or mouth with the semen, vaginal fluids or blood of the presumed attacker, with or without physical lesions, visible tissue damage or the presence of blood at the site of the assault. It must also be offered in cases where the damaged skin or mucosa of the victim has been in contact with the blood, semen or vaginal fluids of the presumed attacker, and in cases of bite marks with visible blood.29
All patients who start PEP after potential exposure to HIV must undergo an HIV detection test performed on a blood sample at the start of the study (before starting PEP), preferably using a rapid serologic test. Non-blood-based tests are not recommended. Patients with a baseline analysis indicating pre-existing HIV infection should not start PEP or should discontinue it if it has already been started, and receive an urgent referral to a reference Infectious Diseases department. For patients whose rapid HIV test results indicate no HIV infection, or where none are available, PEP must be recommended. The start of prophylaxis must not be delayed while awaiting the results of a baseline HIV test. HIV serology should be repeated at 4–6 weeks and 3 months after the exposure to determine whether infection has occurred.30
In addition, anyone who has suffered accidental exposure to HIV must be informed of the signs and/or symptoms of acute HIV infection. In such cases, an HIV viral load test will be performed, regardless of the time elapsed since the SA.
Patients who start PEP will be informed of the side effects of the antiretroviral treatment, possible drug interactions and the need for good adherence to the treatment.31
Pharmacological PEP treatment: treatment for 28 days is recommended. PEP is effective if started in the first 72h after a SA, and is most effective in the first two hours after the possible exposure, so its start must not be delayed.
There is no solid evidence based on randomised clinical trials that any specific combination of antiretroviral drugs (ARDs) is optimal for use as PEP. For this reason, and because observational studies have shown that adherence to PEP regimens is often poor, particularly among SA victims, regimens that facilitate adherence should be used.32,33 Adherence to ARDs can be facilitated by: (1) prescribing medications with fewer side effects, fewer doses per day and fewer tablets per dose; (2) informing the patient of the possible side effects of the specific ARDs indicated and providing measures or medications to help should side effects occur; (3) helping patients to incorporate the doses into their daily routine; and (4) providing a quick and easy way to contact the reference doctor during the period of prophylaxis.
There is some debate surrounding the administration of ARDs as a starter pack (doses for 3–5 days) or treatment for the full 28 days; although providing the full treatment appears to lead to better adherence and prophylaxis completion rates, it also presents some disadvantages, in particular of a logistical nature and, according to some authors, use of a starter pack leads to better adherence in terms of second visits to specialist consultations, at which the victim is in a better state of mind and more able to understand the information given to them.34
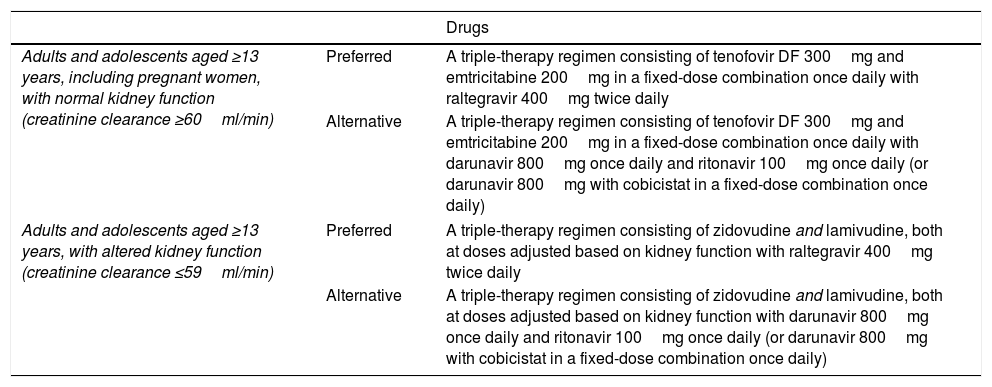
The recommended ARDs are shown in Table 1.
Recommended antiretroviral treatment regimens for post-exposure prophylaxis.
| Drugs | ||
|---|---|---|
| Adults and adolescents aged ≥13 years, including pregnant women, with normal kidney function (creatinine clearance ≥60ml/min) | Preferred | A triple-therapy regimen consisting of tenofovir DF 300mg and emtricitabine 200mg in a fixed-dose combination once daily with raltegravir 400mg twice daily |
| Alternative | A triple-therapy regimen consisting of tenofovir DF 300mg and emtricitabine 200mg in a fixed-dose combination once daily with darunavir 800mg once daily and ritonavir 100mg once daily (or darunavir 800mg with cobicistat in a fixed-dose combination once daily) | |
| Adults and adolescents aged ≥13 years, with altered kidney function (creatinine clearance ≤59ml/min) | Preferred | A triple-therapy regimen consisting of zidovudine and lamivudine, both at doses adjusted based on kidney function with raltegravir 400mg twice daily |
| Alternative | A triple-therapy regimen consisting of zidovudine and lamivudine, both at doses adjusted based on kidney function with darunavir 800mg once daily and ritonavir 100mg once daily (or darunavir 800mg with cobicistat in a fixed-dose combination once daily) | |
Note 1: Some guidelines include dolutegravir (50mg once daily) instead of raltegravir, but in May 2018 the FDA and EMA issued a warning about the possibility of neural tube defects in children born to mothers treated with dolutegravir during pregnancy. For this reason, in principle, its use is not advisable in non-pregnant women of childbearing age who have been sexually assaulted and are not using an effective method of birth control, and pregnant women in early pregnancy, as the risk of a foetus developing a neural tube defect is greatest in the first 28 days. Source: Centers for Disease Control and Prevention. Interim statement regarding potential fetal harm from exposure to dolutegravir–implications for HIV post-exposure prophylaxis (PEP). Statement. 23 May 2018.
Note 2: Although a new dosage form of raltegravir is available (600mg; 2 tablets taken together once daily), there is not yet sufficient data to be able to recommend its use for PEP.
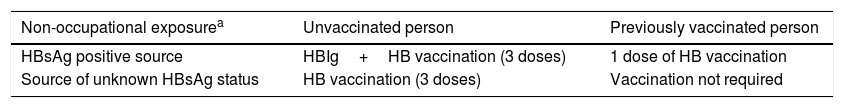
(c) Regarding post-exposure HBV vaccination: the CDC recommend vaccination in previously unvaccinated patients, without administration of gamma globulin, if the vaccination status of the attacker is unknown. If the attacker has HBV surface antigen, vaccination with gamma globulin is recommended in previously unvaccinated patients. Vaccination should be started during the initial assessment and completed according to the vaccine schedule. In vaccinated patients, the medical record must be checked to ensure complete vaccination against HBV and they will not be vaccinated (Table 2).35
HBV vaccination.
| Non-occupational exposurea | Unvaccinated person | Previously vaccinated person |
|---|---|---|
| HBsAg positive source | HBIg+HB vaccination (3 doses) | 1 dose of HB vaccination |
| Source of unknown HBsAg status | HB vaccination (3 doses) | Vaccination not required |
HB: hepatitis B; HBsAg: hepatitis B surface antigen; HBIg: hepatitis B-specific immunoglobulin.
Exposures include the percutaneous route (e.g. needle puncture or bite), exposure of the mucosa to blood or bodily fluids, sexual contact, sharing needles or victims of sexual abuse.
Source: Vaccines Advisory Committee (CAV-AEP). Hepatitis B. Vaccines manual on the website of the AEP (Spanish Paediatric Association) [online]. Madrid: AEP; Feb/2018.
(d) Regarding HPV vaccination: the CDC recommend starting vaccination after the SA in women (9 to 26 years of age) and men (9 to 21 years of age and up to age 26 for men who have sex with men (MSM)) if they have not been vaccinated or if their vaccination was incomplete. In Spain, the Spanish Association of Cervical Pathology and Colposcopy has not issued recommendations on this subject.36
(e) Regarding other STIs: There are no recommendations for prophylaxis in the context of SA.
Collecting samples of legal interestMedico-legal studies are conducted under the instruction of the forensic medical examiner, who will decide which samples to collect: the patient's clothes, pubic hair, fingernail scrapings, vaginal samples to test for sperm, etc., and will take custody of the samples and produce the forensic medical report for the court.37
Treatment of possible physical and psychiatric injuriesIn emergency medical situations, and based on severity criteria, this will be the first action to take.
Injuries will be treated and infection prevention measures employed, with tetanus prophylaxis administered, where necessary.
If considered necessary, a psychiatric assessment will be conducted in the emergency department. Medium- to long-term psychological support will be offered.2–17
Emergency contraceptionA pregnancy test will be performed and, if the result is negative, emergency contraception will be prescribed if no more than 120h have elapsed since the assault.
The following will be administered:
- -
Levonorgestrel 1.5mg in a single dose, if the assault took place within the previous 72h.
- -
Ulipristal acetate 30mg in a single dose, if more than 72h have elapsed. Contraindicated in severe asthma.
If the woman is using an effective method of contraception, emergency contraception will not be necessary.38
The woman will be informed, that should a pregnancy occur, she can opt to terminate it in accordance with current legislation.
Follow-up and subsequent managementFollow-up is of utmost importance for SA victims, and everything possible should be done to properly complete it. For this reason, all victims must be offered follow-up in a specialist centre (sexually transmitted diseases and/or infectious diseases department). The first check-up will be in the first 7–15 days after the SA, for clinical assessment and collection of samples if required. If an STI is diagnosed in the pre-prophylaxis samples collected at the hospital, the care should be the same as if it were diagnosed in any other context. Post-treatment follow-up and contact tracing, if applicable, should be performed. Where PEP has been started for HIV, the follow-up appointment must be arranged for a date before the start pack of medication runs out (generally 3 to 5 days), if used, and must be no later than the second week if the treatment is provided in full. Any reference tests not previously performed will be done at this initial appointment, and the review should determine whether the victim wishes to continue the treatment, as well as assessing possible side effects and reinforcing adherence.39 Additionally, during the follow-up period, and above all the first 12 weeks, the exposed person should avoid potential secondary transmission of HIV or other infections, by always using a condom during sexual intercourse, not sharing needles, avoiding pregnancy and blood and semen donations. Such patients will be followed up for 24 weeks.
Clinical and serological monitoring and collection of samples (if required) will take place at 6 weeks, 3 months and 6 months.
Social careIt is very important that the victim receives care and information from the moment when he or she first enters the framework of the legal investigation.
It is essential that the victim receives information on all the resources and services he or she is entitled to (temporary accommodation if necessary, access to psychological support, legal counselling, etc.).
Child sexual abuse and sexually transmitted infectionsChild sexual abuse (CSA) is the imposition of behaviour that is sexual in nature by an adult on a boy or girl, in a context of power asymmetry or inequality, usually through trickery, force, deception or manipulation. Sexual activities imposed by one child on another are also considered to be abuse if the first is considerably older than the victim or uses force, threats or other means of pressure. (Committee on the Rights of the Child, Recommendation No. 13.)
CSA is one of the most severe forms of violence against children and has devastating consequences leading to a wide range of social and health problems.
Its incidence and prevalence are difficult to determine. This class of violence is often hidden, goes undetected or is not reported. The various studies carried out have had similar findings: between 10% and 20% of the Spanish population suffered some type of sexual abuse in childhood.40
Between September 2011 and September 2012, the Spanish Society of Paediatric Emergency Medicine's abuse and risk situations working group recorded 177 cases of child sexual abuse, representing 37.6% of suspected abuse cases in the emergency departments analysed (some 3.4 cases per 10,000 visits by under 15s).41
The handling of CSA is one of the greatest challenges healthcare professionals can face. The approach must be multidisciplinary and the reference person must work in paediatrics. The guiding principle at all times must be the interest of the child.
Diagnosis is based on the medical record, physical examination and additional tests. The medical record is essential, as lesions are seldom apparent in the examination (fewer than 10% of corroborated CSA cases), even where there has indeed been abuse. The child's own account is key to the diagnosis of CSA.
The doctor must be aware that in the adequate management of such issues, his or her liability is not merely professional and ethical, but also legal. When faced with suspected CSA, the duty court must immediately be notified, and will order the presence of the forensic medical examiner who will examine the child together with the paediatrician and collect the samples that are of legal interest.
It is also always obligatory to inform Social Services, which is the competent body with regard to the protection of minors.
It is advisable to admit the child who has suffered the sexual abuse until the home environment can be ascertained, as in the majority of cases the attacker may be a family member. Never discharge the child if his or her protection is not assured.
In addition to the psychological impact of the situation for minors and those around them, the risk of contracting an STI must be taken into account.
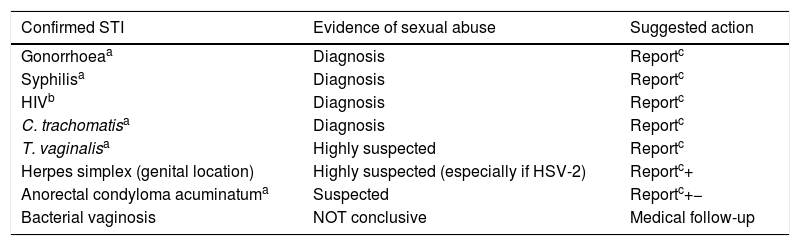
The identification of an STI in a child can have legal significance, as well as implications for treatment. If an STI is detected after the neonatal period, sexual abuse must be ruled out, also taking into account vertical and accidental transmission (Table 3).42,43
Implications in STI diagnosis.
| Confirmed STI | Evidence of sexual abuse | Suggested action |
|---|---|---|
| Gonorrhoeaa | Diagnosis | Reportc |
| Syphilisa | Diagnosis | Reportc |
| HIVb | Diagnosis | Reportc |
| C. trachomatisa | Diagnosis | Reportc |
| T. vaginalisa | Highly suspected | Reportc |
| Herpes simplex (genital location) | Highly suspected (especially if HSV-2) | Reportc+ |
| Anorectal condyloma acuminatuma | Suspected | Reportc+− |
| Bacterial vaginosis | NOT conclusive | Medical follow-up |
+ Rule out self-inoculation; − Report if there is additional evidence of suspected sexual abuse, including from the medical record, physical examination and other infections identified.
The prevalence of STIs in children who have suffered SA depends on the abuse and the prevalence of STIs in the adult.
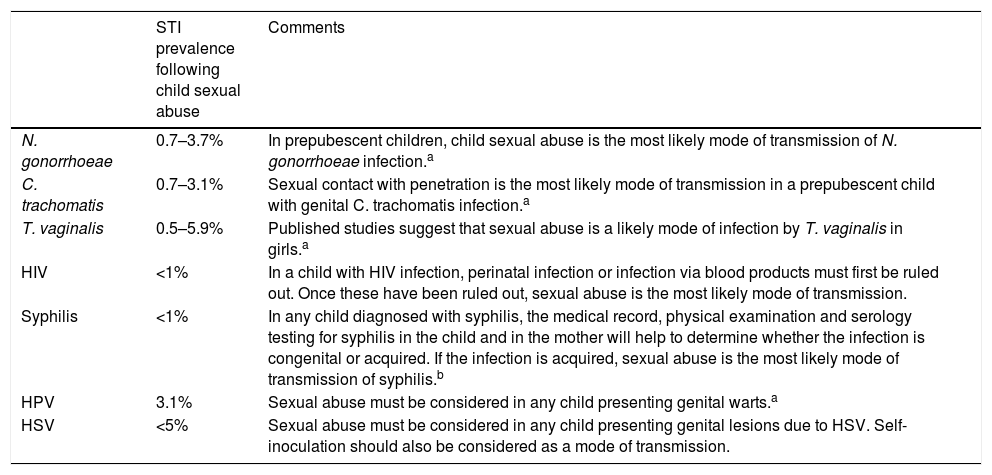
Table 4 shows the association between STIs and sexual abuse in prepubescent children.
STI rate following child sexual abuse.
| STI prevalence following child sexual abuse | Comments | |
|---|---|---|
| N. gonorrhoeae | 0.7–3.7% | In prepubescent children, child sexual abuse is the most likely mode of transmission of N. gonorrhoeae infection.a |
| C. trachomatis | 0.7–3.1% | Sexual contact with penetration is the most likely mode of transmission in a prepubescent child with genital C. trachomatis infection.a |
| T. vaginalis | 0.5–5.9% | Published studies suggest that sexual abuse is a likely mode of infection by T. vaginalis in girls.a |
| HIV | <1% | In a child with HIV infection, perinatal infection or infection via blood products must first be ruled out. Once these have been ruled out, sexual abuse is the most likely mode of transmission. |
| Syphilis | <1% | In any child diagnosed with syphilis, the medical record, physical examination and serology testing for syphilis in the child and in the mother will help to determine whether the infection is congenital or acquired. If the infection is acquired, sexual abuse is the most likely mode of transmission of syphilis.b |
| HPV | 3.1% | Sexual abuse must be considered in any child presenting genital warts.a |
| HSV | <5% | Sexual abuse must be considered in any child presenting genital lesions due to HSV. Self-inoculation should also be considered as a mode of transmission. |
However, the exact age at which the possibility of vertical transmission can be ruled out is not known.
Transmission via blood products must also be ruled out.
Source: Consensus document on diagnosis and treatment of sexually transmitted infections in adults, children and adolescents.20
The steps to take when caring for a minor who has been the victim of CSA are contained in several specific action protocols due to the complexity and distinctive nature of the care of underage abuse victims.
Regarding the management of STIs, the protocol to follow is comparable to that in adults.
Sexually transmitted infections: collection of genital, extragenital and serology samples and microbiological diagnosisAccording to the CDC, routine early detection of all STIs in all sites in asymptomatic children is not recommended, although each case should be assessed individually and it is recommended in:
- •
Minors who have suffered penetration or have evidence of a penetrating injury in the genital, anal or oropharyngeal region.
- •
Minors who have been abused by a stranger.
- •
Minors who have been abused by somebody with an STI or at high risk of STIs (IVDU, MSM or somebody with multiple partners).
- •
Minors with a sibling or family member in the home with an STI.
- •
Minors living in an area with a high prevalence of STIs.
- •
Minors with signs and symptoms of an STI.
- •
Minors diagnosed with one STI should be tested for all STIs.
- •
Request for testing/concerns expressed by the patient/family.
If a child presents signs, symptoms or evidence of infection that would suggest an STI, tests must be performed before starting any treatment that might interfere in the diagnosis, due to the legal implication and the psychosocial consequences that could arise from a positive diagnosis. The diagnostic techniques with the highest specificity should be used.
Regarding the collection of samples for the diagnosis of STIs in prepubescent children, vulvar and vaginal samples should be taken in girls for cultures as endocervical samples are not routinely used. In boys with urethral discharge, a sample taken from the urethral meatus can be used instead of a urethral sample. If there has been extragenital aggression, samples are taken in the same manner as for adults.
Regarding STI diagnosis, there is no consensus on the use of NAATs versus culture. In 2006, the CDC recommended the use of NAATs in children with suspected sexual abuse where culture is not possible. If the result is positive, it must be confirmed with an alternative technique. NAATs are accepted in urine and vaginal samples for CT and NG in prepubescent girls. For prepubescent boys, there are no studies backing the use of these techniques in urine samples or extragenital sites. Data on the use of NAATs for TV detection in children are limited, but there is no evidence that it would differ from that in adults.44–49
Serum is collected for serology testing for syphilis, HBV, HCV and HIV.
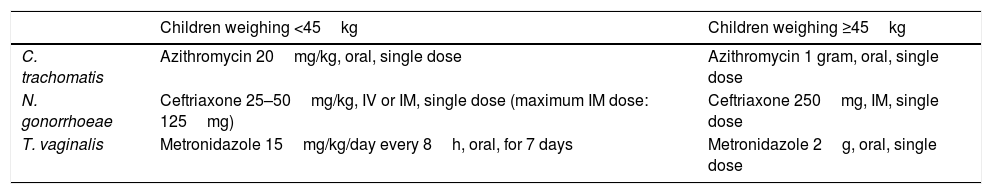
Sexually transmitted infections: prophylaxis(a) Antibiotic prophylaxis of gonorrhoea, chlamydia and trichomoniasis. The recommended regimen is shown in Table 5.
Recommended regimens.
| Children weighing <45kg | Children weighing ≥45kg | |
|---|---|---|
| C. trachomatis | Azithromycin 20mg/kg, oral, single dose | Azithromycin 1 gram, oral, single dose |
| N. gonorrhoeae | Ceftriaxone 25–50mg/kg, IV or IM, single dose (maximum IM dose: 125mg) | Ceftriaxone 250mg, IM, single dose |
| T. vaginalis | Metronidazole 15mg/kg/day every 8h, oral, for 7 days | Metronidazole 2g, oral, single dose |
(b) HIV prophylaxis. This is assessed individually provided that no more than 72hours have elapsed since the SA.
SA increases the risk of viral transmission in children due to their greater anatomical vulnerability to trauma, thinner vaginal and anal mucosa, cervical ectropion, etc. PEP of HIV is recommended in situations of confirmed penetration in both children and adolescents.22
Up to 12 years of age, the regimen to follow is zidovudine (120mg/kg every 8h or 4mg/kg/12h)+emtricitabine (6mg/kg/24h)+lopinavir/ritonavir (230–300mg/kg every 12h).
Preparations of the drugs in solution exist. For older children able to receive full doses (adolescent doses) tablets/capsules may be administered if they are able to swallow them. It is recommended to start post-exposure prophylaxis with these drugs as soon as possible, and always within the first 72h after contact. Prophylaxis should be continued for 28 days. From 13 years of age, the regimen is the same as in adults.
(c) HBV prophylaxis, tetanus prophylaxis, HPV vaccination and emergency contraception: The same regimens as in adults apply.
After discharge, follow-up will be carried out in outpatient paediatric infectious diseases and/or sexually transmitted diseases consultations, with the same process, management and check-ups as in adult patients. The clinical course will be assessed with regard to the suspected sexual abuse and legal proceedings.
ConclusionsSexual violence is a problem on a global scale with sometimes serious health implications that span medical, legal and psychological aspects, and for which care must be multidisciplinary, establishing care protocols that are able to meet the needs of SA victims.
This care must be given regardless of sex, age, race or religious beliefs.
These patients have a high risk of acquiring STIs and, as recommended by the CDC, must receive diagnosis, prophylaxis and treatment.
From our experience with these patients, the management of STIs in the context of a SA is grounded in the collection of samples, microbiological processing, administration of prophylaxis and subsequent microbiological and clinical follow-up. Samples are taken from the site (both genital and extragenital) of the assault and from lesions, if there are any, and this must be done in all cases (prior to antibiotic prophylaxis). Sample collection should not differ based on the subsequent appearance of symptoms, as in many cases STIs can develop asymptomatically, and can also manifest with severe symptoms such as pelvic inflammatory disease. Antibiotic prophylaxis must be started as this is how STIs are prevented and treated.
For microbiological diagnosis, the sampling protocol indicates sending one specific swab for cultures for the diagnosis of NG and TV, and another in the specific transport medium to perform NAATs (NG, CT and TV).
For the diagnosis of NG and TV, culture remains the gold standard, although the use of NAATs increases sensitivity. For CT, culture techniques are no longer in use in Microbiology laboratories, so NAATs are used for diagnosis. Where microbiological confirmation is required, another NAAT with different targets may be used, or the sample may be sent to reference laboratories for culture.
Due to the medico-legal implications that may ensue from a positive result, the samples and isolates must be retained by the microbiology laboratory.
If an STI is diagnosed, the procedure followed is the same as for a diagnosis in any context other than SA, with contact tracing and treatment of contacts.
Medical follow-up is performed in specific consultations until six months after the SA.
If the SA was not recent, early detection tests for STIs should likewise be conducted and follow-up provided in specialist consultations.
Conflicts of interestThe authors declare that they have no conflicts of interests.
Please cite this article as: Hernández Ragpa L, Valladolid Urdangaray A, Ferrero Benéitez OL, Díez Sáez C. Infecciones de transmisión sexual en el contexto de una agresión sexual. Enferm Infecc Microbiol Clin. 2019;37:187–194.