The aim of this study was to determine the effect of oral stimulation on breastfeeding on infants.
MethodThis study uses the design of one group pre-test–post-test. The population was mature neonates aged<14 days who were born without complications at a midwife clinic in Pekanbaru city. The sample consisted of 16 respondents. The sampling technique in this study was purposive sampling with criteria, mothers did not have breast problems and were willing to become respondents. The implementation of intervention was carried out by pre-test, 5min oromuscular stimulation, then a 5-minute pause, then waiting for the next breastfeeding time and post-test. Breastfeeding ability is assessed with Latch score.
ResultsThe results of the univariate analysis showed that the majority of respondents aged 25–35 years (56.3%), the majority were housewife (87.5%), more than half were multiparous (62.5%) and most of the neonates were male (68.8%). The mean of Latch score before the intervention was 7.3 points and after intervention was 9.3 points. The results with the Wilcoxon test showed an increase in the ability of breastfeeding after an intervention of 2 point (p-value=0.001).
ConclusionOromuscular stimulation can be suggested as an alternative therapy to improve breastfeeding ability in neonates.
Parenteral nutrition for the neonate is needed to fulfill the nutritional status of the baby. The requirement for giving oral nutrition to a baby is that the baby has a good suction reflex. Neonates often experience impaired fulfillment of nutritional needs because facial and mouth muscles have not developed, so a stimulation is needed that can stimulate adequate suction reflexes.1–3 Giving oral stimulation has an effect on the suckling process in the neonate. Oral stimulation is defined as a sensory stimulation of the lips, jaw, tongue, palate, pharynx, larynx and respiratory muscles which has an influence on oropharyngeal physiological mechanisms to improve its function.4
Several studies have shown the benefits of giving oral stimulation to the breastfeeding process in premature babies. Based on research conducted by Fucile et al.5 in infants who performed oral stimulation at 10 days after birth showed that there was an increase in the ability to suck children within 48h after stimulation. Research conducted by Boiron et al.,6 found that administration of oral stimulation for 12min every day showed an increase in suction reflexes, in addition the amount of daily milk consumption increased compared to the control group. This study was supported by research conducted by Hwang et al.,7 where there was a significant increase in the ability to feed infants in the first 5min of stimulation. While the results of research conducted by Fucile5 that there is an effect of the provision of oral stimulation on the development of sucking ability, increased digestion and the potential to reduce the length of hospital treatment after being given perioral and intraoral stimulation for 10min every day.
The oral stimulation program used in this study is a combination of massage stroking and tapping techniques on oromuscular muscles and oral structure stimulation.5 This oral stimulation program consists of stimulation of the perioral structures such as the bottom of the nose, lips, cheeks, chin, and lips and stroking in the intraoral structure such as gums, inner cheeks, tongue and palate for 10min every day for 5 days.
MethodThe study was conducted in two midwife clinics in Pekanbaru, Riau Province of Indonesia. The data collection was conducted from August to October 2018. The design used in this study was quasi experimental with one group pre-test–post-test. The population in this study was all neonates aged<14 days of normal birth without complications. Respondents were selected by purposive sampling technique with inclusion criteria permitted by parents and exclusion criteria were the mother with breast problems. The study was conducted on 20 respondents who had met the research criteria.
Data collection was carried out using an observation sheet, on the observation sheet monitoring of sucking ability using the SCORE LATCH. Assessment of sucking ability (pre-test) is carried out before performing oral stimulation. After that, 1 session of oral stimulation was carried out for 5min. Stimulation sessions are carried out in clinics or at home. Oral stimulation is done by giving a light massage to the muscles around the mouth to stimulate the nerves and muscles in the oromuscular area. Massage begins from the area around the nose, ending in the area of the baby's jaw. After therapy, a 5-minute pause was given to wait for the next breastfeeding session and the mother was asked to breastfeed her baby again and then reassessed using a LATCH SCORE (post-test). Data from the results of this study were analyzed using univariate and bivariate tests. Bivariate tests are carried out using frequency tabulation, namely the data on infant gender, gestational age, body weight and the ability to suck. While the bivariate test was carried out by dependent T test on the variable oromuscular stimulation and the ability to suck the baby, but because the data were not normally distributed, alternative tests were carried out.
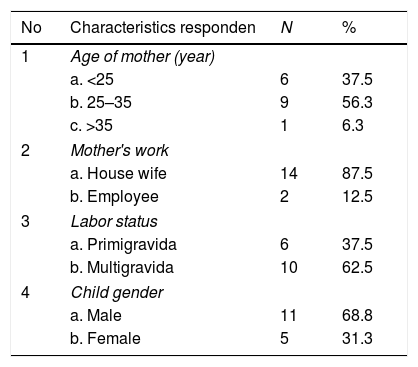
ResultData of respondent characteristics obtained in this study were maternal age, maternal occupation, maternal labor status and sex of the child. Can be seen in Table 1.
Statistical data shows that the majority of mothers are 25–35 years old (56.3%), most mothers are house wife (87.5%), most mothers are multigrafida (62.5%) and most babies are being a respondent is male (68.8%).
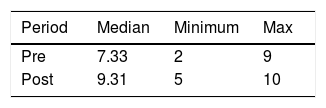
The study was conducted in one group and assessed LATCH scores before and after stimulation. Table 2 shows the LATCH scores before and after therapy.
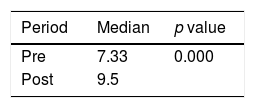
The average value (median) of the LATCH score before stimulation was 7.33 points, while the average value after stimulation was 9.31 points. Based on the results of further statistical tests on LATCH scores before and after therapy showed that oral stimulation was effective for increasing the score of breastfeeding, as shown in Table 3.
Oral stimulation has been shown to be effective in increasing LATCH scores, with an increase of 2 points with (p-value 0.000).
DiscussionMore than half of the mothers of all respondents studied were mostly aged 25–35 years (56.3%). This age is still a productive age for people in Indonesia in general. At this age the peak condition of maternal health is to give birth and care for children, and is the ideal for reproductive age. In this study there are still mothers under the age of 25 years and over 35 years, but generally mothers of respondents do not have serious health problems because they have been taken according to the desired criteria. In this study, the majority of mothers were house wife mother (87.5%). This condition is due to the fact that the place of data collection in both midwife clinics is indeed a suburb of Pekanbaru with the average middle class and lower class, and the head of the family working as a farmer and laborer. So that most mothers are housewives who do not participate in helping her husband increase the husband's income outside the home. Data obtained by most of the mothers was multigrafida (62.5%). In the conditions of multiparous births and mothers still in productive age, usually mothers still tend to be cooperative with nursing actions.
Based on the scoring results before and after therapy, the median LATCH score before therapy was 7.33 points, while the median value after therapy was 9.31 points. The LATCH score is obtained from the accumulation of scoring based on aspects: latch, audible swallowing, tip of nipple, comfort and hold. Research shows 19.2% neonates born were having fair sucking reflex.8 Oral stimulation in the neonate can stimulate the maturation of the motor sensory system in the oromuscular area for sucking and the breastfeeding process.8 Stimulation in the oromuscular in neonatal preterm has been shown to shorten the transition period of oral feeding to full oral feeding, and increase feeding efficiency.3
ConclusionBased on the results of further statistical tests on LATCH scores before and after therapy in this research showed that oral stimulation was effective for increasing the baby's breastfeeding score by 2 points (p-value 0.000). Based on the results of this study, oral stimulation in term neonates can be recommended as independent therapy by nurses to improve LATCH scores in neonates in the first 2 weeks after birth.
Peer-review of abstracts of the articles is under the responsibility of the Scientific Committee of Riau International Nursing Conference 2018. Full-text and the content of it is under responsibility of authors of the article.