To perform the cross-cultural adaptation and validity of a pictogram to assess communication needs in adults with artificial airway in ICU in Cartagena, Colombia.
MethodScale validation study, population comprising all the patients who were hospitalized in six ICU of Cartagena-Colombia. The sample was made up of 181 adult patients with artificial airway, the adaptation to Spanish was determined (translation, backtranslation, expert review, pre-final version, pilot test, final version), facial validity by expert agreement, content validity with the Lawshe index modified by Tristan (cut-off point 0.58), exploratory factor analysis (AFE) with the Bartlett’s test of sphericity and Cattell’s graph; internal consistency measured through the Cronbach alpha statistic.
ResultsPatients between the ages of 19 and 88 years participated (mean = 54 ± 17), 91.71% expressed frequent needs for accompaniment, knowing date and time; 61% of the experts agreed with the cross-culturally adapted items, the overall Content Validity Index (CVI) was 0.86 with agreement in understanding eleven items. The AFE suggested retaining 13 items and 3 factors (perception/cognition, elimination and exchange, comfort), which explain the construct. The internal alpha Cronbach consistency was 0.64.
ConclusionsThe pictographic material, Spanish version, was shown to be a multidimensional instrument composed of 18 items grouped in 3 factors. Therefore, it is recommended it be applied to the patient with artificial airway and to establish communication as a preliminary point of care in nursing.
Realizar la adaptación transcultural y validez de un pictograma para evaluar necesidades de comunicación en adultos con vía aérea artificial en UCI en Cartagena, Colombia.
MétodoEstudio de validación de escalas, población constituida por todos los pacientes que estuvieron hospitalizados en seis UCI de Cartagena-Colombia. La muestra fue conformada por 181 pacientes adultos con vía aérea artificial, se determinó la adaptación al español (traducción, retro-traducción, revisión por expertos, versión pre-final, prueba piloto, versión final), validez facial por acuerdo de expertos, validez de contenido con el índice de Lawshe modificado por Tristán (punto de corte 0.58), análisis de factor exploratorio (AFE) con la prueba de esfericidad de Barlett y gráfico de Catell; la consistencia interna medida a través del estadístico alfa Cronbach.
ResultadosParticiparon pacientes con edades entre 19 y 88 años (Media = 54 ± 17), 91,71% expresaron necesidades frecuentes de acompañamiento, conocer fecha y hora; el 61% de los expertos estuvo de acuerdo con los ítems adaptados transculturalmente, el Índice de validez de contenido (IVC) general fue 0,86 con acuerdo en comprensión de once ítems. El AFE sugirió retener 13 reactivos y 3 factores (percepción/cognición, eliminación e intercambio, confort), que explican el constructo. La consistencia interna alfa Cronbach fue 0,64.
ConclusionesEl material pictográfico versión español, mostró ser un instrumento multidimensional compuesto por 18 ítems agrupados en 3 factores por lo que se recomienda aplicarlo al paciente con vía aérea artificial y establecer una comunicación como punto preliminar de los cuidados enfermería.
The complexity of communication with intubated patients has some to develop instruments that assess the quality of communication. Alarcón and Serrato created a pictographic Therapeutic Communication Guide that involves five forms of communication in the intubated patient care process. However, this guide could not be implemented because the professionals using it could not be in the ICU continuously. In Turkey, Otuzoglu and Karahan designed a pictographic tool with the aim of facilitating the nurse-patient communication process and reported that 77.8% of patients found it helpful in communicating. Nevertheless, this non-verbal communication material, whose original language is Turkish, has only been translated into English; no Spanish version is available.
What does this paper contribute?In the world, and in Colombia, there are few tools available for this purpose. In addition, the materials developed have not been shown to be useful in the process of assessing nurse-patient communication. On the other hand, in Cartagena there is no valid and reliable instrument that can be used by the nurse to assess the communication needs of the adult patient with an artificial airway.
Implications of the studyTo obtain a Spanish-speaking communication tool that facilitates communication, favours the evaluation and understanding of patients’ needs in a timely manner, with greater diagnostic accuracy.12 It will also enhance professionals’ and patients’ satisfaction, increase therapeutic compliance, make better use of healthcare resources, and even generate better health outcomes in a wide range of clinical problems that are not visible given the difficulty in communicating and, therefore, will have a positive impact on the implementation of interventions that are consistent with each situation in particular.13
Communication and the professional nurse-patient relationship is a fundamental tool for sustaining the process of caring for and fulfilling the purposes of patient care. The communicative relationship is implemented through channels that may be verbal and non-verbal and that give make the nurse’s experience of care meaningful.1,2
Finke et al.3 argue that, in the practice of ICU nursing, the use of non-verbal communication is an articulating axis of care, both assistive and technological, aimed at providing quality care. Furthermore, this means of communicating influences recovery and length of stay, as well as reducing patient-reported frustration, as communication barriers are reduced.
However, some patients may perceive this communication process negatively, as the interaction with the nurse is limited, tends to be short, is not always focused on their needs and becomes an exhausting experience.4
As a result of certain health conditions or medical-surgical procedures, people are unable to maintain adequate lung ventilation spontaneously, requiring mechanical ventilation as a strategy to maintain gas exchange, which hinders communication, as well as the expression of thoughts, feelings, and wishes effectively, and interferes with their response to the hospitalisation process.5
The complexity of communication with mechanically ventilated ICU patients has led to the development of instruments that assess the quality of communication like the ICU Environmental Stressors Scale (ICUESS), which identifies difficulties in nurse-patient interaction and evidences the need for appropriate training in the use of adequate tools that respond to patients’ needs.6,7
However, in the world and also in Colombia, there are few materials to evaluate communication with intubated patients. Alarcón and Serrato8 developed a Therapeutic Communication Guide, with five forms of communication for the intubated patient care process, and included the use of images; however, this guide could not be implemented due to lack of reproducibility among nurses; furthermore, the guide showed the need for design adjustments.
Otuzoglu and Karahan9 in Turkey designed a pictographic material with the aim of facilitating the nurse-patient communication process and reported that 77.8% of patients found it helpful in communication. However, this non-verbal communication material, whose original language is Turkish, has only been translated into English for publication purposes, and no Spanish version is available.
In the city of Cartagena there is no valid and reliable instrument that can be used by the nurse to assess the communication needs of the adult patient with an artificial airway. This showed the convenience of linguistic and cultural adaptation, as well as face and content validation, of the tool constructed by Otuzoglu and Karahan.9
This process of instrument validation is a continuous and constant mode of evaluation that invites modifications based on the cultural context and available research to obtain a Spanish-speaking communication tool that facilitates communication, favours assessment and understanding of patients’ needs in a timely manner, with greater diagnostic accuracy.10,11 It will also increase professional and patient satisfaction, foster therapeutic compliance, make better use of healthcare resources, and even generate better health outcomes in a wide range of clinical problems that are not visible due to the difficulty of communication and, therefore, will have a positive impact on the implementation of interventions that are consistent with the specific situation.12
This would provide the nursing discipline with a simple and easy-to-apply material that improves communication with the ventilated patient.
The aim of the present study was to cross-culturally adapt and validate the Otuzoglu and Karahan pictographic material to assess the communication needs of patients with an artificial airway in the ICU.
MethodValidation study of scales without reference criteria. The participants were all adult patients who were hospitalised in six ICUs in the city of Cartagena and had an artificial airway, as well as meeting the selection criteria.
Taking into account the methodological suggestions for determining sample size in scale validation studies (10 participants for each item), 181 participants were estimated as a sufficient sample size for the evaluation of content validity and exploratory factor analysis (EFA).13
InstrumentThe Otuzoglu and Karahan pictographic material consists of 18 items; each item represents a patient’s need (to know about their evolution, hygiene, choking, discomfort with the barrier, nausea, hunger, mobility, night, day, date, and time, going to the toilet, seeing the family, being hot or cold). Each item is expressed by the nurse as a question and the patient is instructed to give a thumbs up (of either hand) if there is a need for communication or a thumbs down if there is no need for communication.
Transcultural adaptationThe cross-cultural adaptation was developed taking into account the methodological guide suggested by Beaton et al.14 in six stages, including translation into Spanish, back-translation into English, expert review, pre-final version testing, and, finally, pilot testing.
Facial validityInitially, a group of 20 experts was created, all of whom were professionals from different areas: thirteen nurses with experience in the ICU, two ICU doctors, two social communicators, one nurse with experience in psychiatry, two nurses with experience in the operating theatre; all had a minimum of one year’s experience in their area of expertise, in addition to the contribution of a graphic designer.
The pictographic material was evaluated by the experts according to the criteria of relevance, accuracy, clarity, and pertinence, at two different time points.15
Content validityFor content validity, the Lawshe model modified by Tristán (CVR) was used, defined as the agreement that the 20 experts have for each item according to the categories of pertinence, relevance, and the qualification criteria with nomenclature equivalent to: essential (the item meets the category), important, although not indispensable (the item moderately meets the category), and not necessary (the item does not meet the category).16
The results were interpreted by applying the equations of the Lawshe model for the calculation of the content validity of an instrument, retaining instruments that showed CVR ≥ 0.58 and with agreement of more than 50% of the panellists.16
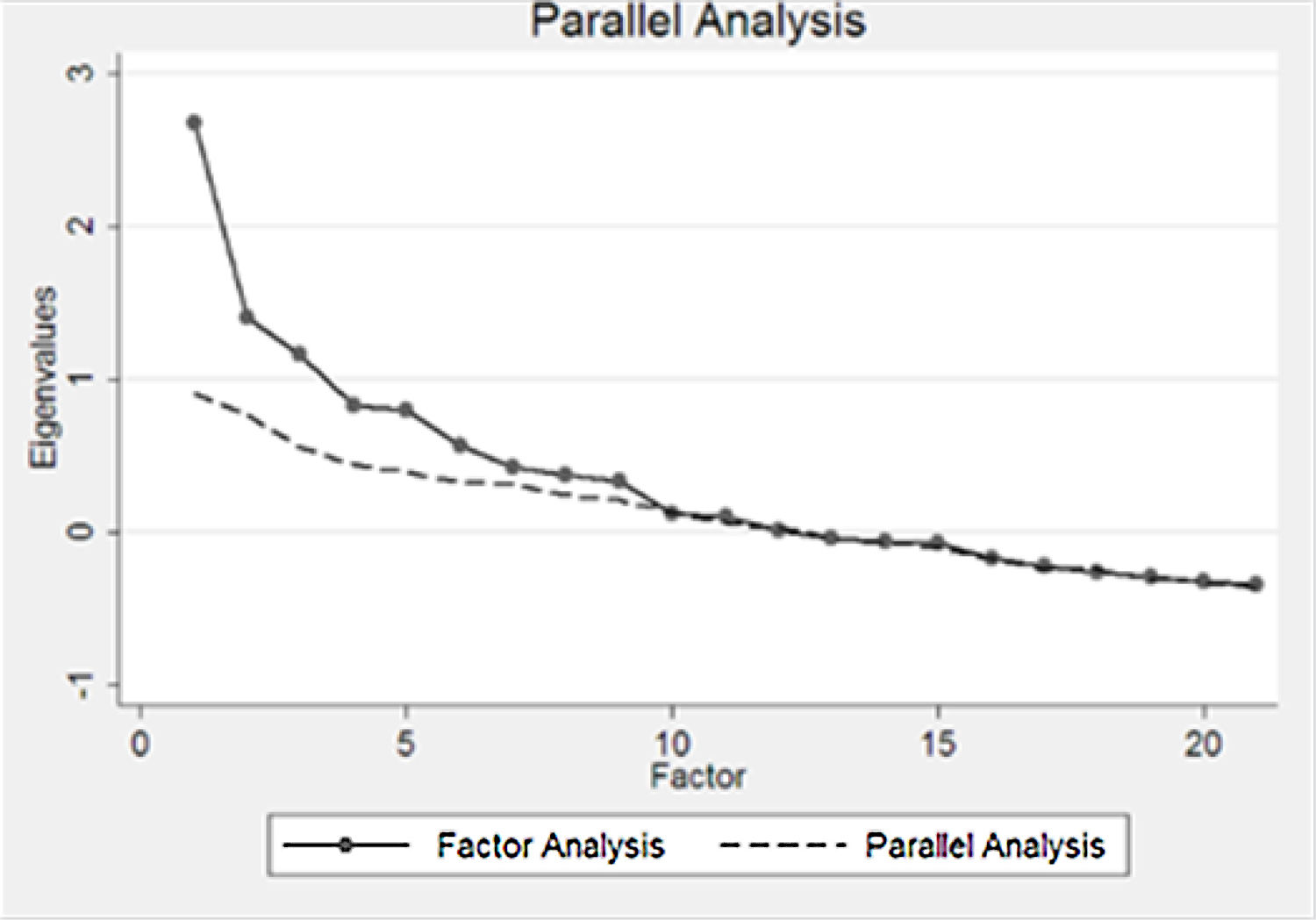
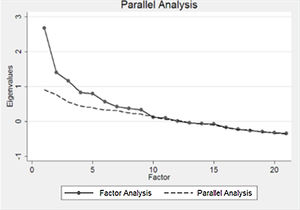
Factor analysesInitially, matrix factorisation was evaluated using Barlett’s test of sphericity,17,18 and deemed appropriate when p < 0.00. Likewise, the Kaiser-Meyer-Olkin (KMO) statistic was 0.80. The Catell plot was used to determine the number of factors to retain.19,20
Factor loadings ≥ 0.30 were taken into account to define factor composition, in accordance with Stevens,20 who considers that the minimum value for retaining an item is >.30.
Internal consistency was calculated using Cronbach’s alpha and evaluated according to the criteria proposed by Kline, being: acceptable (.60–.70), good (.70–.90), and excellent (>.90).21,22
Statistical analysisMeasures of central tendency (median, mean, and standard deviation) were calculated, depending on the symmetry of the distribution assessed with the Shapiro Wills test. If they were on an ordinal or nominal scale, they were shown as frequency measures (percentage).
Ethical considerationsThe principles established in Resolution 8430 of 199323 were taken into account, as were those stated in Helsinki24; similarly, [the study] also had the approval of the research committee of the Faculty of Nursing (Resolution n. 019-2017). Informed consent, a written agreement by which the research subject or their legal representative authorises their participation in the research, with full knowledge of everything related to it, was established. The people who participated in the research were all of legal age and their participation was voluntary (see Appendix B, Annex A).
ResultsThe study involved (n = 181) patients with ages ranging between 19 and 88 years, a mean age of 53.88, and DR ± 17.30. Half (52%) of the patients were male and married. As for the descriptive analysis of Otuzoglu and Karahan’s pictographic material, the vast majority (91.71%) expressed communication needs using the pictographic material. The most frequent need was: Do you want to be accompanied for a longer time during the visit? (91.71%), followed by: Do you want to know what time and date it is today? (91.16%). The communication barrier most frequently presented by patients was the orotracheal tube (65.19%); the median time spent by the nurse in applying the material was 15 min.
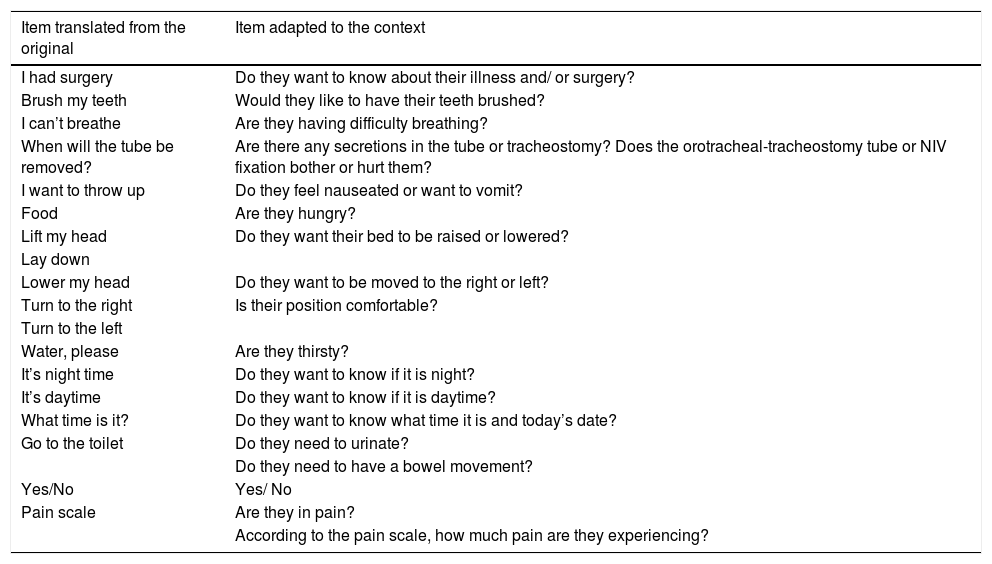
Transcultural adaptationOnce Beaton’s 6 steps were applied, the pre-final version was obtained and administered to both patients and a group of panellists; the answers provided made it necessary to make adjustments to the pictographic material to achieve the final Spanish version of Otuzoglu and Karahan’s pictographic material to evaluate communication needs in patients with an artificial airway in the ICU (Table 1).
Conceptual equivalence and linguistic adaptation of the items of the Spanish version pictographic material reviewed by panellists and patients.
| Item translated from the original | Item adapted to the context |
|---|---|
| I had surgery | Do they want to know about their illness and/ or surgery? |
| Brush my teeth | Would they like to have their teeth brushed? |
| I can’t breathe | Are they having difficulty breathing? |
| When will the tube be removed? | Are there any secretions in the tube or tracheostomy? Does the orotracheal-tracheostomy tube or NIV fixation bother or hurt them? |
| I want to throw up | Do they feel nauseated or want to vomit? |
| Food | Are they hungry? |
| Lift my head | Do they want their bed to be raised or lowered? |
| Lay down | |
| Lower my head | Do they want to be moved to the right or left? |
| Turn to the right | Is their position comfortable? |
| Turn to the left | |
| Water, please | Are they thirsty? |
| It’s night time | Do they want to know if it is night? |
| It’s daytime | Do they want to know if it is daytime? |
| What time is it? | Do they want to know what time it is and today’s date? |
| Go to the toilet | Do they need to urinate? |
| Do they need to have a bowel movement? | |
| Yes/No | Yes/ No |
| Pain scale | Are they in pain? |
| According to the pain scale, how much pain are they experiencing? |
Source: By the authors.
Facial validity was obtained after two meetings with the experts, who rated each of the 18 items according to the criteria of useless, very poor, good, and optimal. The acceptance point for the items was 11, representing 55% agreement of the panellists. These were: Do they want their teeth brushed?; Do they want their bed raised or lowered?; Do they want to be moved to the right or left?; Is their position comfortable? Do they want to know the date and time today?; Do they want to urinate?; Do they want to have a bowel movement?; Do they want someone special to visit them?; Do they want to be accompanied for longer at visiting time?; Are they hot?; Are they in pain?; (“According to the expression on the faces, which face represents you?”): “Answer with a thumbs up for yes/ thumbs down for no. For the remaining 9 items, adjustments were made to the semiotics and semantics in order to maintain them at the suggestion of the experts and patients who participated in the pilot test of the instrument.
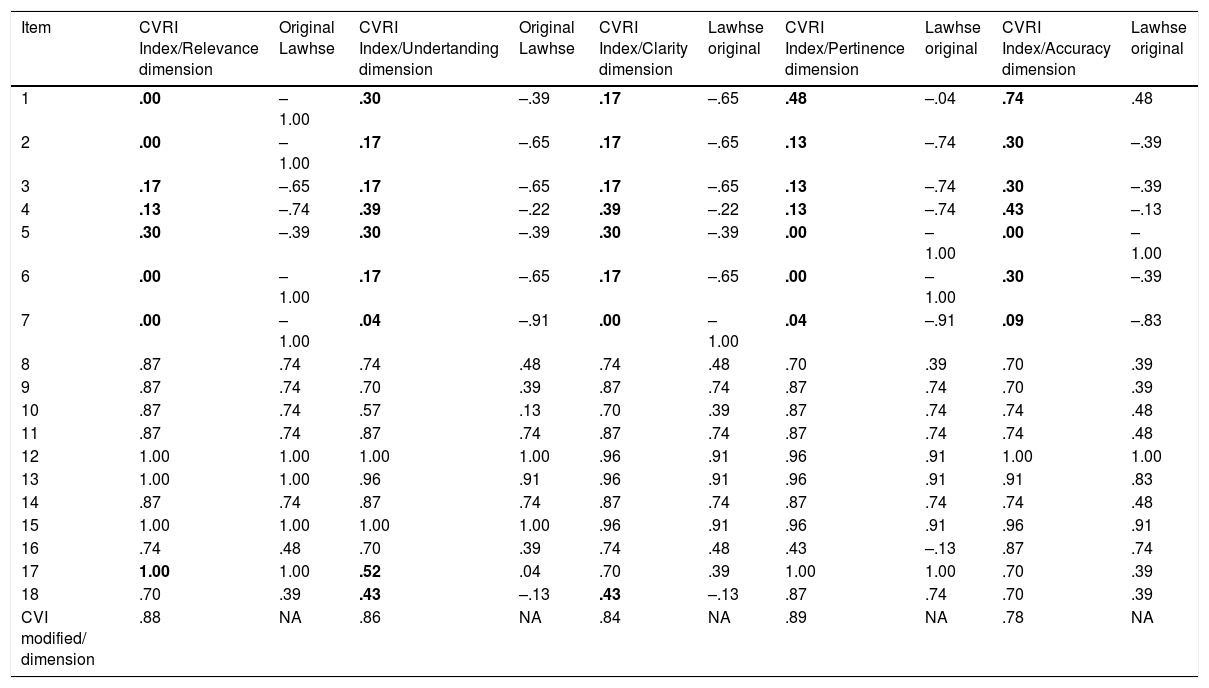
Content validityTable 2 exhibits the valid items according to Lawshe’s criteria.
Content validity according to modified Lawshe index of Otuzoglu and Karaham’s pictographic material to assess the communication needs of the intubated patient.
| Item | CVRI Index/Relevance dimension | Original Lawhse | CVRI Index/Undertanding dimension | Original Lawhse | CVRI Index/Clarity dimension | Lawhse original | CVRI Index/Pertinence dimension | Lawhse original | CVRI Index/Accuracy dimension | Lawhse original |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | .00 | –1.00 | .30 | –.39 | .17 | –.65 | .48 | –.04 | .74 | .48 |
| 2 | .00 | –1.00 | .17 | –.65 | .17 | –.65 | .13 | –.74 | .30 | –.39 |
| 3 | .17 | –.65 | .17 | –.65 | .17 | –.65 | .13 | –.74 | .30 | –.39 |
| 4 | .13 | –.74 | .39 | –.22 | .39 | –.22 | .13 | –.74 | .43 | –.13 |
| 5 | .30 | –.39 | .30 | –.39 | .30 | –.39 | .00 | –1.00 | .00 | –1.00 |
| 6 | .00 | –1.00 | .17 | –.65 | .17 | –.65 | .00 | –1.00 | .30 | –.39 |
| 7 | .00 | –1.00 | .04 | –.91 | .00 | –1.00 | .04 | –.91 | .09 | –.83 |
| 8 | .87 | .74 | .74 | .48 | .74 | .48 | .70 | .39 | .70 | .39 |
| 9 | .87 | .74 | .70 | .39 | .87 | .74 | .87 | .74 | .70 | .39 |
| 10 | .87 | .74 | .57 | .13 | .70 | .39 | .87 | .74 | .74 | .48 |
| 11 | .87 | .74 | .87 | .74 | .87 | .74 | .87 | .74 | .74 | .48 |
| 12 | 1.00 | 1.00 | 1.00 | 1.00 | .96 | .91 | .96 | .91 | 1.00 | 1.00 |
| 13 | 1.00 | 1.00 | .96 | .91 | .96 | .91 | .96 | .91 | .91 | .83 |
| 14 | .87 | .74 | .87 | .74 | .87 | .74 | .87 | .74 | .74 | .48 |
| 15 | 1.00 | 1.00 | 1.00 | 1.00 | .96 | .91 | .96 | .91 | .96 | .91 |
| 16 | .74 | .48 | .70 | .39 | .74 | .48 | .43 | –.13 | .87 | .74 |
| 17 | 1.00 | 1.00 | .52 | .04 | .70 | .39 | 1.00 | 1.00 | .70 | .39 |
| 18 | .70 | .39 | .43 | –.13 | .43 | –.13 | .87 | .74 | .70 | .39 |
| CVI modified/ dimension | .88 | NA | .86 | NA | .84 | NA | .89 | NA | .78 | NA |
The items in bold were revised and adjusted because they had a score <0.58. The table shows the 8 items whose semiotics were finally adjusted in order to continue to be included in the pictographic material.
Source: Created by the authors.
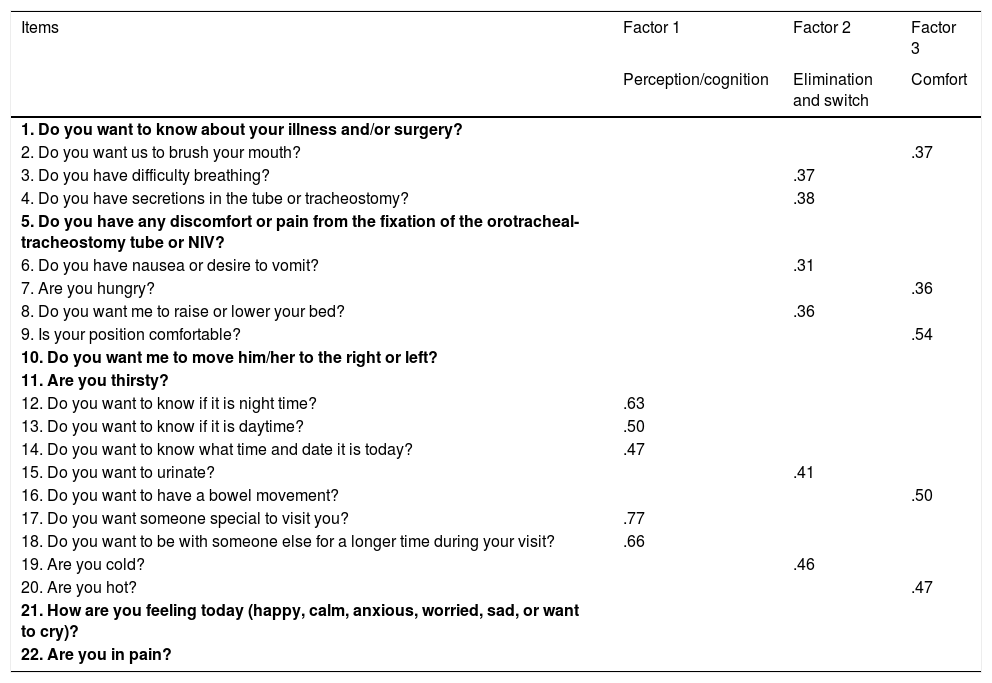
The instrument consisted of 18 items, 3 factors, and 13 domains whose factor loadings were >.30, resulting in items distributed as follows: factor 1 perception/cognition (items 9, 10, 11, 13); factor 2 elimination and exchange (items 3, 4, 5, 7, 12, 14); factor 3 comfort (items 2, 6, 7, 12, 15). Factor loadings ranged from .31 to .77. Items 1, 4.1, 7.3, 8, 16, and 17 were excluded as they had factor loadings of less than .30 (Table 3).
Exploratory factor analysis suggesting three domains that respond to the communication need construct.
| Items | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|
| Perception/cognition | Elimination and switch | Comfort | |
| 1. Do you want to know about your illness and/or surgery? | |||
| 2. Do you want us to brush your mouth? | .37 | ||
| 3. Do you have difficulty breathing? | .37 | ||
| 4. Do you have secretions in the tube or tracheostomy? | .38 | ||
| 5. Do you have any discomfort or pain from the fixation of the orotracheal-tracheostomy tube or NIV? | |||
| 6. Do you have nausea or desire to vomit? | .31 | ||
| 7. Are you hungry? | .36 | ||
| 8. Do you want me to raise or lower your bed? | .36 | ||
| 9. Is your position comfortable? | .54 | ||
| 10. Do you want me to move him/her to the right or left? | |||
| 11. Are you thirsty? | |||
| 12. Do you want to know if it is night time? | .63 | ||
| 13. Do you want to know if it is daytime? | .50 | ||
| 14. Do you want to know what time and date it is today? | .47 | ||
| 15. Do you want to urinate? | .41 | ||
| 16. Do you want to have a bowel movement? | .50 | ||
| 17. Do you want someone special to visit you? | .77 | ||
| 18. Do you want to be with someone else for a longer time during your visit? | .66 | ||
| 19. Are you cold? | .46 | ||
| 20. Are you hot? | .47 | ||
| 21. How are you feeling today (happy, calm, anxious, worried, sad, or want to cry)? | |||
| 22. Are you in pain? |
The items in bold were revised and adjusted because they had a score < .30.
Source: Created by the authors.
Catell’s graph suggested that three domains best explain the construct (Fig. 1).
Cronbach’s alpha coefficient was 0.64 for the items retained in the factor analysis, indicating acceptable internal consistency or homogeneity of measurement.
For the final Otuzoglu and Karahan pictographic material adapted and validated in Cartagena, Colombia, see Appendix B, Annex B.
DiscussionIn the present study, the Otuzoglu and Karahan pictographic material to determine validity and reliability across the 18 items that comprise the instrument, manages to assess the communication of the needs of patients with an artificial airway hospitalised in the ICU, similar to those of the original study by Otuzoglu and Karahan,9 which reveals that the pictographic material is effective for communication between healthcare staff and intubated patients in more than three quarters (78%) of the group intervened (p = .02).
In terms of content validity, the pictographic material displayed acceptable validity. Nevertheless, six images exhibited poor performance: learning (.30), hygiene (.17), breathing (.39), elimination (.30), eating (.17), and moving (.04), yielding values <.58, making it necessary to adjust these items. In this regard, it is important to highlight that the content validity index (CVI) suggests that items with values lower than .58 should be excluded from the instrument; however, in the present study these questions (images) were not discarded, as they are basic patient needs that must be communicated in order to satisfy them and nurses require the use of an instrument that enables them to identify them.25 Granados and Díaz,26 for their part, demonstrate that the needs (communication, movement, posture, breathing, eating and drinking, and the need for body hygiene) were classified by 84 health professionals as priorities in intubated ICU patients, which accounts for the importance of guaranteeing that the image reported by the patient be understood.
According to the results obtained, the internal consistency of the instrument was rated as acceptable (=.64), which shows that the items measured in the instrument present a degree of internal correlation between them. Other authors17,18 maintain that in the initial processes of construction and verification of the psychometric performance of an instrument, the minimum acceptable value for Cronbach’s coefficient can be .60; below this value, the internal consistency of the scale is low and it is suggested that the scale be revised and a process of fine-tuning be continued until better performance is achieved, ideally above .70.21 It is important to mention that there are no studies that prove the reliability of this material, given that the authors only found its effectiveness [sic]. Likewise, there are no studies in Colombia or in the world that demonstrate the validity and reliability of tools that examine the communication construct between nursing staff and ventilated patients in the ICU.27
As for the factor analysis, in the three factors retained: perception, cognition, elimination and exchange, and the comfort factor, the nomenclature was based on the taxonomy of the nursing profession, the North American Nursing Diagnosis Association (NANDA); these diagnoses are classified into domains, which represent the human responses or needs that patients may present in healthcare institutions. Likewise, in this study, the items that make up each factor are related to the 14 needs proposed by Virginia Henderson, which are common and essential in every human being. In this regard, Sahagún and Frutos28 identified the diagnoses that most frequently occur in the ICU related to the needs proposed by Henderson, which coincides with the domains that assess the needs found in the present research (breathing normally, eating and drinking adequately, elimination by all routes of elimination, moving and maintaining a suitable position, maintaining body temperature, maintaining body hygiene, skin integrity, and communicating with others to express emotions, needs, and fears).
As proposed by Stevens,20 six items from the original 18-item pictographic material were excluded (being informed, position, discomfort related to the tube, thirst, pain, mood) because they had factor loadings of <.30. These needs, according to Kolcaba,25 constitute specific care that the nurse performs on a daily basis in the ICU and which Kolcaba distributes as 28% for the physical aspect and 56% for the psychospiritual dimension. These activities are routinely conducted without the patient requesting them, and for this reason, it is difficult for the patient to communicate them; likewise, the patient is in a different context from their original context, in addition to the alarms and noises typical of the area that constitute the impediment that generates the communication barrier itself.
In this order, in this study, the authors found that 61% (n = 181) of the patients had difficulty expressing pain; 82% needed to be moved, and 55% had secretions. These data are consistent with those reported by Martinho and Rodriguez,29 who evaluated a scale to assess the level of communication difficulty in intubated patients and found that 38% (n = 33) of them considered that communicating physical needs, such as position changes, feeling pain, and needing suction, was “extremely difficult.”
Henao and Amaya30 conducted a study similar to the present research. They designed an instrument to probe individualised nursing care of adults in the ICU (CEI-ICU), taking the criteria proposed by NANDA as a reference to identify care interventions, and reported a CVI of between .58 and .90, internal consistency of .66, and the content validity quantified through exploratory factor analysis suggested 4 factors and 8 items (NANDA domains), to conclude that the needs of intubated patients were nutrition (64%), elimination (53%), activity (73%), vital principles (62%), and self-perception (52%), in line with the needs assessed by the Otuzoglu and Karahan pictographic material in the Spanish version, which reinforces the need for a capable, valid, reliable, and useful instrument to establish effective communication and identify these needs as being the most common ones in patients with an artificial airway hospitalised in ICUs.
Likewise, the CEI ICU study revealed that 100% of ICU nurses carry out activities that respond to the domains of perception/cognition and comfort; within these domains are the items of having pain and how [the patient] feels today, wanting to know about their illness, wanting to be moved to the right or left, which were eliminated from the Otuzoglu and Karahan pictographic material in the Spanish version after conducting the factor analysis, revealing that the nurse identifies these needs in intubated patients without the patient having to express them.
Some of the limitations of the present study have to do with the lack of a gold standard to compare the psychometric properties of this instrument with those that have been applied in other contexts to a population with similar characteristics. Likewise, instruments with polytomous response options (Likert) may be better able to measure the construct, unlike what was observed in this study with dichotomous responses, which may have influenced the result of the factor analysis, showing a multidimensional type of material that, in principle, was intended to be unidimensional, and its acceptable internal consistency.
In conclusion, the pictographic material to identify communication needs turned out to be a multidimensional instrument that consisted of 18 items in 3 domains that rely on the NANDA domains as a reference for their nomenclature, with acceptable validity and reliability. Therefore, the authors recommend promoting the use of reliable pictographic tools that make it possible for the patient with an artificial airway to maintain interaction with healthcare personnel in which communication is established as a preliminary point of nursing care.
For the development of further instruments in non-verbal communication, a theoretical disciplinary reference must be taken into account to guide the process of psychometric application, so that it can be compared with studies in different countries in which both theory and communicative tools have been used.
It is important to continue to examine the psychometric properties of the Spanish version of the pictographic material in order to generate valid constructs that offer better contributions to the instrument so as to establish communication with the healthcare professional, as well as to see options for its use with other populations.
FundingThis work received no specific support from the public, commercial or non-profit sectors.
Conflict of interestNone.
Please cite this article as: Manrique-Anaya Y, Cogollo Milanés Z, Simancas Pallares M. Adaptación transcultural y validez de un pictograma para evaluar necesidades de comunicación en adultos con vía aérea artificial en cuidados intensivos. Enferm Intensiva. 2021;32:198–206.