The COVID-19 pandemic and its associated factors have been shown to affect anxiety levels of young people. We meta-analytically assessed the prevalence of anxiety symptoms and anxiety disorders in children and adolescents during the pandemic, and the predictors and moderating factors influencing anxiety.
MethodsMultiple databases and registers were searched in this PRISMA and MOOSE-compliant systematic review and meta-analysis (PROSPERO:CRD42021266695) until 27/06/2021. We included individual studies evaluating the prevalence and characteristics of anxiety symptoms or anxiety disorders in children and adolescents (mean age ≤18 years), during the COVID-19 pandemic. Data extraction and quality assessment were carried out by independent authors. Random-effects meta-analyses of the prevalence of anxiety symptoms and anxiety disorders were conducted using Comprehensive Meta-Analysis (CMA) V3.
Results74 articles (total participant sample=478,882) were included (mean age=13.4 years, 52.3% female). The pooled rate of children and adolescents fulfilling diagnostic criteria for anxiety disorders was 13.0% (95%CI=4.9–30.1); the pooled prevalence of anxiety symptoms was 26.5% (95%CI=20.3–33.9). Anxiety symptoms were significantly more prevalent in females than males (B = 0.103, p<.001), significantly higher during the second wave of COVID-19, following July 2020, than during the first wave, prior to June 2020, (Q= 8.136, p=.017), and during school closure (Q= 8.100, p=.014). Quality of included studies was overall moderate.
ConclusionsThere is a high prevalence of anxiety symptoms in children and adolescents during the COVID-19 pandemic, especially amongst females. This study identifies vulnerable groups, risk, and protective factors, which is crucial to developing clinical practice to prevent further mental health deterioration in young people.
COVID-19 was declared a global pandemic on the 11th of March 2020 by the World Health Organization (WHO).1 As of the 13th of April 2023, a total of 762,739,900 COVID-19 cases have been confirmed worldwide, with 6,896,778 deaths.2 The COVID-19 pandemic is having detrimental effects on public mental health,3 with a significant impact on mental health outcomes in children and adolescents,4-6 especially older adolescents, girls, and young people with neurodiversities and/or chronic physical conditions.7 Anxiety disorders and anxiety symptoms account for the most prevalent psychiatric problems in those aged 6 to 18 years old, with a worldwide prevalence of 6.5%.8 Anxiety symptoms seem to have exacerbated in the general population during the COVID-19 pandemic.3
A previous meta-analysis assessed the prevalence of anxiety amongst medical students during COVID-19,9 which was shown to significantly increase compared to pre-pandemic levels. Meta-analyses on the prevalence of anxiety amongst the general population3 and college students10 have also been conducted, showing female sex as the most significant risk factor. A narrative review and a systematic review on the psychological impact of COVID-19 thus far have shown a high prevalence of anxiety, amongst children4 and adolescents,5 respectively; but no meta-analyses were conducted. A recent meta-analysis of 29 studies assessed the prevalence of anxiety symptoms and depressive symptoms in children and adolescents, finding a 20.5% prevalence of clinically elevated anxiety, highlighting increased anxiety levels, and evaluated three moderating factors: age, sex, and pandemic data collection time point.6 Further to this, a recent meta-analysis of children and adolescents from Turkey and China found a 26% prevalence of anxiety, with adolescents and females reporting a higher prevalence of anxiety than children and males.11
This systematic review and meta-analysis evaluates and comprehensively characterizes anxiety symptoms and anxiety disorders in children and adolescents during the COVID-19 pandemic, evaluating a broad range of moderating factors. This review aims to meta-analyse the prevalence of anxiety symptoms and the proportion of anxiety disorder emergence present amongst children and adolescents during the COVID-19 pandemic. This systematic review also aims to provide comprehensive evidence about the influence of predictors and moderating factors on the anxiety symptoms within children and adolescents.
MethodsWe followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (eTable 1 & eTable 2) and Meta-analyses Of Observational Studies in Epidemiology (MOOSE) guidelines12 (eTable 3). We pre-registered the study protocol in PROSPERO (CRD42021266695).
Search strategy and selection criteriaA systematic search was conducted on PubMed and Web of Science database (Clarivate Analytics), incorporating the Web of Science Core Collection, BIOSIS Citation Index, KCI-Korean Journal Database, MEDLINE, Russian Science Citation Index, and SciELO Citation Index as well as Cochrane Central Register of Reviews, and Ovid/PsycINFO databases from inception until the 1st of April 2021 was conducted and then updated on the 27th of June 2021. The following search terms were applied and adapted accordingly: (“COV” OR “coronavirus” OR "Orthocoronavirinae" OR "SARS-CoV-2″ OR "2019 nCoV" OR "2019nCoV" OR "2019 novel coronavirus" OR "COVID-19″ OR "new coronavirus" OR "novel coronavirus" OR "SARS CoV-2″ OR "Wuhan coronavirus" OR "COVID 19″ OR "2019-nCoV") AND ("teen" OR "child*" OR "adolesc*" OR "kid" OR "student" OR "p?ediatric" OR "juven*") AND ("anxiet*" OR "anxious" OR "hypervigilance" OR "social anxiety" OR "panic" OR "GAD" OR "generali?ed anxiety disorder").
To identify relevant grey, non-published, literature, we looked at medRxiv, psyArXiv, and bioRxiv pre-print databases. A manual search of the references of the included primary studies and reviews related to this topic was conducted. Articles identified were screened as abstracts by two independent researchers (UP, IC; MSc level researchers, supervised by a senior academic researcher). After excluding those that clearly did not meet our inclusion criteria, the full texts of the remaining articles were then assessed for eligibility and decisions were made regarding their final inclusion in the review.
The inclusion criteria were as follows: 1) individual studies with original data, including grey literature, 2) conducted in children and adolescents with a mean age of <18y, in line with previous studies,13 3) assessing exposure to COVID-19, 4) reporting the percentage of anxiety and/or depression symptoms/disorder in this population, 5) in English. The exclusion criteria were as follows: 1) conference proceedings, case reports, narrative reviews, or qualitative studies, 2) studies including adults with a mean age >19-years-old, 3) studies in which children and adolescents were not exposed to COVID-19, 4) studies focusing on physical health outcomes or mental health outcomes other than anxiety.
Data extractionData extraction was led by the main researcher (UP) and also independently extracted by members of the research team who extracted data in pairs and attained consensus via group discussion (HAG, KP, BK; MD/Doctorate level researchers, supervised by a senior academic researcher). Any discrepancies arising were resolved through consensus, consulting another senior academic researcher (GSP) if an agreement was not attained. The variables extracted included: first author, year of publication, country(ies), wave of COVID-19 during study duration, whether there was school closure, the percent attending school, whether there was a lockdown (as operationalised in each study - such as, home confinement, school closure, quarantine etc.), months since March 2020 - when COVID-19 was declared a global pandemic, study design (cross-sectional, longitudinal), sample size, sex (% females), age (mean±SD, range), tools to assess anxiety symptoms (see eTable 4), mental health outcome (anxiety measurement instrument used, threshold of the anxiety measurement instrument used), quality appraisal (see below) and key findings.
Strategy for data synthesisA meta-analysis for the prevalence of anxiety symptoms was conducted as our primary outcome. A secondary analysis was conducted on the prevalence of anxiety disorders according to DSM/ICD criteria. Random effects model meta-analyses were conducted pooling the percentage (95%CI) expressing the rate of the symptoms/disorders. We also tested using sub-analyses the prevalence of anxiety symptoms by continent (Europe, Asia, North America, South America), wave of the pandemic (first wave – up to June 2020 –, second/subsequent waves – from July 2020), school closure (yes, no) lockdown status (yes, no), design (cross sectional, longitudinal).
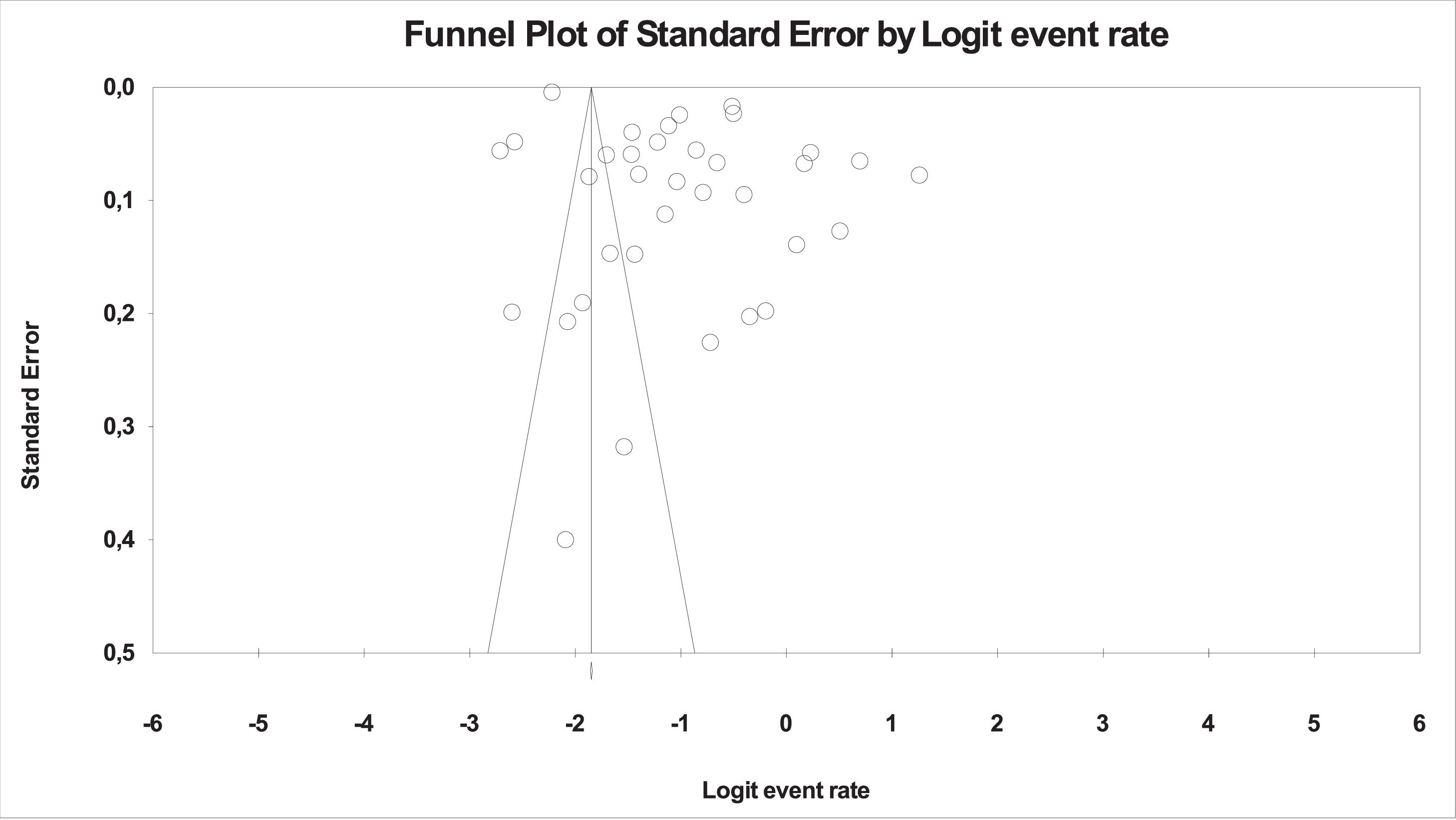
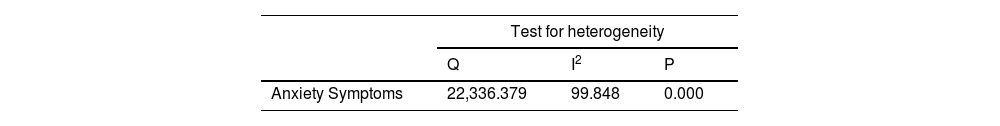
Hedges’ g was used to estimate parameters and effect size in the meta-analysis. Publication biases were assessed with the metafunnel function visually by examining the funnel plot and quantitatively by the Egger's test.14 The trim and fill method was used to correct the estimates in the case of publication biases. The presence of significant heterogeneity amongst study point estimates was assessed using Q statistics. The proportion of the total variability due to true heterogeneity was evaluated with the I2 index. We conducted meta-regressions including age, sex, sample size, percent attending schools and longitudinal progression (i.e., time passed from March 2020) as moderating factors. The meta-analyses were conducted using Comprehensive Meta-Analysis (CMA) V3.15
Results of the systematic review were synthesised narratively and summarised in tables. Results were stratified by clinical at-risk populations and risk factors, followed by protective factors.
Quality appraisalFor study appraisal, this systematic review used the Newcastle-Ottawa Scale (NOS). We used the appropriate version of the NOS according to the design of the studies (cross-sectional studies (see appendix) or cohort studies16). The quality assessment process was led by the main researcher, and also independently assessed by other co-authors (HAG, KP, BK). Any disagreements that arose were discussed with the corresponding author and resolved.
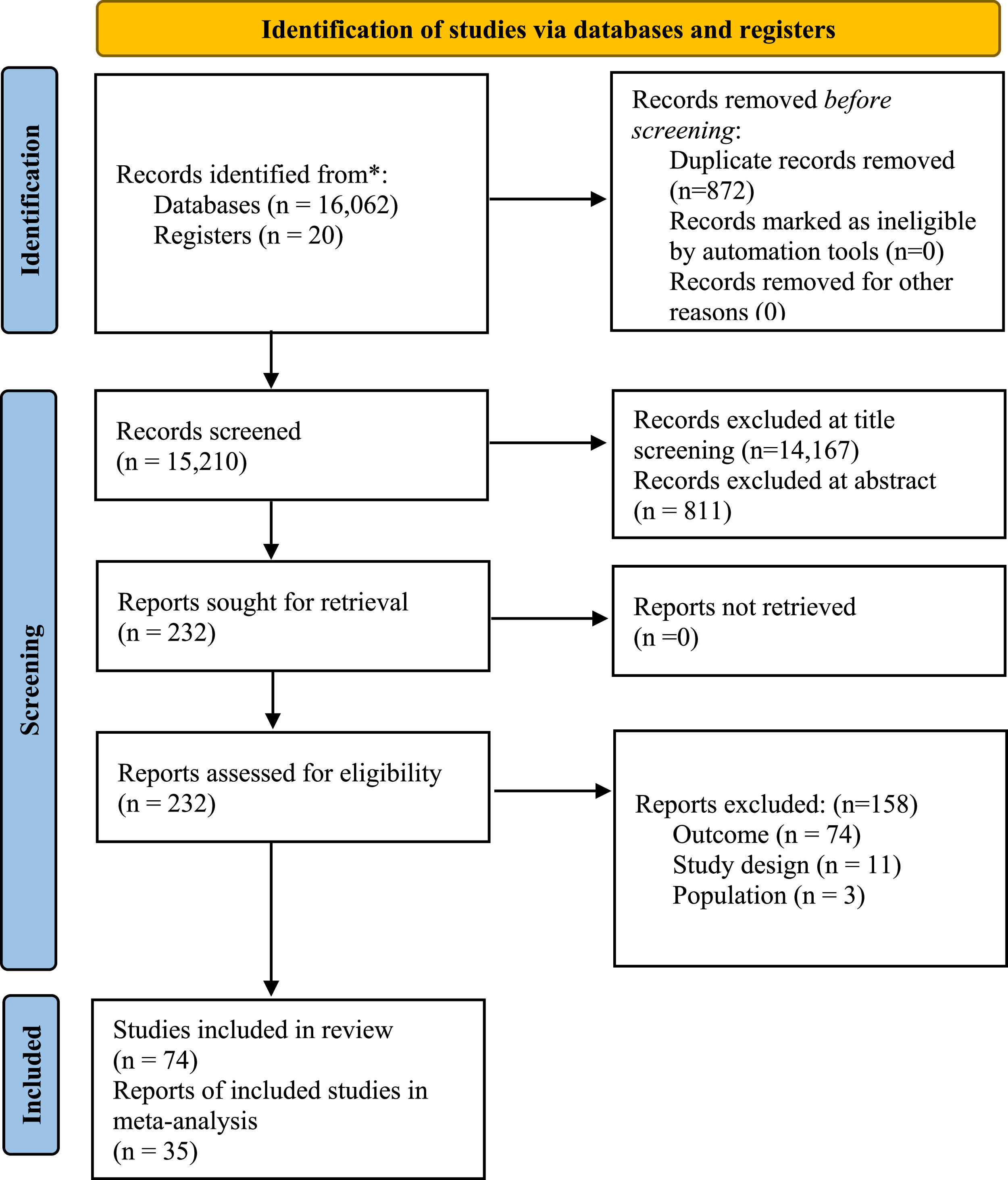
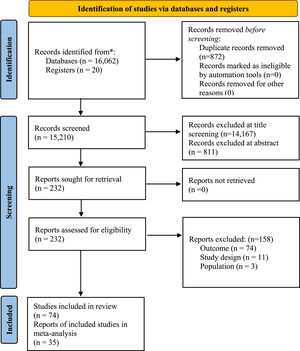
ResultsSearch resultsOur electronic search identified 16,082 publications; a further 6 publications were identified via backward searching of key papers. 1043 and 166 publications went through abstract screening and full-text screening, respectively; 92 publications were excluded (see eTable 7), and 74 publications, including one study from pre-print databases,17 met the criteria for inclusion. After accounting for overlap in study outcomes, 35 samples reported meta-analysable results for anxiety. Results of the search follow in the PRISMA 2020 flow diagram (Fig. 1).
Study characteristicsSample sizes ranged from 45 to 373,216 participants (total sample size (n)=478,882), of which 52.3% were female. Participants had a mean age of 13.4 years (range: 0–22). Most publications were cross-sectional studies (number of studies (k = 63, n = 85.1%), the rest were longitudinal studies or clinical trials (k = 11, n = 14.9%). The included studies were conducted in Asia (k = 42, n = 56.8%), Europe (k = 21, n = 28.4%), North America (k = 9, n = 12.2%), South America (k = 1, n = 1.4%), and Australia (k = 1, n = 1.4%). (Summary of study characteristics and key findings can be found in eTable 8).
Quality assessmentThe quality of the included studies was 6.3 ± 1.6 (range: 2–9), which is considered moderate quality. Cross-sectional studies scored an average of 6.4 ± 1.6 (range: 2–9) out of 9.0 stars longitudinal studies scored an average of 5.8 ± 0.9 (range: 5–8) out of 8.0 stars (see eTable 8 & eResults).
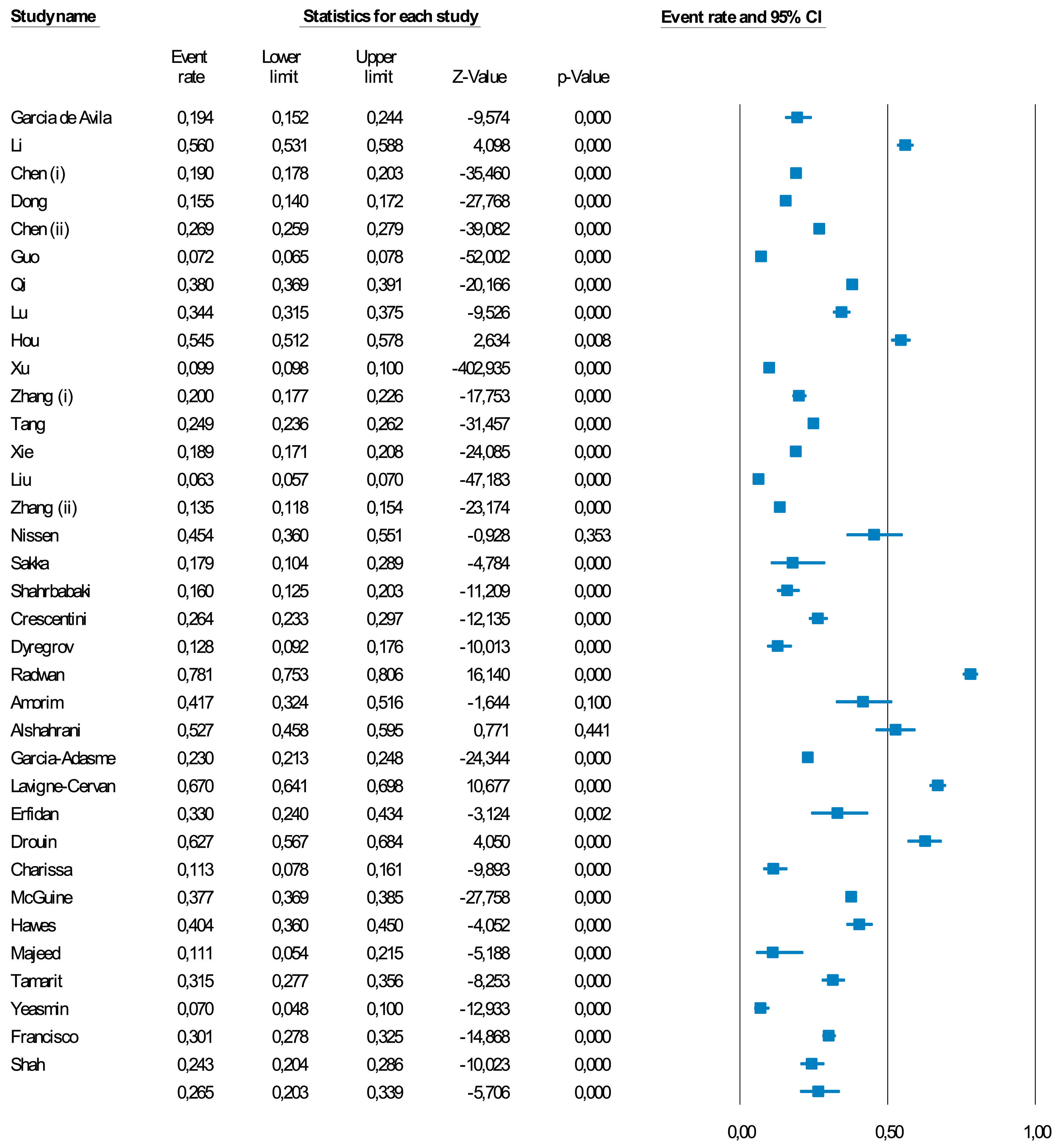
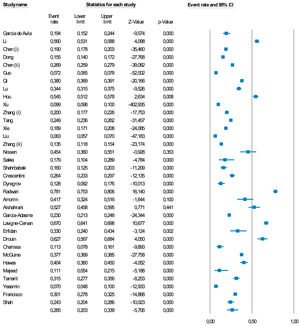
Meta-analysisA meta-analysis of 35 studies showed a pooled percentage of anxiety symptoms during the COVID-19 pandemic of 26.5% (95%CI=20.3–33.9) (Fig. 2 & Table 1). The prevalence ranged from 1.8%18 to 62.7%.19 13.0% (95%CI=4.9–30.1) of children and adolescents had DSM/ICD anxiety disorders (k = 4). Anxiety levels worsened from baseline to follow-up (hedges' g = 0.493, 95%CI=0.430–0.556) (k = 3) in the longitudinal studies (mean follow up=95.3 days) (eTable 5).
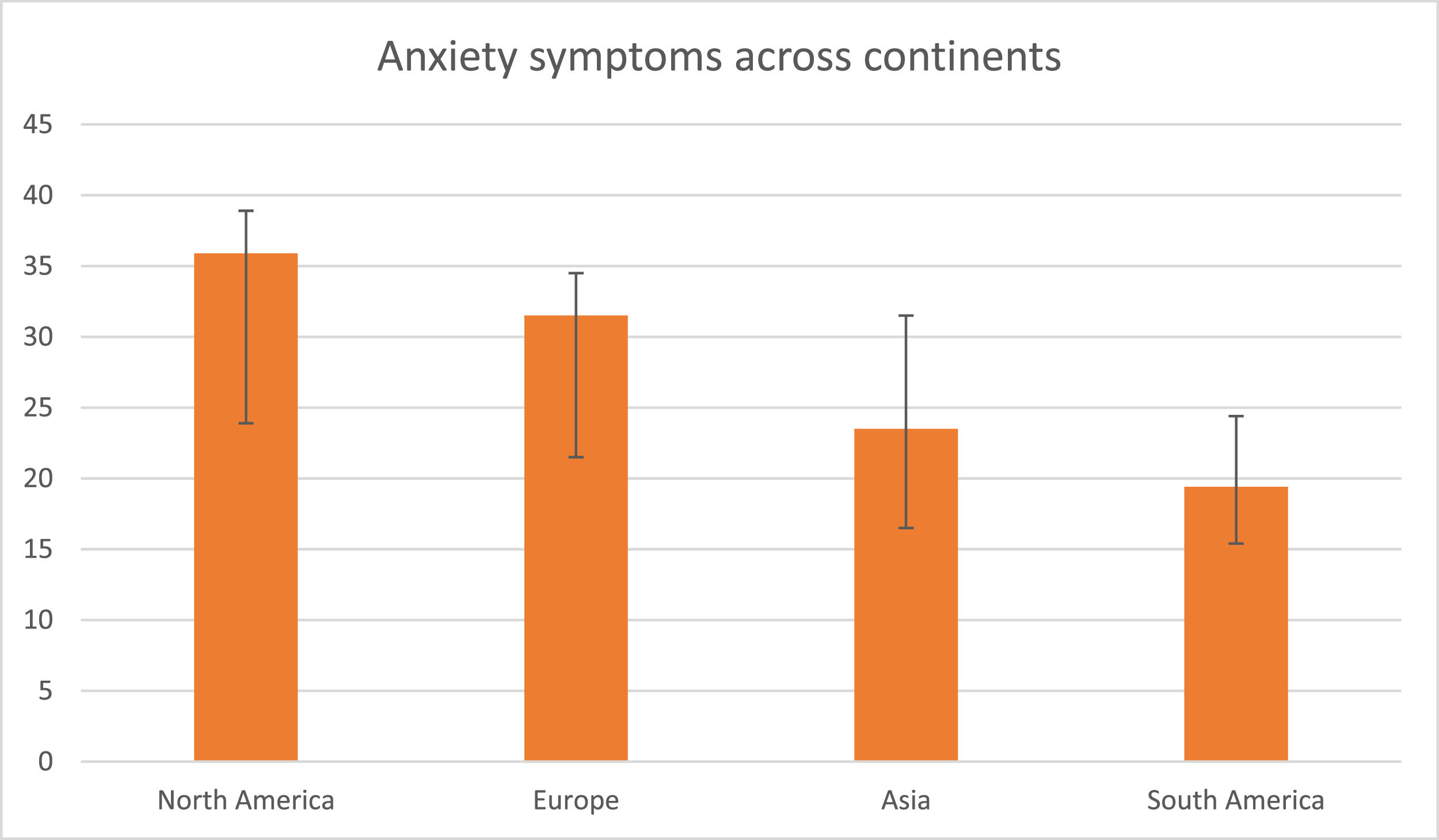
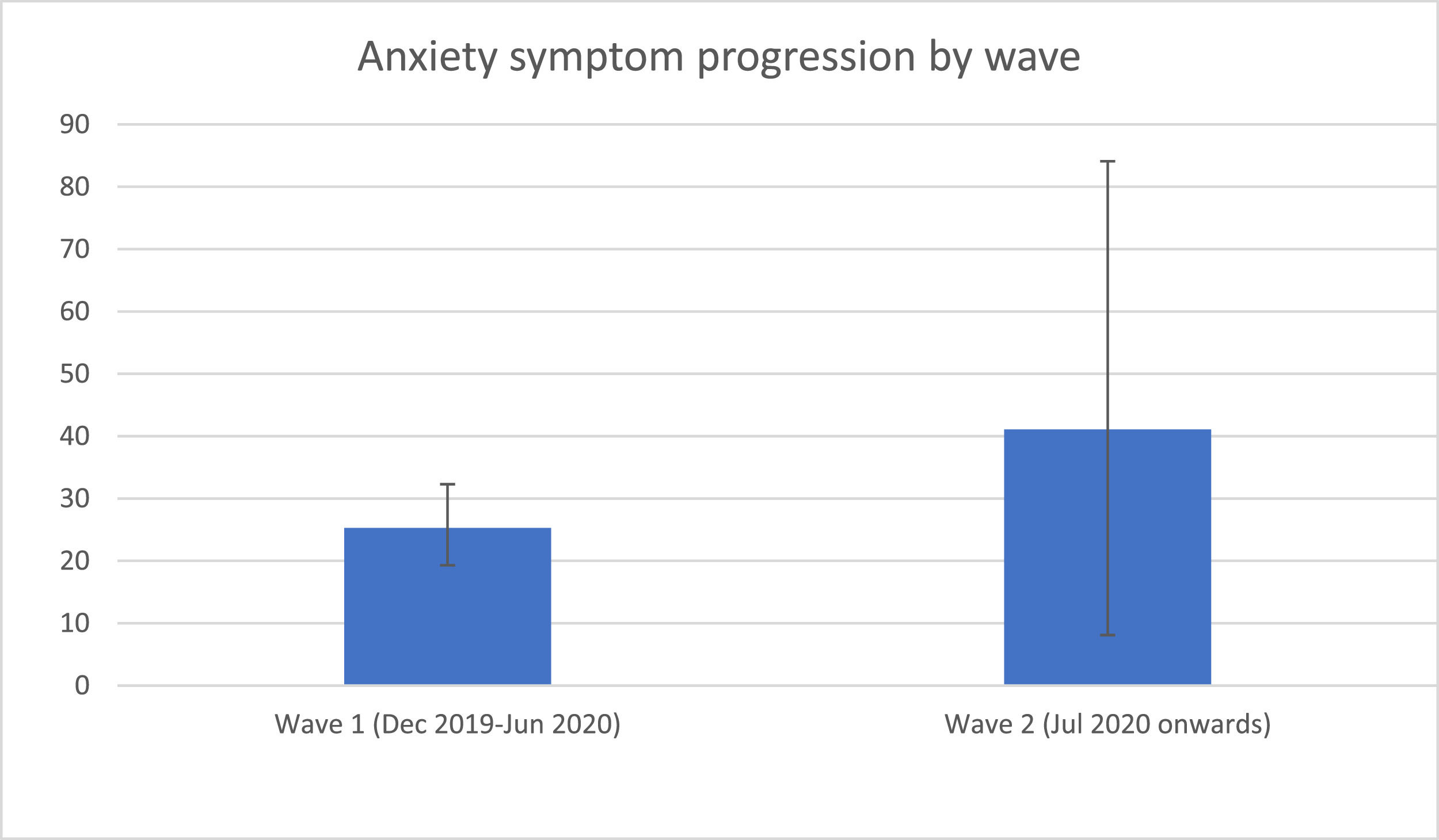
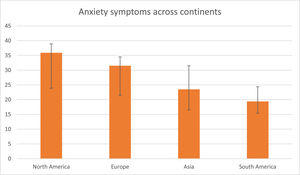
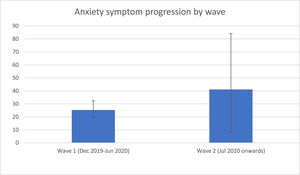
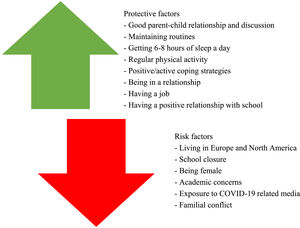
In the sub-analysis (see eTable 5), we found that anxiety symptoms were more prevalent in North America (35.9%, 95%CI=24.1–38.9, k = 4, n = 11.4%) and Europe (31.5%, 95%CI=21.4–34.3, k = 9, n = 25.7%) than in Asia (23.5%, 95%CI=16.7.4–32.1, k = 21, n = 60.0%) and South America (19.4%, 95%CI=15.2–24.4, k = 1, n = 2.9%) (Q = 9.231, p=.026) (Fig. 3). We also found that there were more anxiety symptoms during the second wave, following July 2020 (41.1%, 95%CI=8.1–84.7, k = 3, n = 8.6%), than during the first wave, from December 2019 to June 2020 (25.3%, 95%CI=19.2–32.6, k = 32, n = 91.4%) (Q = 8.136, p=.017) (Fig. 4). We finally found that there were more anxiety symptoms in children whose school had closed (17.8%, 95%CI=11.9–25.8, k = 10, n = 31.3%) than those whose school had not closed (32.5%, 95%CI=26.9–38.7, k = 22, n = 68.8%) (Q = 8.100, p=.014). We did not find differences between studies conducted during lockdown period (k = 22) and those in which this was not specified (k = 12) (p=.576) or between cross-sectional (k = 32) and longitudinal studies (k = 3) (p=.551).
Meta-regressions between the outcome of anxiety and other predictorsIncreased number of months since March 2020 (B = 0.150, p<.001) and increased % of females (B = 0.103, p<.001) were associated with a higher prevalence of anxiety symptoms (see eTable 6). Meta-regressions for age, % attending school, and sample size did not result statistical significance (all p>0.05) (eTable 6).
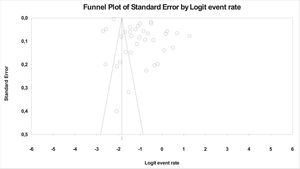
Publication bias (small study effect) assessmentSome asymmetry was found within the funnel plot (Fig. 5) and Egger's test quantitatively suggested publication bias (t-value=3.695; p=.00079). However, trim and fill value did not adjust the results and the plot did not indicate small-effect bias (Fig. 5). Thus, publication bias was not found.
Narrative synthesisThe following clinical populations reported an increased risk of anxiety symptoms: Autism Spectrum Disorder (ASD) (p<.001),20 hearing difficulties (p=.003),21 haematology-oncology disease (p=.01),22 neurological disorders (p<.05),23 multiple sclerosis (p<.001),24 and those who had previously sought out psychiatric help (OR=4.4, 95%CI=2.5–25.3).25
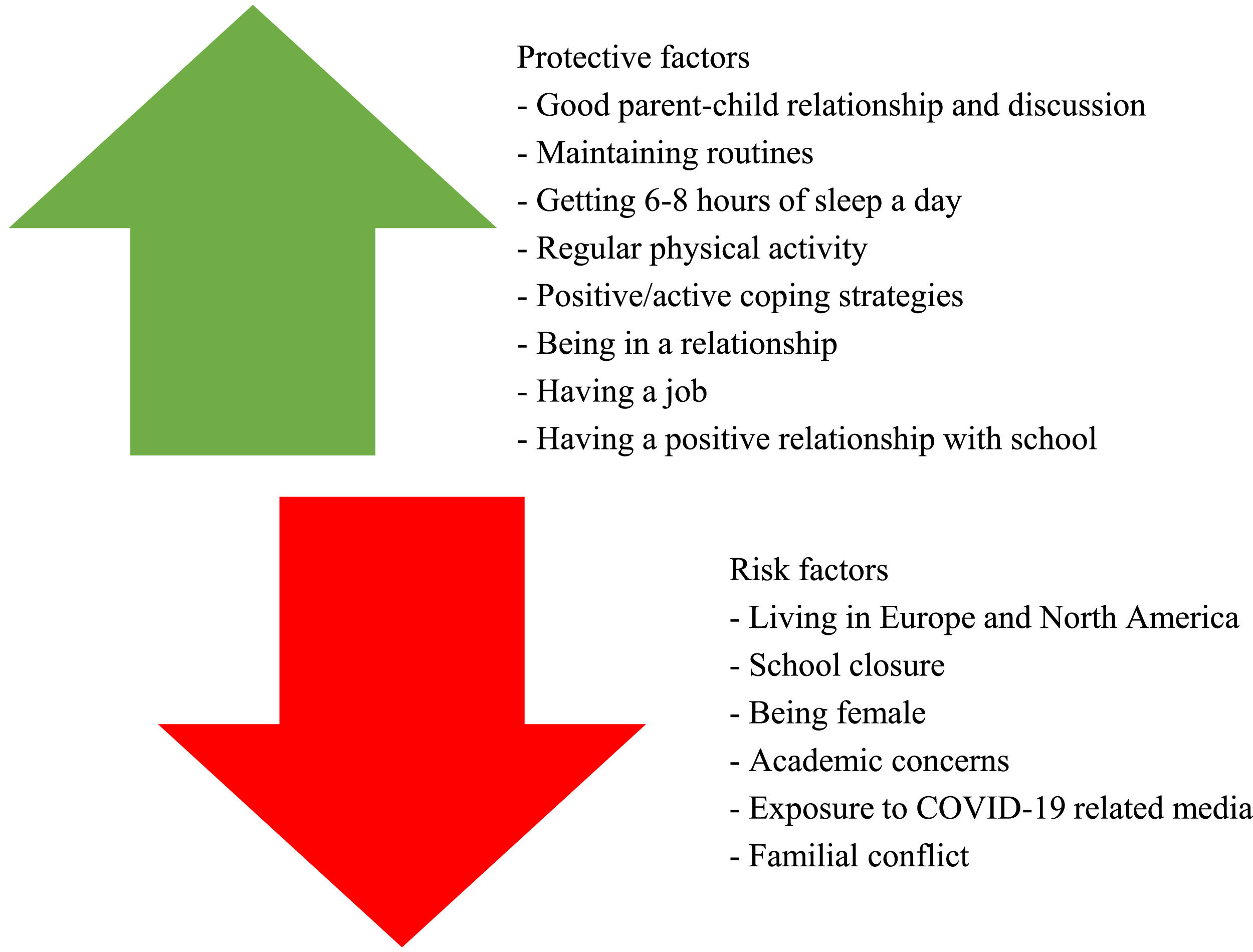
Risk factors for exacerbation of anxiety symptoms evaluated during COVID-19 included family relationships, media use, and level of COVID-19 fear (see eTable 4). Regarding family, parental anxiety symptoms (95%CI=1.0–4.6),26,27 parent behaviour, including their employment status, sports practiced, and compulsions (p<.001),28,29 being away from parents (OR=1.3, 95%CI=1.1–1.6),30,31 number of people at home (OR=1.3, 95%CI=1.0–1.6),30 having siblings (p<.001),32 and arguments with parents (OR=2.5, 95%CI=1.8–3.6)33 have been associated with exacerbation of anxiety symptoms. Similarly, a family member testing positive for COVID-19 (OR=3.8, 95%CI=1.8–13.6)25 was found to be a risk factor for anxiety symptoms. Furthermore, exposure to COVID-19 related media was associated with more severe anxiety symptoms (OR=1.5, 95%CI=1.0–2.3).18,25,34,35 COVID-19 related fear was also a common risk factor for anxiety symptom exacerbation (OR=1.3, 95%CI=1.0–1.5)30-32,36-41 (see Fig. 6).
School concerns were associated with panic disorder (p<.001), social anxiety (p<.05), and generalised anxiety (p<.001).39 Specifically, being a senior in high school as opposed to younger ages (OR=1.3, 95%CI=1.2–1.4),31,42-44 poor academic records (OR=1.4, 95%CI=1.0–1.9),45 and inattention during online studying (OR=1.3, 95%CI=1.0–1.8) were associated with exacerbation of the symptoms of anxiety. Longitudinal research has shown that pre-pandemic symptoms of anxiety were the strongest indicator of anxiety symptoms during the pandemic (p<.001).46
Personal protective factors included positive coping (OR=0.946, p<.001),47 such as regular moderate-high level physical activity (p<.05),36,37,40,42,45,48,49 sleeping 6–8 h a day (p<.001),40,42 maintaining routines (p=.045),20 balanced videogame usage (p<.05),50 maintaining hobbies such as gaming,49 and active and humorous coping51 which were associated with lower anxiety levels. School-related protective factors for anxiety symptoms included teacher's social support,52 hoping to go back to school (OR=0.6, p<.001), and missing teachers (OR=0.5, p<.001) or classmates (OR=0.6, p<.001).33 Furthermore, protective factors related to the home were: good parent-child relationships (p<.001),32 being accompanied at home on a workday (p<.001),36 living with parents (p=.009),31 and parent-child discussion (OR=0.7, 95%CI=0.6–0.8).44 In addition, being in a romantic relationship (OR=0.4, 95%CI=0.2–0.9)53 and being employed (p=.005)54 were associated with lower anxiety levels (see eTable 4).
DiscussionThis systematic review and meta-analysis provides a large and comprehensive review on the presentation of anxiety symptoms and disorders in children and adolescents. The pooled estimated prevalence of anxiety disorders during the COVID-19 pandemic was 13.0%, and that of anxiety symptoms was 26.5%. This meta-analysis found the prevalence of anxiety disorders during the COVID-19 pandemic to be twice as high as the worldwide prevalence of anxiety disorders before the COVID-19 pandemic.8 Meta-regressions found anxiety symptoms to be significantly more frequent in females. Furthermore, our results suggest that children and adolescents’ anxiety symptoms significantly increased since the onset of the pandemic, in March 2020. Anxiety symptoms were more prevalent in the second wave of COVID-19 than the first wave of COVID-19, more prevalent in young people whose school had closed, and more prevalent in North America and Europe than in Asia and South America. Previous meta-analyses of the COVID-19 period have found the prevalence of anxiety symptoms to be between 28.0%9- 31.0%10 in college students, which is comparable, if not higher, to the figures that this meta-analysis found, suggesting that the increase in anxiety symptoms extends from childhood and adolescence to early adulthood.55 The 26.5% prevalence of anxiety symptoms found in this meta-analysis was higher than that found in a previous meta-analysis (20.5%),6 suggesting that anxiety symptoms kept increasing, up to 29.3%, during the research period from the start of the pandemic in December 2019 until June 2021.
Resilience is our ability to adapt well to adversity and is shaped by individual, familial, and systemic factors.56,57 Typically, young people show high levels of resilience.58 However, resilience in young people may have a limit, with anxiety symptoms increasing from wave 1 to wave 2 of COVID-19. The first wave of the pandemic may have been associated with the fear of the unknown as the developing COVID-19 situation is unpredictable and novel59,60; furthermore, young people may have been exposed to consistently increasing morbidity and infection rates2 alongside anxiety-provoking media.18 With repeated activation of acute stress mechanisms, subsequent waves may be associated with chronic stress,61 post-traumatic stress62,63 and hypochondriasis.59 Children seem to cope better with shorter lockdowns64 and face more mental health difficulties with longer lockdowns,65,66 showing further that resilience in children may have a limit. Furthermore, the mental health difficulties seen with longer lockdowns emphasise that they are only appropriate in emergency cases, due to the negative impacts of social restrictions and their associated stressors. Consequently, children and adolescents should have access to resilience-based interventions,67,68 including the provision of academic skills at the individual level, support for family cohesion, and supportive teacher interactions.69 Further longitudinal research is required on the impact of the COVID-19 pandemic on anxiety in young people to assess if further waves do lead to chronic stress or if young people habituate70 to the unprecedented global situation which may become their new normal.71
School closures resulted in more anxiety symptoms in children and adolescents. One potential hypothesis is that this could be due to parental burnout and limited support from teachers during remote learning,52 alongside difficulty accessing school-based psychological services.72 Children and adolescents from low socioeconomic backgrounds experienced more financial stressors,73 and health risks during the COVID-19 pandemic.74-76 One in seven children were unable to access the internet at home, the rate of which is two times higher in low-income communities77; which may exacerbate social comparison.78 The compounded social and economic difficulties may complexify the transition to remote learning.79 While school closures are effective in controlling COVID-19, the psychological harm for young people could be profound,80 as children face disruptions in school routines.72 Families with low socioeconomic status should be supported with financial safety nets, with schools ensuring all students have access to resources required to get online, to ensure equity. Furthermore, school closures, which are needed for protection, occur during periods of high transmissibility, and may result in more anxiety in young people due to the underlying emphasis on high infection rates. Schools should aim to not overwork students and be mindful of the mental health difficulties vulnerable students are facing.
Our meta-regression analysis showed female sex to be associated with higher levels of anxiety symptoms28-31,33,35-37,42-45,49,50,53,54,81-86 and chances of developing anxiety disorders87 during the COVID pandemic. This seems to be more pronounced during adolescence, coinciding with puberty and a shift in hormones88; females in general are more prone to experiencing anxiety than males.89 Females reportedly face more interpersonal stressors,90 including family, peer, and intimate relationships,91 and were more likely than males to experience increases in interpersonal violence during lockdowns.92 Females also ruminate more,93 which may adversely impact their mental health and could be targeted for early intervention support. Age was not found to be a predictor for anxiety symptoms or disorders in our meta-regression analyses.
Further specific vulnerable groups identified by this systemic review include children and adolescents with neurodevelopmental disorders or Special Educational Needs or Difficulties (SEND),20,23,25 haematological or oncological diseases,22 neurological disorders23,24 or hearing difficulties,21 amongst others. Vulnerable young people have lost both specialised educators52 and a structured learning environment due to the pandemic.77 Children with SEND may experience a delay in the developmental progress of essential skills resulting from a suspension of social groups and therapy sessions.94 Those with chronic illnesses are reported to have higher levels of anxiety during pandemics.95,96 Physical health conditions may affect one's immune system and result in more COVID-19 related anxiety due to the higher risk of vulnerability-based complications during COVID-19.97 Furthermore, as those with chronic physical health conditions already face more disability and non-disability challenges,98 they may experience diminished resilience when facing the additional stressor of COVID-19. Young people with disabilities may also face difficulties in accessing the routine medical care they rely on as healthcare systems are at risk of being overwhelmed by COVID-19, leading to an increase in anxiety.99 Services should attempt to check-in with those known to be medically vulnerable to mediate negative mental health effects because of the chronic and acute difficulties they face.
Children with behavioural problems, pre-existing mental health difficulties, and children who already had a poor relationship with their parents prior to the pandemic are especially vulnerable to an exacerbation of conflicts at home100 which may result in exacerbation of anxiety symptoms.33,46,101 Home is not a safe space for all children99 and schools being shut means children are less able to access safeguarding networks that would be available to them if schools were open.102 Furthermore, studies included in this systematic review found parental stress and anxiety to be risk factors for anxiety symptomatology within children and adolescents.26,27,103 Parents experiencing parental burnout during COVID-19 are more likely to engage in child abuse and neglect,104 posing a short-and-long-term risk for children.105,106 Some parents, for instance, healthcare workers, may be under particular pressure which may result in an exacerbation of anxiety symptoms in children.30,38,107 This is related to long working hours, highly emotive work, and increased potential exposure to COVID-19.108,109
This systematic review found that pre-pandemic anxiety symptoms were predictive of anxiety symptoms severity during the pandemic.46 Having previously accessed psychiatric help is a risk factor for the exacerbation of anxiety symptoms.25 Those known to have previous psychiatric disorders should receive early intervention to help them to cope with expected difficulties and prevent further mental health consequences. Telemental health services have shown to be effective72 and should be adapted to reach vulnerable groups in an extended scope.
This meta-analysis found young people from western continents, including Europe and North America, to report more anxiety symptoms than young people from Asia and South America. Young people from Asia face a range of more severe adverse risks before COVID-19.110 Children and adolescents from high-risk backgrounds are found to show more resilience.111 Furthermore, young people from cities are reported to face more mental health difficulties than those from rural areas.112 There is a lower prevalence of people who use the internet or own a smartphone in Africa, Asia, and South America, in comparison to people from Canada, Australia, or the Netherlands.113 Excessive exposure to COVID-19 related media18,25,34,35 is a risk factor for anxiety symptom exacerbation. Previous research has supported this by showing increased smartphone usage is associated with anxiety levels114 which is more prevalent in western continents. Limiting exposure to media may result in decreased anxiety levels.115 Another hypothesis would be that fear relating to COVID-19 is a risk factor for anxiety symptoms.30-32,36-41,101,116 Since the start of the pandemic, western Europe and North America have had higher rates of COVID-19 community infections, with a higher death rate per million inhabitants, compared to eastern continents and eastern Europe.117 Low-income countries have an estimated infection-fatality rate of 0.23% compared to 1.15% in high-income countries.118 The rate of COVID-19 in the community is associated with more COVID-19 fear and anxiety36 and a lower rate of community COVID-19 cases in low-income countries could explain why there are lower subsequent levels of anxiety. In addition, children from western countries may be more open to report anxiety and communicate their feelings compared to children from eastern countries; this may come from the cultural model of individualism in western cultures more easily allowing individuals to express internal personal characteristics and emotions.119 Furthermore, research has found stressful life events to be perceived as less stressful than breaking cultural taboos120; therefore, there are cultural differences in what is perceived as stressful or anxiety inducing.
More government support is needed to promote recovery. Some studies report disasters to require global and governmental efforts to maintain and restore resilience within society.121,122 This should involve both a rise in funding and the provision of more trained staff to Child and Adolescent Mental Health Services (CAMHS). As COVID-19 is exacerbating young people's mental health and resulting in the emergence of anxiety, the demand on CAMHS, an already stretched service, will grow.74 To prevent further adversity to young people's mental health, we need to provide an adaptable, multi-disciplinary support system74 to protect children and adolescents’ mental health. Furthermore, governmental guidance surrounding disaster regulations and plans should be readily available and easy to understand to maintain resilience in the community.123-125
The COVID-19 pandemic has resulted in a shift in mental health care for young people.126 To ensure continuity of care, mental health services have adopted a telehealth support format.127 Remote interventions have shown good effectivity in anxiety treatment.128 Research has found minimal therapist contact therapies to be efficacious for a range of anxiety diagnoses,129 showing that face-to-face contact may not be essential for therapeutic efficacy.129 Telehealth interventions are cost-effective130 and reduce barriers to care by improving access.131 Telehealth-based psychotherapy has a range of uses within paediatric care132 however, can be limited by one's psychological resistance to novel treatment methods, cultural background, alongside their technology literacy.133 Most reviews looking at the efficacy of remote psychotherapy interventions for anxiety occurred pre-COVID-19. More research including randomised control trials and meta-analyses are needed to evaluate the effectiveness of remote psychotherapy during COVID-19 for children and adolescents so that the best care can be provided.
LimitationsThe findings of this review should be interpreted in the context of various limitations. First, 52.7% of included studies either did not provide clear outcome data or were too heterogeneous or not rigorous enough to be meta-analysed (e.g., the thresholds of the instruments were not in line with validation data). Only four studies provided meta-analysable data regarding anxiety disorders. Second, 87.9% of included studies were from the first wave of COVID-19. More studies on the 2nd and 3rd wave of COVID-19 are needed to evaluate the long-term impact that COVID-19 has on the mental health of young people. Third, 86.5% of included studies were cross-sectional, which limits causal inference. Future longitudinal research should follow those presenting anxiety symptoms during the pandemic to assess if the symptoms presented reduce, continue, or develop into anxiety disorders either as the pandemic continues or post-COVID-19.
ConclusionThis meta-analysis found a high prevalence of anxiety symptoms and the emergence of anxiety disorders in children and adolescents during the COVID-19 pandemic. Specific vulnerable groups include young people in North America and Europe, and females. Identifying those at risk is the first step in developing more appropriate community-based preventative clinical interventions.