The relationship between pain and psychiatric conditions in children and adolescents has been understudied. This study aimed to investigate the influence of gender on the association between pain and psychiatric diagnoses, as well as the specific relationship between pain and attention deficit/hyperactivity disorder (ADHD), in a sample of adolescents from the general population. Additionally, the study explored whether pain frequency or intensity in individuals with ADHD was influenced by coexisting psychiatric disorders and ADHD medications.
MethodsThis cross-sectional study included 1608 conveniently sampled Swedish upper secondary school students aged 15–19 years. Data were collected at the end of 2020 using the electronic "Mental and Somatic Health without borders" survey.
ResultsA significant positive association (p < 0.001) was observed between pain frequency, intensity, and the presence of any psychiatric diagnosis. Female adolescents reported more frequent and intensive pain in the groups with or without any psychiatric diagnosis and in those with ADHD, however the presence of a psychiatric diagnosis had a comparatively lesser impact on pain frequency in females when compared to males. In adolescents with ADHD, pain frequency, but not intensity, showed a significant further increase. Moreover, the presence of coexisting depression and/or anxiety further heightened the association between pain frequency and ADHD. Notably, common ADHD medications did not have a significant impact on pain experiences. Headache emerged as the most prevalent type of pain across all groups of adolescents. Back pain specifically appeared as the next most common type of pain among adolescents with ADHD.
ConclusionThe findings suggest a positive association between pain and the presence of psychiatric diagnoses, including ADHD, in adolescents. Gender modified this association. Back pain arised specifically coupled to ADHD. Common ADHD medications did not show a significant impact on pain experiences in this study. These results highlight the importance of a holistic approach to child and adolescent care.
The co-occurrence of psychiatric conditions and pain presents a significant and intricate issue with substantial implications for clinical practice, research, and public health. This association operates in a bidirectional manner, where chronic pain increases the risk of developing psychiatric disorders, and the presence of psychiatric disorders exacerbates the severity and treatment resistance of chronic pain conditions.1 Gaining a deeper understanding of this co-occurrence is essential for optimizing treatment strategies, unraveling shared underlying mechanisms, improving treatment outcomes, and enhancing functional well-being and quality of life for individuals experiencing both conditions.
Within the realm of pain and psychiatric disorders, much of the focus has centered on mood disorders. The direct correlation between chronic pain, negative affect, and heightened susceptibility to mood disorders2 readily comprehensible. Recent research endeavors have begun to elucidate the underlying mechanisms involved, including the role of the opioid system3 and dopaminergic pathways in the brain.4,5 These findings shed light on the complex interplay between pain and mood disorders and provide insights into the biological mechanisms involved.
Exploring the overlap between psychiatric disorders and chronic pain holds significant importance, particularly considering the involvement of altered dopamine signaling in the development of chronic pain. Dysfunction within the dopaminergic system has been associated with deficits in attention networks, resulting in diminished learning capacity and motivation, as observed in attention deficit/hyperactivity disorder (ADHD).6,7 ADHD is a neurodevelopmental disorder characterized by symptoms of inattention and hyperactivity/impulsivity, with an estimated global community prevalence of 5.6% in teenagers aged 12 to 18.8 Additionally, a notable proportion of children exhibit difficulties with overactivity, inattention, and impulsivity that fall just below the diagnostic threshold for ADHD. Recent research has indicated a link between attention deficits and modified sensory processing, potentially influencing the perception of pain.9,10 Furthermore, a comprehensive review recently examined the occurrence of chronic pain in youth with ADHD, the prevalence of ADHD in individuals with chronic pain, and the intricate connection between chronic pain and ADHD in the younger population.11 Battison and colleagues' review provided a comprehensive overview of the research findings indicating a greater occurrence of ADHD among young individuals experiencing chronic pain, as well as a higher prevalence of chronic pain within samples of youth diagnosed with ADHD. Moreover, additional studies have emphasized the association between childhood ADHD and an elevated risk of developing chronic pain later in adulthood.12 It is important to acknowledge that ADHD often coexists with other psychiatric conditions, including anxiety and depression, which are closely linked to pain.12–14 While these disorders may contribute to the sensitization of pain perception, they alone cannot fully account for the development of pain-related pathologies in individuals with ADHD.
The treatment approach for ADHD often involves the administration of oral methylphenidate, which has the ability to increase dopamine and noradrenaline levels in the brain.15 The impact of methylphenidate on pain perception is not yet fully understood, as studies have reported both alterations in pain sensitivity16,17 and improvements in pain insensitivity.18 In the case of children with ADHD who experience sleep problems after receiving methylphenidate treatment, melatonin may offer a potentially effective and safe solution, regardless of factors such as gender, age, and comorbidities.19 Melatonin possesses both hypnotic and chronobiotic properties, which can influence circadian rhythm sleep disorders. Moreover, melatonin is involved in numerous physiological and pathophysiological processes and exhibits antioxidant, antineoplastic, anti-inflammatory, and immunomodulatory properties. Recent evidence suggests that melatonin plays a significant role in modulating pain through multiple mechanisms.20
In the context of treatment strategies for ADHD, gender specificity was not previously defined. However, notable gender differences exist both in the prevalence and type of ADHD, as well as in the prevalence of chronic pain. ADHD, particularly the hyperactivity/impulsivity-dominant subtype, is more frequently diagnosed in males, whereas the inattentive-dominant subtype is more commonly recognized in females.21 On the other hand, chronic pain, both in the general population22 and psychiatric populations,23 is more frequently reported by females. These gender disparities in ADHD and chronic pain highlight the need for further research and consideration of gender-specific factors in understanding and addressing these conditions.
Building on the scientific background outlined above, the current study aims to examine the relationship between pain and psychiatric conditions, with specific emphasis on ADHD, within a sample of adolescents from the general population. Additionally, we seek to evaluate the previously proposed moderating effect of ADHD medications on pain.
MethodsThe "Mental and Somatic Health without borders" (MeSHe) project, available at https://meshe.se/, follows a cross-sectional, retrospective design. Data used in the present study were collected between September and December 2020 through the electronic MeSHe survey. The survey was primarily distributed via social media platforms in Sweden. Within the electronic MeSHe survey, various validated questionnaires (e.g.: Alcohol Use Disorder Identification Test (AUDIT), Drug Use Disorder Identification Test (DUDIT), Life History of Aggression (LHA), Big Five Inventory (BFI)) were incorporated to evaluate self-reported mental and physical health, risk behaviors, and personality profiles of adolescents. For a detailed description of the MeSHe survey please refer to https://meshe.se/. Participants also provided information on any prescribed medication used, the presence of any psychiatric diagnosis as well as ratings of pain frequency, intensity, and type, experienced over the previous 12 months. These variables were utilized in the resent study. For a detailed description of the data collection process in Sweden, please refer to the study design and procedure section of Sfendla et al., 2023.24
In the present study data from 1608 Swedish upper secondary school students (631 male, 962 female, 15 non-binary), aged 15–19 (mean 17.15) years, were analyzed. Of the 1608 respondents, 27 did not answer the question about the existence of any psychiatric diagnosis and/or pain frequency (1.7% internal attrition rate). Of the remaining 1581 respondents, 311 (19.7%) reported having at least one psychiatric diagnosis. The question about the existence of any psychiatric diagnosis was answered with a “yes,” “no,” or “I do not know” response and, in case of a “yes” response, accompanied by free-text information about the type of diagnosis (or diagnoses).
The respondents were asked if they had suffered from pain during the previous 12 months. Responses to this question were reported on a five-point Likert scale (never, rarely, sometimes, often, all the time). Those who responded anything other than “never” to this question were asked to specify, in free text, the type of pain. Pain intensity was reported on a scale from zero (total absence of pain) to ten (the worst imaginable pain).
StatisticsDescriptive statistics were employed to summarize the characteristics of the sample, while 1000-times bootstrapping with a 95% confidence interval was used to estimate descriptive statistics for the small groups categorized by medication type in adolescents with ADHD. To assess differences between groups, non-parametric tests, namely the Mann-Whitney U and Kruskal-Wallis tests, were employed due to the non-normal distribution of the data. Effect size was reported using η2, calculated as η2 = Z2/(N − 1), where η2 > 0.01 suggests a small effect size and η2 > 0.06 suggests a medium effect size.
Multivariate linear regression analyses were conducted to explore the relationship between pain (dependent variable) and variables including any psychiatric diagnosis, ADHD, gender, and age (independent variables). Additionally, moderation analyses were performed to examine the influence of coexisting psychiatric disorders and ADHD medication on the relationship between ADHD and pain frequency. The statistical analyses were conducted using SPSS version 28 (IBM). The significance level was set at p < 0.05.
ResultsOf the 1581 respondents, 311 (19.7%) reported having at least one psychiatric diagnosis. In the free text, 87 (28% of those with psychiatric diagnoses; 5.5% of the study population) indicated the existence of an ADHD or attention-deficit disorder diagnosis (with or without coexisting psychiatric disorders). These 87 respondents are referred to herein as a group of adolescents with ADHD. The most frequent comorbidities were depression (22%, n = 19) and/or anxiety (12%, n = 10) and autism spectrum disorder (10%, n = 9).
Headache emerged as the most frequently reported type of pain in both the general population and among adolescents with any psychiatric diagnosis or ADHD, accounting for 49.56%, 55.31%, and 51.72% respectively. Additionally, joint pain (18.10% and 27.89%) and abdominal pain (14.73% and 18.97%) were the next most common types of pain in the general population and among those with any psychiatric diagnosis. In the subgroup of adolescents with ADHD, following headache, back pain (24.14%) and joint pain (19.54%) were the most commonly reported types.
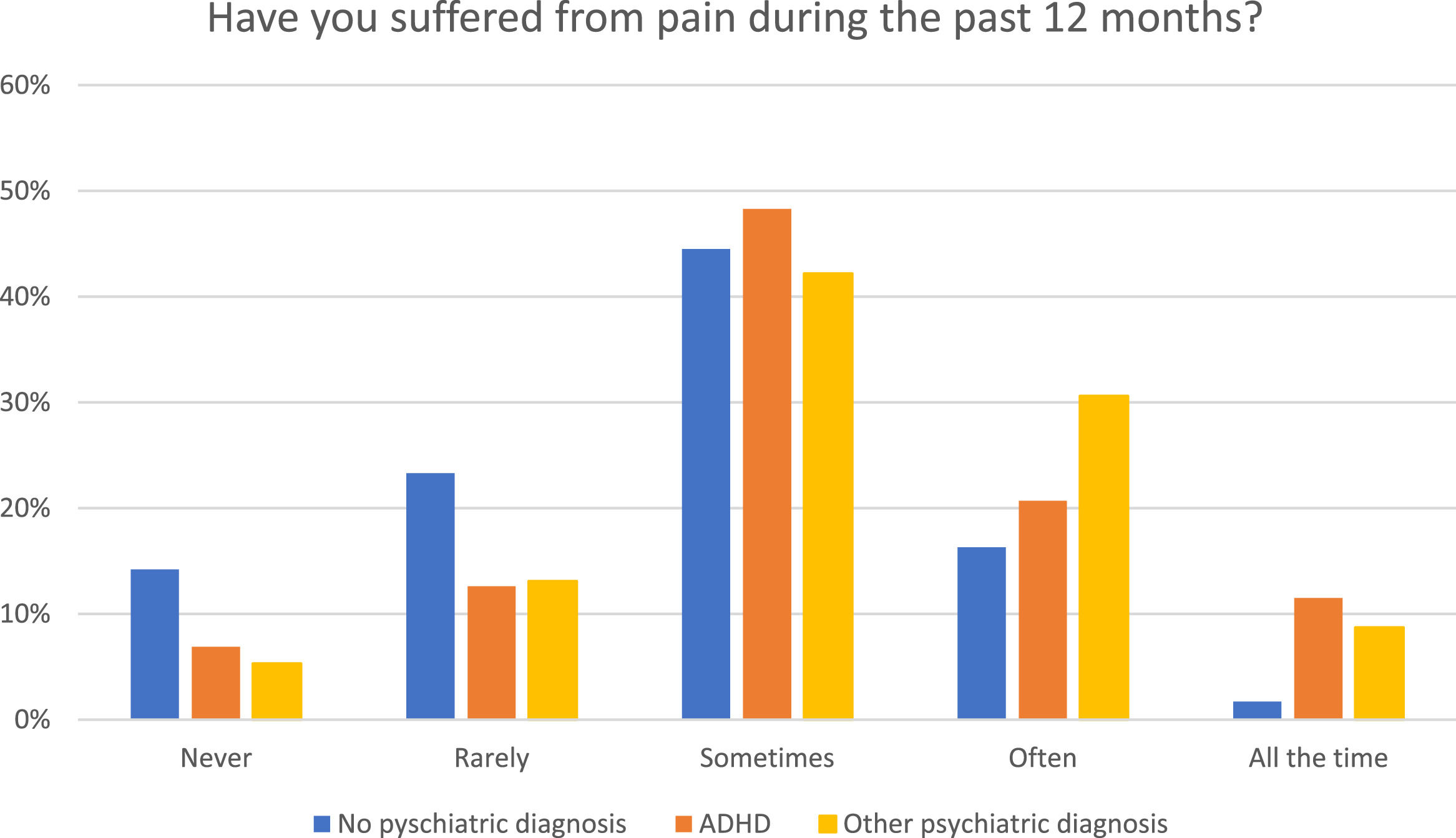
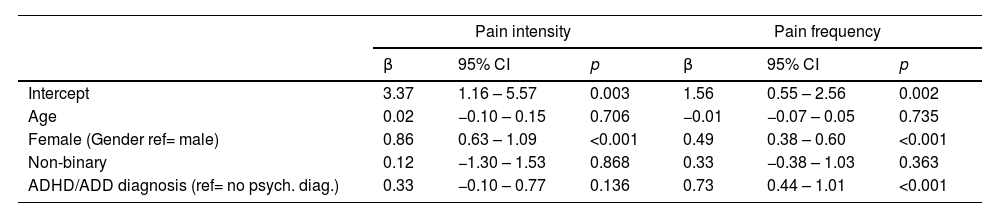
Adolescents who reported having any psychiatric diagnosis also reported a significantly (p < 0.001) higher frequency (Fig. 1) and greater intensity of pain. The observed differences in pain intensity and frequency were of small effect size, as indicated in Table 1.
Descriptive statistic of pain scores in the groups of respondents with and without any psychiatric diagnosis.
| Adolescents reporting no psychiatric disorder | Adolescents reporting psychiatric disorder(s) | p* | η2 | |
|---|---|---|---|---|
| Pain frequency M/Md (SD) | 1.68/2 (0.97) | 2.20/2 (0.99) | <0.001 | 0.042 |
| Pain Intensity M/Md (SD) | 3.95/4 (2.20) | 4.62/5 (2.08) | <0.001 | 0.014 |
p* = significance level calculated with the non-parametric Mann–Whitney U test; η2 =effect size.
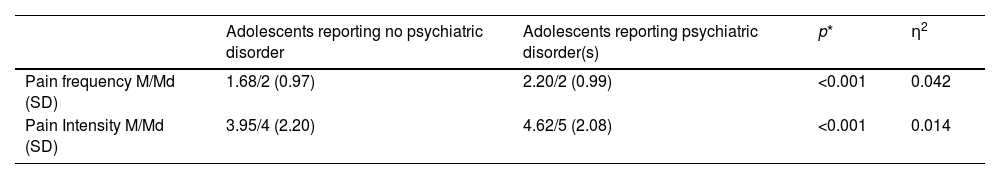
Gender significantly moderated the association between pain and the presence of psychiatric diagnosis. Females with psychiatric diagnosis reported a significantly higher frequency of pain (p = 0.045) and significantly greater pain intensity (p < 0.001) compared to their male counterparts, but age (between 15 and 19) did not impact these associations significantly.
These associations are proven also in a multivariate linear regression of pain frequency on pain intensity, adjusted for age, gender and presence of psychiatric diagnosis (Table 2). When investigating genders impact on the association between pain and the existence of psychiatric diagnosis, a negative association was found for female gender, indicating that the effect of psychiatric diagnosis on pain frequency is weaker for females compared to males (Table 2).
Association between pain frequency and intensity.
β = coefficient of multiple linear regression model; CI=95% Confidence Interval.
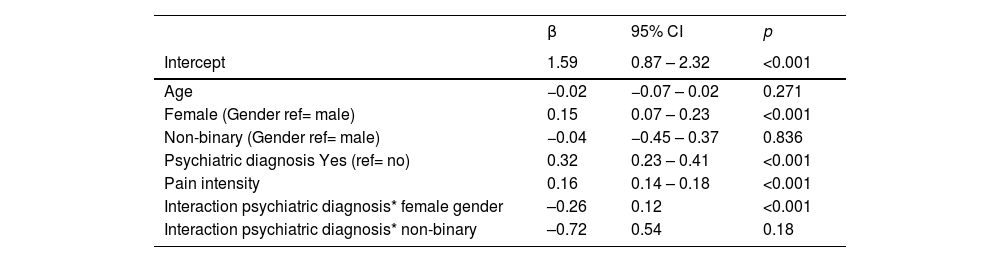
When analyzing pain frequency and intensity specifically in relation to the presence of ADHD, it was found that only pain frequency was significantly increased in individuals reporting ADHD (Table 3). Females with ADHD reported a significantly higher frequency of pain (p < 0.001) and significantly greater pain intensity (p < 0.001) compared to males. When investigating genders impact on the association between pain and ADHD diagnosis, no significant association was found (data not shown). Furthermore, the increase in pain frequency among those with ADHD was even stronger compared to individuals reporting any psychiatric diagnosis (β = 0.73, CI = 0.44–1.01, p < 0.001 for ADHD vs β = 0.32, CI = 0.23–0.41, p < 0.001).
Association between ADHD and pain frequency or intensity.
β = coefficient of multiple linear regression model; CI=95% Confidence Interval.
When ADHD coexisted with depression and/or anxiety, pain frequency increased significantly (β = 0.71, CI = 0.25–1.17, p = 0.003), but pain intensity did not (β = 0.43, CI = –0.56–1.42, p = 0.39). The coexistence of autism spectrum disorder with ADHD did not seem to modify the association between pain frequency (β = –0.11, CI = –0.72–0.51, p = 0.73) or pain intensity (β = 0.29, CI = –0.98–1.56, p = 0.65) and ADHD.
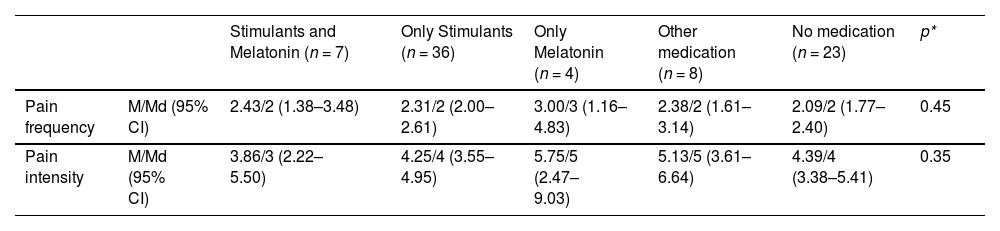
Almost one third (28.7%, n = 25) of the adolescents who reported the presence of ADHD diagnosis did not take any medication. One respondent reported to take medication but did not specify the type of it and nine adolescent received other type of psychiatric medication (SSRI and/or anxiolytics). More than half (55.1%, n = 48) were receiving pharmacological treatment with stimulants. A small proportion (14.9%, n = 13) had received hypnotic medication/melatonin as part of their treatment. In our analyses, neither pain frequency nor pain intensity was changed significantly by any of the aforementioned medications or their combination (Table 4).
Descriptive statistics, including 95% confidence intervals (CI), were calculated using 1000 bootstrapping iterations to analyze pain intensity and frequency among different medication groups in adolescents with ADHD.
p* = significance level calculated with Kruskal- Wallis non-parametric test; n is based on the response about pain intensity and frequency and type of the medication.
The results of this study reinforce the interconnectedness between mental and somatic health by demonstrating a significant association between the presence of any psychiatric diagnosis and increased frequency and intensity of pain in adolescents from the general population. This finding aligns with previous research indicating that individuals with psychiatric diagnoses may be more susceptible to experiencing pain symptoms.25,26 It is noteworthy that female adolescents, not only in this study but in other studies as well27–29 tend to report more frequent and intense pain. We observed a positive association between female gender and both pain intensity and frequency across the general population, individuals with any psychiatric diagnosis, and those with ADHD. However, our interaction analysis shed light on an interesting aspect: the influence of psychiatric diagnosis on pain frequency is less pronounced among females when compared to males. In simpler terms, the presence of a psychiatric diagnosis has a relatively smaller impact on pain frequency among females than it does among males.
Considering the type of pain, headache was reported as the most frequent pain in the general sample and those with any psychiatric diagnosis or those with ADHD. The prevalence of headache in our population, approximately 50%, aligns with findings from a previous systematic review encompassing 50 population-based studies.30 Notably, while joint pain and abdominal pain were the subsequent commonly reported types among individuals with or without any psychiatric diagnosis, back pain emerged as the next most frequent reason for pain among adolescents with ADHD. This increased prevalence of back pain among adolescents with ADHD may serve as a potential predictor of the previously reported association between ADHD and fibromyalgia.12
The increase in pain frequency, but not in pain intensity, among individuals with ADHD (compared to those with any psychiatric diagnosis) draws attention to the complex and multifactorial nature of pain prevalence within this population. The overlapping cognitive and behavioral processes shared by ADHD and chronic pain, as well as the potential involvement of neuroinflammation and/or central sensitization, may contribute to this relationship.29,31 Genetic factors and intergenerational recurrence of ADHD and/or chronic pain may contribute to the observed risk factors.11 An increasing amount of research shows the associations between ADHD and modified pain experiences in children and adolescents.11 Our study, conducted on a sample from the general population, highlights that adolescents with ADHD report significantly higher pain frequency compared to those without psychiatric diagnosis and those with psychiatric diagnosis other than ADHD. These findings underscore the need for an improved and holistic approach in the clinical assessment and treatment of children and adolescents with ADHD, particularly regarding pain management.
The findings of this study provide further support for the well-established association between anxiety/depression and chronic pain. Previous research has suggested that ADHD may mediate this relationship.13,14,15 Our study adds to this understanding by demonstrating that when anxiety/depression co-exists with ADHD in adolescents, it leads to an additional increase in pain frequency. Interestingly, while previous studies have reported a strong association between autism spectrum disorder and altered pain perception32 our study did not find any significant impact of autism spectrum disorder co-existing with ADHD on pain frequency or intensity. Further research is warranted to investigate the underlying mechanisms and potential variations in pain experiences among individuals with ADHD, anxiety/depression, and autism spectrum disorder. This research will contribute to the development of tailored interventions for improved pain management in this specific population.
Finally, the question regarding the impact of ADHD medication on pain experience in adolescents. In our study, we observed that approximately one-third of adolescents diagnosed with ADHD do not receive or use any medication for their condition. Among those who do receive and use medication, more than half are prescribed stimulants, while a smaller proportion are prescribed melatonin or SSRI/anxiolytic treatments alone or in combination with stimulants. Surprisingly, our findings indicate that none of these medications or their combinations have shown a significant impact on pain experience in adolescents with ADHD. Our results warrant further research to explore the potential mechanisms underlying the lack of significant medication effects on pain in adolescents with ADHD. Additionally, studying alternative non-pharmacological approaches for managing pain in this population may be beneficial.
Strengths and limitationsThe present study, like any scientific study, possesses both strengths and limitations. One of the notable strengths is the considerable size of the study population, comprising over 1500 adolescents aged 15 to 19 from the general population. Although the sample was not representative of all Swedish secondary upper high school students due to convenient sampling, responses were obtained from all 21 counties of Sweden, including participants from various locations and schools. The MeSHe study, of which this research is a part, initially aimed to investigate international cultural risk and protective factors in adolescents' behaviors, mental and somatic health (www.meshe.se . In early 2020, the MeSHe survey was utilized to assess the impact of COVID-19 pandemic on the psychosocial functioning of adolescents.33 For the present study, we focused solely on data from Sweden, as it is well-known that mostly due to cultural differences among raters, ADHD diagnosis often lack cross-cultural stability,34 which could present a significant limitation if a multinational study population were used for the analyses. Importantly, the survey incorporates a salutogenic perspective, addressing both unhealthy and healthy aspects, which ensures the inclusion of individuals who are both healthy and experiencing illness. The prevalence of ADHD in our study population was 5.5%, aligning with the reported prevalence of ADHD among 12- to 18-year-old adolescents in a scoping international review, which reported a prevalence of 5.6%8. This indicates that the cohort has good validity, providing the opportunity of drawing reliable conclusions and generalizing the results to a larger population.
However, it is important to acknowledge the limitations inherent in the study design and data collection methods. One limitation is the use of convenient sampling, which may affect the generalizability of the results. While the findings may be applicable to Swedish adolescents and potentially to Scandinavian countries with similar ADHD investigation procedures and physician rating preferences, caution should be exercised when generalizing the results to other populations.
Another potential limitation is the inability to determine if the experience of pain was influenced by the COVID-19 restrictions. However, it is important to note that any impact of the restrictions would likely affect all adolescents, regardless of their ADHD diagnosis. In previous publications, we reported that Swedish adolescents did not specifically report a worsening of their everyday life33 or increased psychological distress35 during the COVID-19 pandemic. Another limitation of the study is the reliance on self-reported measures of pain intensity and frequency over the course of the past 12 months. However, it is important to note that the survey did not include assessments of how pain impacted participants' functioning and quality of life, factors that could potentially be influenced by both ADHD and ADHD medications. These limitations should be taken into consideration when interpreting the study findings and generalizing them to broader populations.
Future research with more diverse samples and rigorous study designs would provide a more comprehensive understanding of the relationship between psychiatric diagnoses, ADHD, pain experiences, and additional contextual factors.
ConclusionIn summary, our study found that adolescents with any psychiatric diagnosis, especially ADHD, experience increased pain frequency. Headache stands out as the most prevalent type of pain, with back pain being the subsequent commonly reported type among adolescents diagnosed with ADHD. Females exhibit a stronger association with pain, while the presence of a psychiatric diagnosis has a relatively smaller impact on pain frequency among females than it does among males. Coexisting anxiety/depression further amplifies pain frequency in those with ADHD. Medications commonly used for ADHD treatment have no significant effect on pain. These findings underscore the importance of taking a holistic approach in assessing and managing ADHD in adolescents.
Ethical considerationsThe National Ethics Review Board has approved this project (registration numbers 689–17 and 2020–03351). Completion of the anonymous electronic survey was voluntary.