Acute liver failure (ALF) is a rare complication of malignant liver infiltration with a high mortality. In the largest case series reported in the literature, with 4020 ALF cases of multiple etiologies, malignant infiltration was only responsible for 0.44%1. The diagnosis of malignant liver infiltration as the etiology of ALF is a clinical challenge, occurring with breast cancer, small cell lung cancer, lymphoma, melanoma and myeloma2.
A 50-year-old man presented with a two-week history of lumbar pain and malaise. He had a past history of hypertension, a daily alcohol intake of 30g and 40 pack-year history of smoking. Other behavioral risk factors, recent travel, use of new drugs or herbalist products were excluded.
Physical examination revealed hepatomegaly and right upper quadrant tenderness. Initial laboratory workup showed leukocytosis (22.7×109/L), normal platelet count (127×109/L), bilirubin (0.8mg/dL), alkaline phosphatase (110U/L), gamma-glutamyl transferase (95U/L) and international normalized ratio (INR) (0.88) but an elevated aspartate aminotransferase (AST) (194U/L), alanine aminotransferase (ALT) (130U/L) and lactate dehydrogenase (LDH) (1663U/L). Abdominal ultrasound confirmed hepatomegaly. He was admitted with the diagnosis of acute hepatitis of unknown etiology.
HIV, viral hepatitis and autoimmune markers were negative. Lipid profile, protein electrophoresis, ceruloplasmin and α1-antitrypsin levels were also normal.
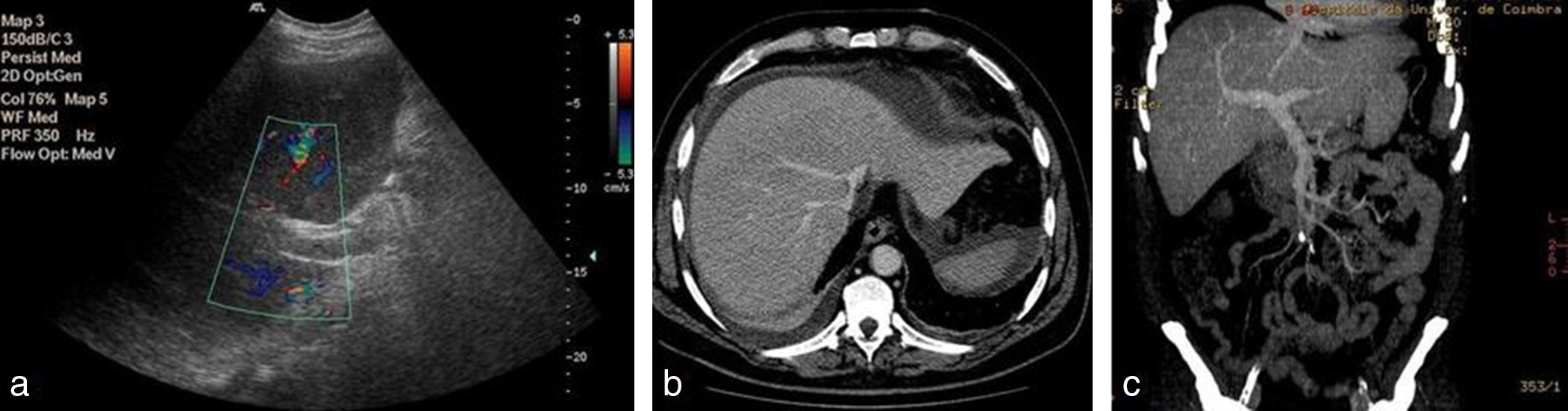
Seven days after admission, he developed jaundice and rapid deterioration of liver function (INR 1.76, bilirubin 6mg/dL, AST 872U/L, ALT 492U/L, LDH 3325U/L). Doppler abdominal ultrasonography demonstrated increased portal vein caliber and very low portal blood flow. Subsequent abdominal computed tomography angiography showed hepatomegaly and perihepatic peritoneal effusion (Fig. 1).
Imagiology. Abdominal ultrasound with doppler: the portal vein with doppler color showed no visible flow with the scaled velocity of 5.3cm/s (image a). Abdominal computed tomography angiography demonstrated hepatomegaly, mild perihepatic peritoneal effusion and permeability of portal and suprahepatic veins (image b and c).
Eight days after admission he developed encephalopathy and respiratory failure requiring mechanical ventilation. As the clinical picture remained elusive a transjugular liver biopsy was performed. Over the following day he fulfilled King's College criteria and liver transplantation was decided, but the patient died intraoperatively.
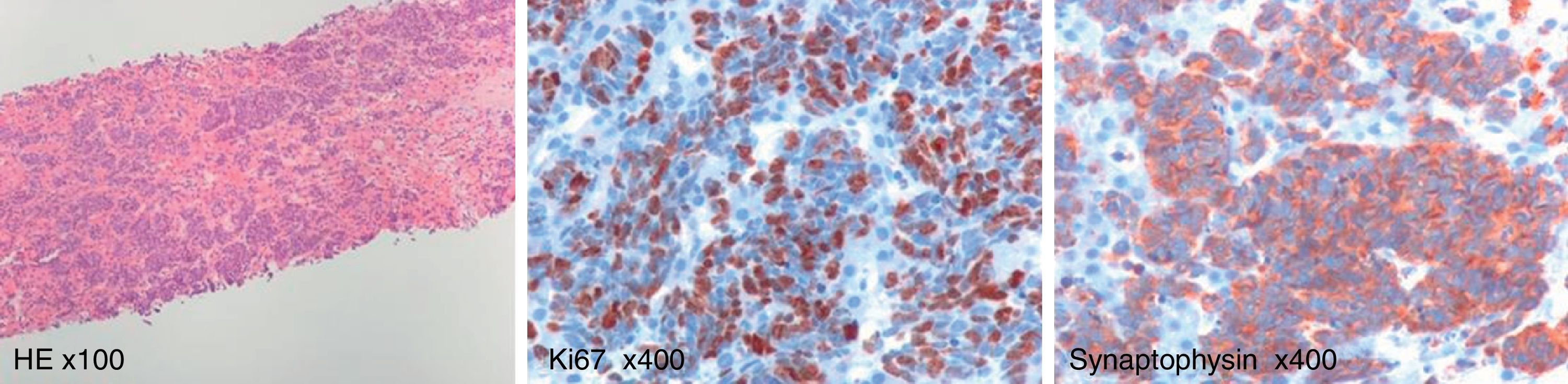
The final diagnosis was made postmortem by the result of transjugular liver biopsy revealing a poorly differentiated neuroendocrine tumor of unknown primary site (Fig. 2).
Malignant infiltration is a rare cause of ALF and difficult diagnosis requiring a high degree of suspicion, especially if there is no history of primary malignant disease. In more than half of the cases with ALF due to malignant infiltration, cancer was not diagnosed before the development of ALF3. The clinical presentation is not specific and there is an absence of the classical imaging findings consistent with liver metastases, because of the histological pattern of microinvasion3. The massive sinusoidal infiltration and hepatic vessels obstruction by tumor cells result in ischemia and hypoxic hepatocellular necrosis1,3. We have a short window for investigation since most of these patients die soon after admission4. The diagnosis is frequently made by postmortem liver histology.
The majority of neuroendocrine tumors of unknown primary site are poorly differentiated carcinomas with aggressive biology5. These cancers are characterized by multiple sites of metastases and rarely produce symptoms related to secretion of bioactive substances. In addition to the liver, common metastatic sites include bone, lung and brain. Small cell neuroendocrine tumors with metastases, frequently originate in the lungs. Diagnosis of these neuroendocrine tumors depends on immunohistochemical staining for chromogranin and/or synaptophysin.