Extramedullary plasmacytomas are uncommon plasma cell neoplasms which account for 3–4% of these tumors.1 The presence of extramedullary plasmacytoma associated to multiple myeloma (MM) occurs in 4–7% of patients.2 Gastrointestinal involvement may appear in up to 10% of the cases, usually involving the liver and, less frequently, the pancreas.2 In a recent review of patients with MM, only 50 reported cases of pancreatic plasmacytomas (PP) were diagnosed as part of a clinical progressive course of the disease in majority of these cases.3 There are very few cases reported of PP as a manifestation of MM relapse. We report a case of a man with previous history of MM who developed obstructive jaundice due to PP as a manifestation of MM relapse.
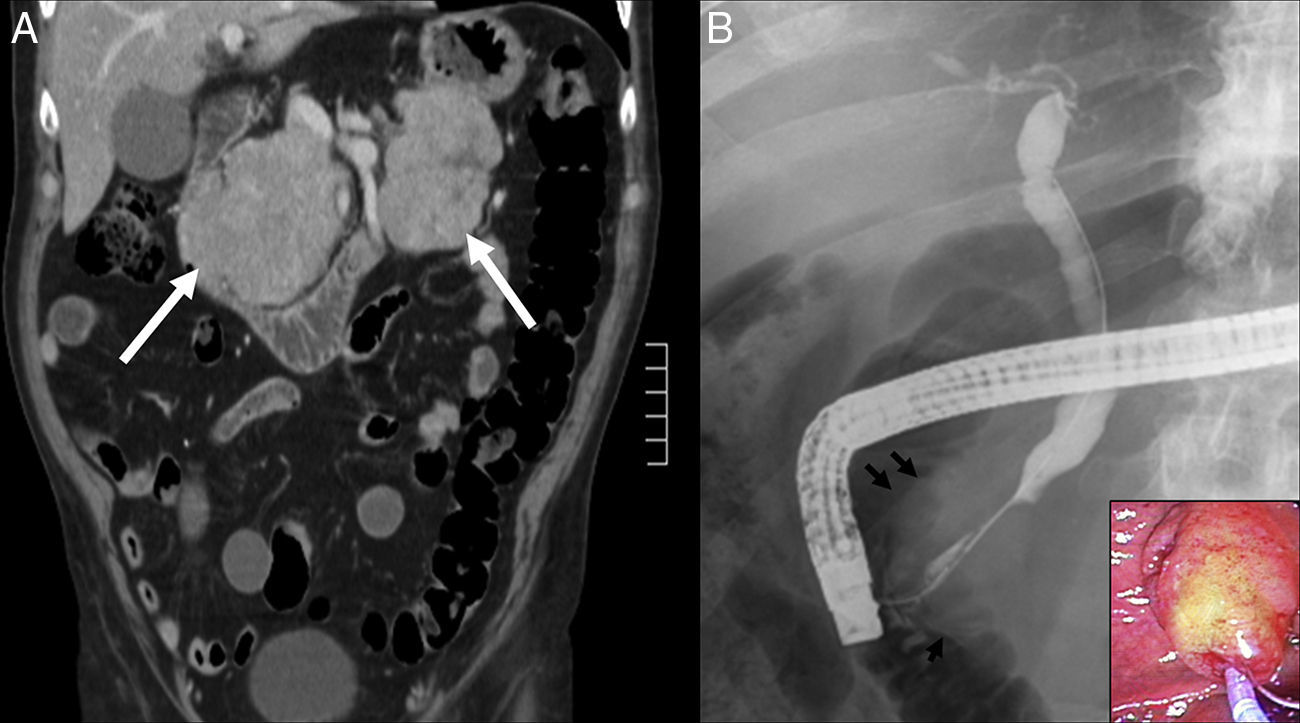
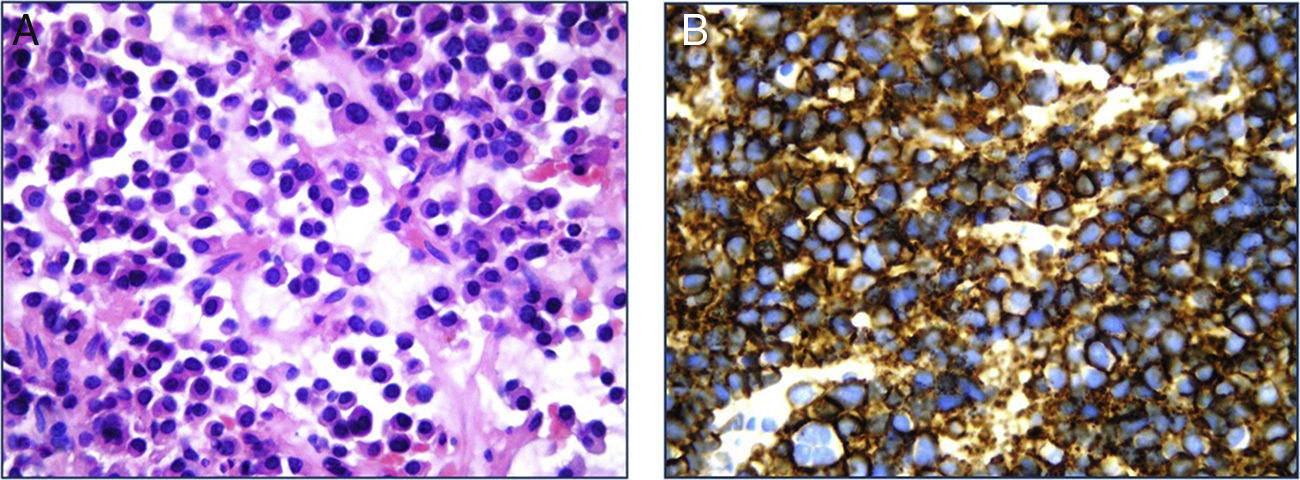
A 70-year-old man with a previous history (3yrs prior) of stage IIA MM was admitted to the hospital with jaundice. Previous bone marrow aspiration showed 12% plasma cells and lambda light chains were present on serum immunofixation (IF). Serum protein analysis was normal and there was no proteinuria. Urine IF was negative. Treatment with dexamethasone and thalidomide was started with complete response. A follow-up evaluation one year later showed no evidence of bone marrow involvement (bone marrow aspiration was normal and serum/urine IF were negative). Four weeks before admission, he complained of jaundice, anorexia and weight loss (approximately 8kg). Diabetes mellitus with insulin requirement was diagnosed three weeks before admission. On examination, he was afebrile, and alert and oriented. His abdominal exam revealed a palpable nodular mass localized in the right upper quadrant. Laboratory tests showed serum bilirubin level of 17.2mg/dl (normal range<1.2mg/dl), aspartate aminotransferase 98U/l (normal range<37U/l), alanine aminotransferase 227U/l (normal range<41U/l), gamma glutamil transpeptidase 1087U/l (normal range<49U/l) and alkaline phosphatase 1106U/l (normal range 91–258U/l). Serum lipase and amylase values were within normal values. An abdominal computed tomography (CT) revealed common bile duct dilatation (10mm) and a pancreatic mass (8.6cm×6.2cm) located in the pancreatic head and nodular lesions in the pancreas tail. Peripancreatic lymph nodes (>1cm) were also present, but there were no signs of vascular invasion or liver involvement (Fig. 1A). Carcinoembryonic antigen levels were 5.4ng/ml (normal value<5ng/ml) and CA19-9 levels were 266IU/ml (normal value<37IU/ml). Endoscopic retrograde cholangiopancreatography (ERCP) showed a diffuse increase of the size of the major duodenal papilla with ulcerated mucosa (Fig. 1B). The cholangiogram showed a 30mm stricture in the distal common bile duct with proximal biliary dilatation. Multiple biopsies from the papillary region were taken and a 10cm, 10Fr plastic stent was inserted across the stricture. The pathological study showed a neoplastic plasma cell infiltration (Fig. 2A). A CT-guided needle biopsy of the pancreatic head mass confirmed the findings of the papillary biopsies. Plasma cells were CD138 positive and showed lambda light chain monoclonal expression (Fig. 2B). Proliferation index, assessed with Ki67, was 40% and the neoplastic cells exhibited p53 expression in a 50%. PP secondary to MM was diagnosed. Treatment with lenalidomide, cyclophosphamide and dexamethasone was started with good clinical and analytical response. After three months, liver tests were normal and an abdominal CT showed a significant reduction of the pancreatic head mass and disappearance of the tail lesions. ERCP performed four months after the initial presentation jaundice showed resolution of the biliary stricture.
Extramedullary plasmacytomas are rare tumors that can occur either as a manifestation of MM (secondary tumors) or as a primary lesion (primary tumors).2 About 80% of the extramedullary plasmacytomas develop in the upper respiratory tract; however, other sites such as the gastrointestinal tract may also be involved. Extramedullary plasmacytomas are frequently diagnosed in advanced stages of MM and are associated with poor prognosis.4
Pancreatic involvement by plasma cell neoplasms is very infrequent, accounting for less than 0.1% of pancreatic masses.3 PP occur most commonly in the sixth and seventh decades of life and have a male predominance (3:1).1 In a series of autopsies of 57 patients with known MM, PP was found in only 2% of the cases.2 Most of the PP are single lesions, although two o more concurrent lesions may occur.3 There are very few cases reported in the literature of PP as a manifestation of MM relapse. Fischer et al. described a similar case in whom PP of the head of the pancreas was the main manifestation of MM relapse.5 Furthermore, in two cases PP was diagnosed in association to other extramedullary plasmacytomas localized in the stomach or at the spinal canal.6,7 Finally, PP was reported as the only clinical manifestation of MM relapse in two patients after an initial response with autologous stem cell transplantation.8,9
The differential diagnosis of PP includes pancreatic adenocarcinoma, neuroendcrine tumors, lymphoma and amyloidosis. Endoscopic ultrasound-guided fine needle aspiration or percutaneous biopsy can be helpful to confirm the pathological diagnosis. However, as described in this case, biopsies from the papillary region during ERCP allow a less invasive approach in cases with papillary involvement. The use of ERCP in the diagnosis of PP has not been reported.10 In our knowledge, this is the first case that PP was diagnosed with biopsies at ERCP.
Treatment of biliary obstruction secondary to PP should include endoscopic stent placement and a size reduction therapy of the pancreatic mass.3 Plasma cells tumor are highly radiosensitive and chemosensitive. In secondary PP, therapeutic options include chemotherapy, radiation therapy, or a combination of both. Prognosis is more favorable in primary PP than in secondary PP. The presence of extramedullary involvement in MM at any time of its evolution is associated with a more aggressive course.3
In conclusion, we present the case of a patient that developed a PP as a manifestation of MM relapse. Obstructive jaundice due to a biliary stricture improved with biliary stenting and chemotherapy. Although symptomatic involvement of the gastrointestinal tract in patients with MM is infrequent, PP should be considered in the differential diagnosis in patients with known MM and a pancreatic mass.