Chronic diarrhoea (lasting for more than 4–6 weeks) is relatively common among the general population. The main causes according to pathogenesis are shown in Table 1. It is essential to take a detailed medical history and perform a thorough physical examination to adequately manage this disorder, since this makes it possible to screen for patients requiring more detailed tests and examinations.
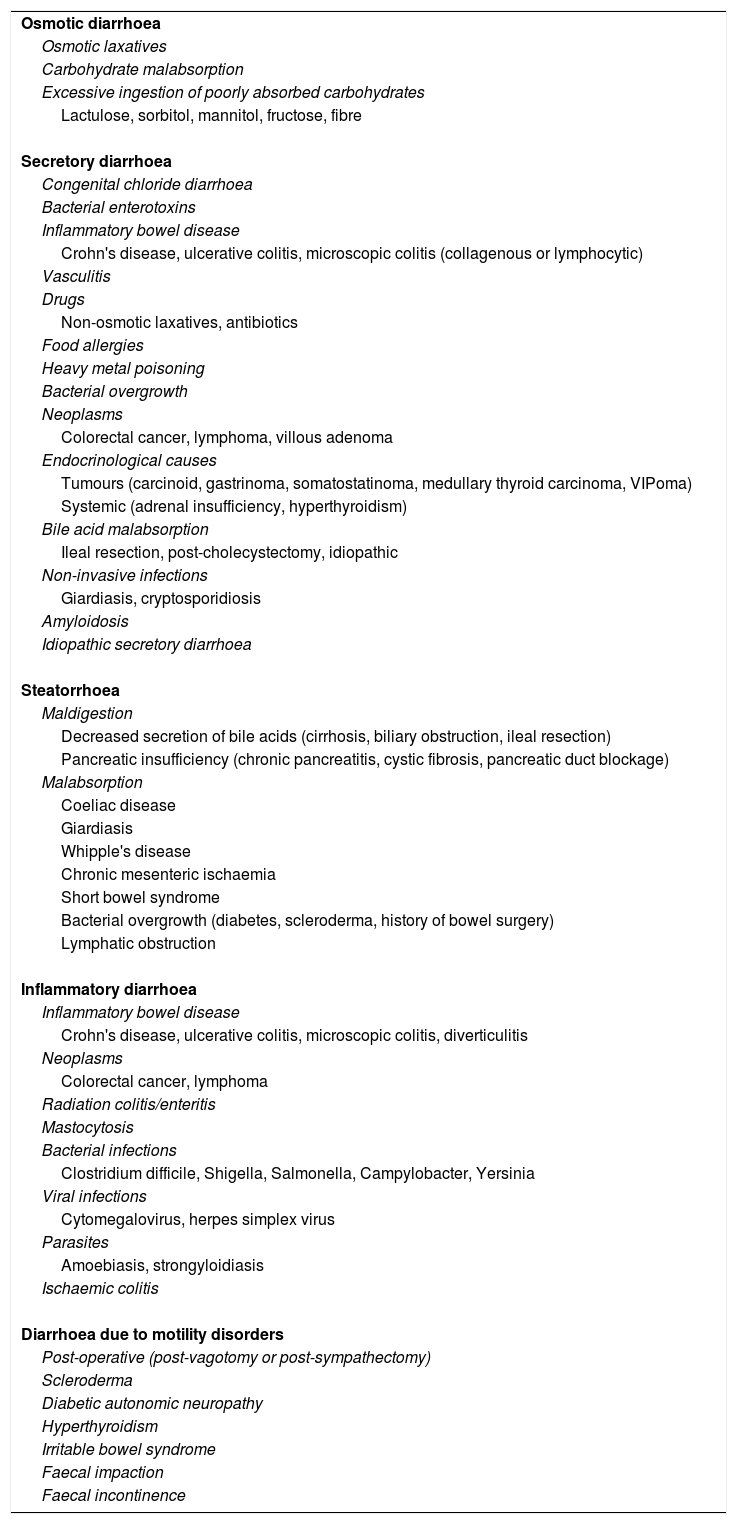
Causes of chronic diarrhoea according to pathogenesis.
| Osmotic diarrhoea |
| Osmotic laxatives |
| Carbohydrate malabsorption |
| Excessive ingestion of poorly absorbed carbohydrates |
| Lactulose, sorbitol, mannitol, fructose, fibre |
| Secretory diarrhoea |
| Congenital chloride diarrhoea |
| Bacterial enterotoxins |
| Inflammatory bowel disease |
| Crohn's disease, ulcerative colitis, microscopic colitis (collagenous or lymphocytic) |
| Vasculitis |
| Drugs |
| Non-osmotic laxatives, antibiotics |
| Food allergies |
| Heavy metal poisoning |
| Bacterial overgrowth |
| Neoplasms |
| Colorectal cancer, lymphoma, villous adenoma |
| Endocrinological causes |
| Tumours (carcinoid, gastrinoma, somatostatinoma, medullary thyroid carcinoma, VIPoma) |
| Systemic (adrenal insufficiency, hyperthyroidism) |
| Bile acid malabsorption |
| Ileal resection, post-cholecystectomy, idiopathic |
| Non-invasive infections |
| Giardiasis, cryptosporidiosis |
| Amyloidosis |
| Idiopathic secretory diarrhoea |
| Steatorrhoea |
| Maldigestion |
| Decreased secretion of bile acids (cirrhosis, biliary obstruction, ileal resection) |
| Pancreatic insufficiency (chronic pancreatitis, cystic fibrosis, pancreatic duct blockage) |
| Malabsorption |
| Coeliac disease |
| Giardiasis |
| Whipple's disease |
| Chronic mesenteric ischaemia |
| Short bowel syndrome |
| Bacterial overgrowth (diabetes, scleroderma, history of bowel surgery) |
| Lymphatic obstruction |
| Inflammatory diarrhoea |
| Inflammatory bowel disease |
| Crohn's disease, ulcerative colitis, microscopic colitis, diverticulitis |
| Neoplasms |
| Colorectal cancer, lymphoma |
| Radiation colitis/enteritis |
| Mastocytosis |
| Bacterial infections |
| Clostridium difficile, Shigella, Salmonella, Campylobacter, Yersinia |
| Viral infections |
| Cytomegalovirus, herpes simplex virus |
| Parasites |
| Amoebiasis, strongyloidiasis |
| Ischaemic colitis |
| Diarrhoea due to motility disorders |
| Post-operative (post-vagotomy or post-sympathectomy) |
| Scleroderma |
| Diabetic autonomic neuropathy |
| Hyperthyroidism |
| Irritable bowel syndrome |
| Faecal impaction |
| Faecal incontinence |
This article looks at the case of a 36-year-old male with no notable medical history who started with diarrhoea with 3–4 stools a day, some during the night, without blood, mucus or pus. He had no abdominal pain, nausea, vomiting or fever. His symptoms were not related to meal times, and he showed no improvement, despite a lactose-free diet. On physical examination, his abdomen was soft, non-tender and with no palpable masses or organomegaly.
A full blood count and stool culture were ordered, both of which were within the normal ranges. Due to the persistence of symptoms for 4 months and the presence of nocturnal bowel movements, the patient was assessed by the digestive diseases department. A colonoscopy and endoscopy were ordered, revealing only the presence of erosive gastritis; the patient was found to be Helicobacter pylori positive. The patient took antibiotic treatment for H. pylori eradication, but symptoms persisted.
A broader study was ordered including an abdominal ultrasound. Numerous nodular hyperechoic liver lesions were observed that are compatible with metastasis. Therefore, a CT scan of the chest and abdomen was performed. The CT scan showed the same liver nodules, osteoblastic bone lesions and a thyroid nodule, all of which is indicative of a neuroendocrine tumour (Fig. 1).
More blood tests, including tumour marker tests, were ordered, showing very high calcitonin (38,653ng/l, normal range 0–18.2) and carcinoembryonic antigen levels (1065ng/ml, normal range 0–5.4). For better characterisation of the thyroid nodule, an ultrasound of the neck was performed which showed a lesion in the left thyroid lobe measuring 37mm with ultrasound characteristics of malignancy. It also showed the presence of multiple swollen lymph nodes in the central, ipsilateral and contralateral compartments of the neck.
A biopsy of this nodule and one of the lymph nodes was compatible with medullary thyroid carcinoma (MTC) and, therefore, RET proto-oncogene mutation and urinary catecholamine and metanephrine tests were ordered due to the possibility of pheochromocytoma in the event of multiple endocrine neoplasia. The genetic study revealed a heterozygous RET mutation at pC618R. Urinary catecholamines and metanephrines were normal, which ruled out the concomitant presence of pheochromocytoma.
In view of these results, it was decided to perform a total thyroidectomy and removal of lymph nodes from the neck in order to prevent local symptoms and facilitate future treatments. Histological examination confirmed multifocal, bilateral MTC with vascular and lymphatic invasion.
After being assessed by the oncology department, it was decided to complete treatment with tyrosine kinase inhibitors.
Twelve months after surgery, tumour markers have remained stable, and the disease has not progressed in imaging studies.
For the initial management of chronic diarrhoea, it is essential to look for warning signs or symptoms, such as blood in the stool, fever, weight loss, family history of cancer, nocturnal diarrhoea or diarrhoea that persists even during fasting or hepatosplenomegaly.1
Neuroendocrine tumours account for less than 1% of causes of chronic diarrhoea, and, therefore, do not tend to be considered during initial screening. It may therefore be several years before a diagnosis is reached.2 MTC is a neuroendocrine tumour that originates from the C cells or parafollicular cells of the thyroid gland and accounts for 1–2% of all thyroid cancers.3 Although diarrhoea is a relatively common symptom of MTC, it does not tend to be the first manifestation of the tumour since the appearance of a mass in the neck is the most common symptom. The mechanism that causes diarrhoea is fundamentally fluid and electrolyte secretion, induced by various peptides (calcitonin, serotonin, VIP),2,4 although there may also be an increase in intestinal motility.
Initial screening tests for these tumours include an ultrasound of the neck.5 The most sensitive diagnostic test is the cytologic smear using a fine-needle aspiration biopsy with positive staining for calcitonin, chromogranin A and carcinoembryonic antigen.6 Plasma calcitonin and carcinoembryonic antigen levels are useful for diagnosing and monitoring this type of tumour.7 Calcitonin, although not a specific marker, also correlates with the extent of the disease.8
In 75% of cases, MTC is sporadic, while in 25% of cases it is hereditary. It is generally associated with multiple endocrine neoplasia and hereditary MTC due to RET proto-oncogene mutation. This mutation should be studied in all patients diagnosed with this type of tumour, and appropriate genetic counselling should be provided.9,10
This is an interesting case because chronic diarrhoea was the patient's only symptom, but a diagnosis of metastatic MTC was reached. A detailed medical history and a thorough physical examination are essential to determine which patients require complementary examinations and tests.
Please cite this article as: Ernaga Lorea A, Migueliz Bermejo I, Eguílaz Esparza N, Hernández Morhain MC, Pineda Arribas J. Diarrea crónica: el primer síntoma de un carcinoma medular de tiroides metastásico. Gastroenterol Hepatol. 2018;41:105–107.