Eating disorders (ED) constitute an important group of conditions that commonly occur in adolescents. Gastrointestinal complaints are frequently reported in ED patients. Few studies assessed the association of irritable bowel syndrome (IBS) with ED. The aim of the current study is to determine the prevalence of ED in a group of IBS patients and compare it with a healthy control group and assess the relationship of IBS sub-types, it's duration and severity with ED.
Patients and methods100 IBS patients diagnosed according to the Rome-IV criteria and a control group consisting of 100 healthy adults, between 18 and 65 years old, were enrolled in this study. Sub-type, duration and severity of IBS were determined. All participants were requested to fill questionnaires to screen for ED.
Results200 subjects participated in the study. 118(59%) were female and 92(41%) were male. The Eating Attitudes Test (EAT) score was significantly higher in the IBS group (Odds ratio: 5.3 CI 95%:4.3–9.3; p<0.001). The number of subjects with EAT score >30 was significantly higher in the IBS group (p<0.001). EAT scores were significantly higher in female IBS patients and in younger patients (p=0.013 and p=0.043; respectively). No significant association between the IBS sub-type and EAT score was found (p>0.05). However, IBS severity and duration positively correlated with EAT scores.
DiscussionED should be considered in the management of IBS patients. Since many psychological factors can exacerbate IBS symptoms a multidisciplinary approach consisting of medical and behavioral therapeutic modalities should be employed for a better management of these patients.
Los trastornos de la alimentación (TA) constituyen un grupo importante de afecciones que suelen aparecer en adolescentes. Los pacientes con TA refieren con frecuencia molestias abdominales. La asociación del síndrome de colon irritable (SCI) con los TA se ha evaluado en un número reducido de estudios. El objetivo del estudio actual es determinar la prevalencia de los TA en un grupo de pacientes con SCI y compararla con un grupo de control sano para evaluar la relación de los subtipos de SCI, así como su duración e intensidad con los TA.
Pacientes y métodosEn este estudio se incluyeron 100 pacientes con SCI diagnosticados según los criterios Rome-IV y un grupo de control compuesto por 100 adultos sanos de entre 18 y 65 años. Se determinaron el subtipo, la duración y la intensidad del SCI. Se pidió a todos los pacientes que cumplimentaran cuestionarios de detección de TA.
ResultadosEn el estudio participaron 200 sujetos. Ciento dieciocho (59%) eran mujeres y 92 (41%) eran varones. La puntuación en las pruebas de actitudes alimentarias (Eating Attitudes Test [EAT]) fue significativamente superior en el grupo de SCI (cociente de probabilidades: 5,3; IC del 95%: 4,3-9,3; p<0,001). El número de sujetos con puntuación de EAT>30 fue significativamente superior en el grupo de SCI (p < 0,001). Las puntuaciones de EAT fueron significativamente superiores en pacientes mujeres con SCI y en pacientes más jóvenes (p=0,013 y p=0,043, respectivamente). No se halló una asociación significativa entre el subtipo de SCI y la puntuación de EAT (p>0,05). Sin embargo, la intensidad y la duración del SCI presentaron una correlación positiva con las puntuaciones de EAT.
DiscusiónEl TA debe tenerse en cuenta en el tratamiento de los pacientes con SCI. Puesto que muchos factores psicológicos pueden exacerbar los síntomas del SCI, deberá emplearse un enfoque multidisciplinar compuesto por modalidades terapéuticas médicas y conductuales para un mejor tratamiento de estos pacientes.
Irritable bowel syndrome (IBS) is a functional disorder of the gastrointestinal system characterized by abdominal pain, abdominal discomfort and alteration of bowel habits. The complex pathogenesis of IBS is thought to involve abnormal bowel motility, visceral hypersensitivity, inflammation, disorders of the hypothalamic-pituitary-adrenal axis, brain-gut axis and pain modulation centers which may be caused by abnormal autonomic activity and emotional factors.1 The prevalence of IBS in Europe is thought to be around 11.5%.2 This ratio is estimated between 6.2 and 19.1% in Turkey.2 Diet restriction and excessive eating were reported to occur more commonly in IBS patients (15.7%) compared to the general population.3
Eating disorders (ED), are a major health issue that ED increase patients’ mortality risk by affecting their psychosocial and medical conditions.4,5 Although the etiologic factors of this entity remain controversial, many mechanisms were proposed to play a role in its pathogenesis; these include: disorders in serotonergic, monoamine and neurotransmitter systems, obstetric complications, exposure to environmental factors during childhood, genetic factors and other psychiatric disorders.5
Besides affecting almost every organ system, the most severe symptoms of ED usually occur in the gastrointestinal system. Many studies reported an increased incidence of abdominal pain, nausea, vomiting, constipation, bloating and abdominal distension in these patients.6 In a study that enrolled 101 ED patients, Body et al. identified at least one functional gastrointestinal disorder (FGID) in 98% of the cases.7 Similarly, another study reported a 68.8% prevalence of IBS in ED patients.8 The relationship between IBS and ED and the association of these disorders with a higher incidence among females, patients having a history of physical or sexual abuse, anxiety, depression, personality disorders and other psychiatric disorders is not well understood.9 Both, duration of gastrointestinal symptoms and severity of IBS positively correlate with the prevalence of psychiatric disorders. Currently, controversial data regarding the relationship of ED with subtypes of IBS is available.1,10
Few studies explored the relationship of ED with IBS diagnosed using the Rome III diagnostic criteria,11 but there is no study diagnosed using the Rome IV diagnostic criteria in Turkey. The primary objective of this study is to determine the prevalence of ED in a group of IBS patients and compare it with a healthy control group. Secondary objectives are to identify the predisposing factors for developing ED in IBS patients, assess the relationship between ED and the predominant subtype of IBS, duration of IBS complaints and severity of IBS symptoms.
MethodsStudy populationOur study was conducted between June 2016 and September 2016 in the Bezmialem Vakıf University Hospital. The study included 100 IBS patients aged between 18 and 65 years who were under follow up at our gastroenterology outpatient clinic. A control group consisting of 100 healthy individuals was also included in the study. Our study was designed prospectively. Consent was taken for all participants to be included in the study. The subjects were examined by a gastroenterologist and afterwards they were evaluated for somatoform disorders by a psychiatrist.
Diagnosis of IBSIBS diagnosis was made based on the Rome IV criteria (complaints must be started at least 6 months before diagnosis and abdominal pain at least 1 day per week during the last 3 months or abdominal discomfort at least 1 day per week during the last 3 months, associated with at least two of the finds accompanying the change (1. pain relieved by defecation 2. altered stool frequency 3. change in stool form)).12
Inclusion criteriaThe medical history was taken and physical examination was performed. Routine studies (fasting glucose, urea, creatinine, liver functional tests, total bilirubin, albumin, prothrombin time, total cholesterol, low density cholesterol, triglycerides, complete blood count, C-reactive protein, erythrocyte sedimentation rate, thyroid functional tests, hemoglobin A1c, fecal occult blood test, microscopic examination of the stool for parasites, stool helicobacter pylori antigen) were obtained. Healthy volunteers who applied to the hospital for general health screening and who did not find any pathology in the examinations and routine biochemical tests were taken as control group. Patients with normal physical examination and routine biochemical tests and diagnosed with IBS by the gastroenterologist were included in the study.
Exclusion criteriaPatients with anemia, fever, persistent diarrhea, refractory constipation, rectal bleeding, weight loss, abnormal physical examination findings, nocturnal pain and defecation, family history of inflammatory bowel disease and celiac disease, history of bowel cancer, symptoms starting after the age of 50 years were not enrolled in the study. Pregnant and lactating women, patients below 18 and over 65 years old, patients with documented gastrointestinal disease (stomach-duodenal ulcer, gastric cancer, small and large intestine cancer, inflammatory bowel disease, gastroparesis, chronic intestinal ischemia, etc.) or pancreaticobiliary, hepatobiliary, systemic and psychiatric disorders, patients with history of major abdominal surgery and alcohol addiction were excluded from the study.
The type and severity of IBSIBS predominant sub-type was determined using the Bristol stool scale.13 Patients were divided into three groups: diarrhea, constipation and alternating groups. If the constipation rates were more than 25% and the diarrhea rates were less than 25% in all defecations, the patients were defined as constipation-predominant IBS; if the diarrhea rates were more than 25% and constipation rates were less than 25%, the patients were defined as diarrhea-predominant IBS; and if the constipation rates were more than 25% and diarrhea rates were also more than 25%, the patients were defined as mixed-type IBS.14 The duration of symptoms was recorded. The severity of the disease was determined using the Irritable Bowel Syndrome Score Questionnaire and it was reported as mild, moderate or severe.15
Eating attitudes and behaviorsEating attitudes and behaviors were evaluated using the Eating Troubles Module (EAT-26). This module is based on the Eating Attitude Test (EAT).16 Although it does not yield a specific diagnosis, the EAT-26 is a widely used standardized measure of the severity of the symptoms frequently seen in ED. The cut-off EAT score suggesting a possible ED is >30.16 The EAT score was divided into four groups: <10, 10–20, 20–30, and >30. The relationship between groups and IBS subtype, IBS symptom severity, and IBS duration were examined.
Ethics statementEthical approval was received from the Ethical Committee of the Hospital for the study. All procedures were in line with the ethical standards of the committee on human experimentation of our institution and with Helsinki Declaration.
Data analysisThe data was analyzed using the NCSS (Number Cruncher Statistical System, LLC Kaysville, Utah, USA) program. Descriptive statistical methods (mean, standard deviation, median, frequency and ration) were used to evaluate the data. Student's t-test was used to compare normally distributed parameters and Mann–Whitney U test was used to compare non-normal distributed variables. Person's analysis was used to evaluate correlation between variables. Pearson's chi-squared test, Yates Continuity Correction test, Fishers Exact test and Fisher Freeman Halton test were used to compare categorical variables. Variables with p value <0.05 or within the 95% confidence interval were considered statistically significant.
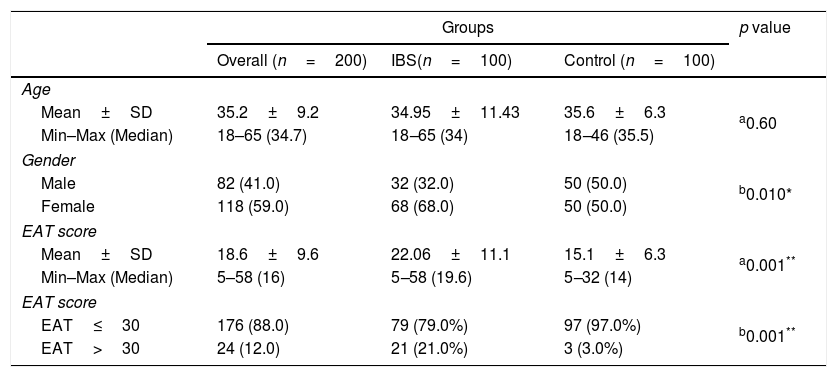
ResultsA total of 200 subjects were enrolled in this study. 41% (n=92) were male and 59% (n=118) were female. The proportion of females in the control group was significantly smaller than the IBS group (50% vs. 68%, respectively; p<0.001). The ages of the participants varied between 18 to 65 years. The overall mean age was 35.2±9.2 years. The mean age of the participants was 35.6±6.3 years (range: 18-55) in the control group and 34.9±11.4 years in the IBS group (range: 18–65). The mean EAT score was significantly higher in the IBS group (odds ratio: 5.3 CI: 95%: 4.3–9.3; p<0.001). The number of patients with an EAT score >30 was significantly higher in the IBS group (p<0.001) (Table 1).
Demographic characteristics and Eating Attitude Test scores of the study groups.
| Groups | p value | |||
|---|---|---|---|---|
| Overall (n=200) | IBS(n=100) | Control (n=100) | ||
| Age | ||||
| Mean±SD | 35.2±9.2 | 34.95±11.43 | 35.6±6.3 | a0.60 |
| Min–Max (Median) | 18–65 (34.7) | 18–65 (34) | 18–46 (35.5) | |
| Gender | ||||
| Male | 82 (41.0) | 32 (32.0) | 50 (50.0) | b0.010* |
| Female | 118 (59.0) | 68 (68.0) | 50 (50.0) | |
| EAT score | ||||
| Mean±SD | 18.6±9.6 | 22.06±11.1 | 15.1±6.3 | a0.001** |
| Min–Max (Median) | 5–58 (16) | 5–58 (19.6) | 5–32 (14) | |
| EAT score | ||||
| EAT≤30 | 176 (88.0) | 79 (79.0%) | 97 (97.0%) | b0.001** |
| EAT>30 | 24 (12.0) | 21 (21.0%) | 3 (3.0%) | |
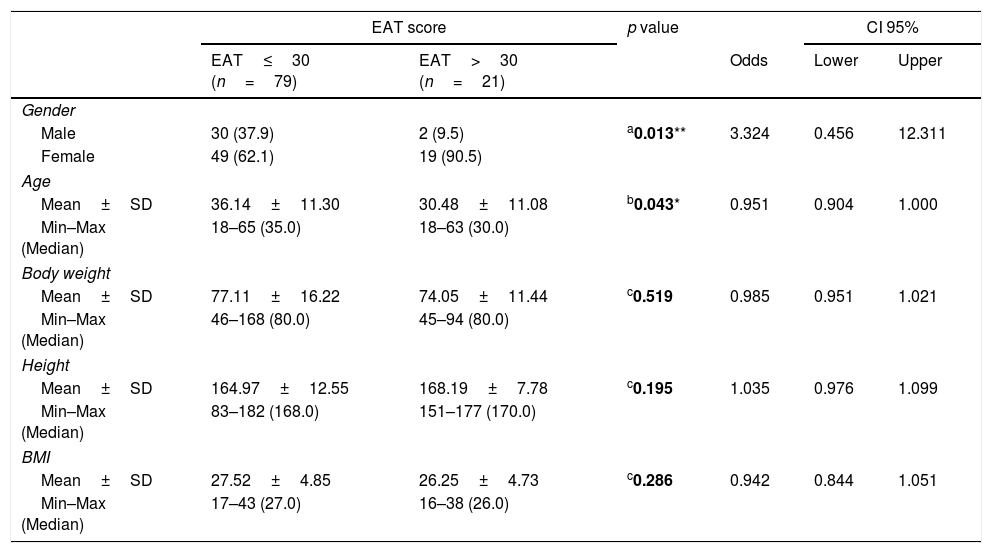
Assessment between EAT score with gender and age distributions; A significantly higher number of females (p=0.013) and young patients (p=0.043) were found in the group of IBS patients with EAT score >30. No statistically significant difference in body weight, height or BMI was found between patients according to their EAT scores (p>0.05) (Table 2).
Demographic characteristics of IBS patients according to Eating Attitude Test scores.
| EAT score | p value | CI 95% | ||||
|---|---|---|---|---|---|---|
| EAT≤30 (n=79) | EAT>30 (n=21) | Odds | Lower | Upper | ||
| Gender | ||||||
| Male | 30 (37.9) | 2 (9.5) | a0.013** | 3.324 | 0.456 | 12.311 |
| Female | 49 (62.1) | 19 (90.5) | ||||
| Age | ||||||
| Mean±SD | 36.14±11.30 | 30.48±11.08 | b0.043* | 0.951 | 0.904 | 1.000 |
| Min–Max (Median) | 18–65 (35.0) | 18–63 (30.0) | ||||
| Body weight | ||||||
| Mean±SD | 77.11±16.22 | 74.05±11.44 | c0.519 | 0.985 | 0.951 | 1.021 |
| Min–Max (Median) | 46–168 (80.0) | 45–94 (80.0) | ||||
| Height | ||||||
| Mean±SD | 164.97±12.55 | 168.19±7.78 | c0.195 | 1.035 | 0.976 | 1.099 |
| Min–Max (Median) | 83–182 (168.0) | 151–177 (170.0) | ||||
| BMI | ||||||
| Mean±SD | 27.52±4.85 | 26.25±4.73 | c0.286 | 0.942 | 0.844 | 1.051 |
| Min–Max (Median) | 17–43 (27.0) | 16–38 (26.0) | ||||
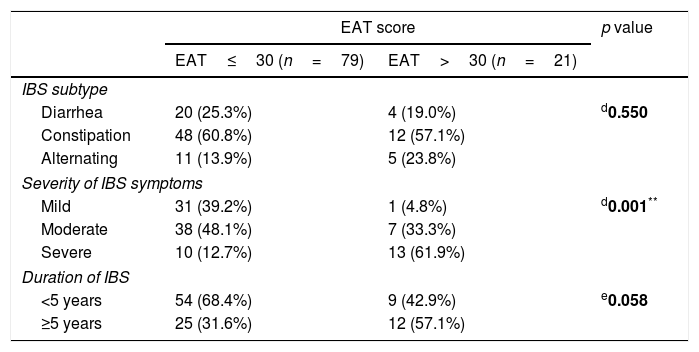
While there was no statistically significant difference between the IBS types (p<0.01) of the cases, a statistically significant difference was detected between the IBS severity distributions of the cases according to the EAT Score (p=0.001; p<0.01). While the mild IBS rates of the cases who had EAT scores at or below 30 was significantly high (p=0.006; p<0.01); the IBS severity was significantly high in cases who had EAT score higher than 30 (p=0.001, p<0.01). The rate of IBS being over 5 years in the cases with EAT score more than 30 was determined to be higher although not at a statistically significant level than the cases with EAT score at or below 30 (p=0.058, p>0.05). The odds value of the effect of the IBS time on the EAT score was determined as 2.88 (CI 95%: 1.075–7.718) (Table 3).
Characteristics of IBS patients according to Eating Attitude Test scores.
| EAT score | p value | ||
|---|---|---|---|
| EAT≤30 (n=79) | EAT>30 (n=21) | ||
| IBS subtype | |||
| Diarrhea | 20 (25.3%) | 4 (19.0%) | d0.550 |
| Constipation | 48 (60.8%) | 12 (57.1%) | |
| Alternating | 11 (13.9%) | 5 (23.8%) | |
| Severity of IBS symptoms | |||
| Mild | 31 (39.2%) | 1 (4.8%) | d0.001** |
| Moderate | 38 (48.1%) | 7 (33.3%) | |
| Severe | 10 (12.7%) | 13 (61.9%) | |
| Duration of IBS | |||
| <5 years | 54 (68.4%) | 9 (42.9%) | e0.058 |
| ≥5 years | 25 (31.6%) | 12 (57.1%) | |
In the examination which was made by dividing the EAT scores into four groups (EAT scores: 0≤10, 10–20, 20–30, >30), no statistically significant differences were detected between the groups in terms of having IBS-type diarrhea (p>0.05); however, a statistically significant difference was detected between having IBS-type constipation and the groups (p=0.015; p<0.05). The rate of detecting constipation-type in the cases with EAT score between 20 and 30 was found to be statistically significant higher in the cases with an EAT score between 0–10, 10–20 and over 30 level (respectively; p=0.032; p=0.003; p=0.030; p<0.05). A statistically significant difference was detected between having IBS-type alternant and groups (p=0.010; p<0.05). The rate of detecting alternant-type in the cases with EAT score between 20-30 was found to be statistically significant lower in the cases with an EAT score between 10–20 and over 30 level (p=0.004; p=0.012; p<0.05) (Table 4).
Characteristics of the IBS patients according to Eating Attitude Test scores.
| EAT score | dp | ||||
|---|---|---|---|---|---|
| EAT 0≤10 | EAT 10-20 | EAT 21-30 | EAT > 30 | ||
| IBS subtype | |||||
| Diarrhea | 5 (38.5%) | 11 (28.2%) | 4 (14.8%) | 4 (19.0%) | d0.337 |
| Constipation | 7 (53.8%) | 18 (46.2%) | 23 (85.2%) | 12 (57.1%) | b0.015* |
| Alternating | 1 (7.7%) | 10 (25.6%) | 0 (0.0%) | 5 (23.8%) | d0.010* |
| Severity of IBS symptoms | |||||
| Mild | 6 (46.2%) | 14 (35.9%) | 11 (40.7%) | 1 (4.8%) | d0.011* |
| Moderate | 6 (46.2%) | 22 (56.4%) | 10 (37.0%) | 7 (33.3%) | b0.272 |
| Severe | 1 (7.7%) | 3 (7.7%) | 6 (22.2%) | 13 (61.9%) | d0.001** |
| Duration of IBS | |||||
| <5 years | 9 (69.2%) | 23 (59.0%) | 22 (81.5%) | 9 (42.9%) | d0.043* |
| ≥5 years | 4 (30.8%) | 16 (41.0%) | 5 (18.5%) | 12 (57.1%) | |
A statistically significant difference was detected between the rates of the cases with mild IBS severity according to the EAT scores (p=0.011; p<0.05). In the cases with EAT score more than 30, the rate of having IBS severity mild was determined to be lower at a statistically significant level compared to the cases with EAT scores 0–10, 10–20 and 20–30 (p=0.007; p=0.019; p=0.012; p<0.05). According to the EAT scores, no statistically significant difference was detected between the cases with moderate IBS severity (p>0.05). According to the EAT scores, a statistically significant difference was detected between the rates of severe IBS cases (p=0.001, p<0.01). The severity of IBS severity in cases with EAT score more than 30 was higher at a significant level than the EAT score of the cases with 0–10, 10–20 and 20–30 (p=0.006; p=0.001; p=0.013; p<0.05) (Table 4). A statistically significant difference was detected between the IBS times of the cases according to the EAT scores (p=0.043; p<0.05). In the cases with EAT scores more than 30, the IBS time being five and more years was detected to be higher at a significant level compared to the cases whose EAT scores were between 20 and 30 (p=0.013; p<0.05) (Table 4).
DiscussionIn our study we determine the prevalence of ED in a group of IBS patients and compare it with a healthy control group, reviewed the predisposing factors for developing ED in IBS patients, and assess the relationship between ED and the predominant subtype of IBS, duration of IBS complaints and severity of IBS symptoms. Our study is very important that relationship of ED with IBS diagnosed using the Rome IV diagnostic criteria. Because there is no study diagnosed using the Rome IV diagnostic criteria. We take care of the age distribution were similar in two groups. The proportion of females in the control group was significantly smaller than the IBS group. The mean EAT score was significantly higher in the IBS group and the number of patients with an EAT score >30 was significantly higher in the IBS group. A significantly higher number of females and young patients were found in the group of IBS patients with EAT score >30. Also there are positive correlation was found between the IBS subtype, severity of gastrointestinal symptoms, duration of the IBS, and EAT scores.
The prevalence of IBS in patients with ED is higher compared to the general population.17–19 Studies reported that at least one ED is diagnosed in 5.3–44.4% of patients presenting with gastrointestinal complaints.17 Guthire et al. demonstrated that EAT score was significantly higher in patients diagnosed with IBS compared to patients with organic disorders.18 In our study, the mean EAT score and the proportion of subjects having an EAT >30 were significantly higher in the IBS patient group compared to the control group. There is a strong association between IBS and ED but the extent to which they affect each other is unknown. A study following up patients being treated for ED showed that at the end of the one year-treatment, the IBS symptoms improved in 23% of the patients, did not change in 22%, while 12% of the cohort developed IBS symptoms during the follow up.19 Body at al. reported that the FGID symptoms persisted in 77% of the patients diagnosed with ED after they were treated and signs of improvement were recorded.7
Several studies reported the presence of some physiological abnormalities, such as abnormal esophagus activity, delayed gastric emptying, prolongation of gastrointestinal transit period, abnormal hormonal and neurotransmitter activity in ED patients.3 Studies using electrogastrography and manometry reported dysmotility of the stomach and esophagus in these patients. Partial improvement in dysmotility was also noticed after treating ED.6 Duration of bowel transit, measured using the radioisotope technique, was significantly longer in ED patients compared to the normal population.6 Additionally, mega duodenum and duodenal immobility were reported to have an impact on the course of this entity.6 Constipation seen in ED patients was attributed to bad nutrition, prolonged colon transit time, electrolyte imbalances and metabolic myopathy caused by continuous use of laxatives.6,20 It was suggested that a decrease in the hormones synthesized by the brain-gut axis (such as cholecystokinin) may contribute to constipation via an unknown mechanism.6,20 Stress is an important predictor for both IBS and ED. Exacerbation of IBS symptoms often causes the patients to restrict their diet which may provoke ED symptoms. Food rich in carbohydrates and fat consumed by ED patients leads to exacerbation of IBS symptoms. These data demonstrate the close relation between these two disorders.
ED occur more commonly in young women and adolescents, however, BMI has not been associated with these disorders.3,5,9 Perkins et al. reported no relationship between BMI and the prevalence or severity of ED.21 Body et al. could not demonstrate a significant association between BMI and the presence of FGID before or after treating ED.19 Similarly, our study showed a significantly higher EAT score in women and young adolescents, and no impact of BMI on the prevalence of ED was found. The reason why women are more prone to develop ED is unknown. Biological and social factors are thought to play a role the etiology of this entity. In young adolescents, biological factors (hormonal imbalances and abnormalities in the brain synapsis), social factors, such as stress, the idealization of being thin, family history of depression and alcoholism and early menarche were proposed as predisposing factors for ED.5
Studies examining the relationship between ED and the severity of gastrointestinal symptoms yielded controversial results. Sainbury et al. reported that the severity of gastrointestinal symptoms was a predictive factor for development of ED. On the other hand, Tang et al. found no relationship between symptom severity and prevalence of ED.9,22 In our study, a significant positive correlation was found between the severity of gastrointestinal symptoms and ED score. Several hypotheses were proposed to account for this relationship. Especially, some overweight patients with severe gastrointestinal symptoms do not restrict their diet but consume food that triggers ED. One study reported that some patients with severe gastrointestinal symptoms who were on a strict diet developed ED. This study suggested that food restriction and having the patients consume nutrients they disliked caused anxiety which provoked the onset of ED symptoms.17 Even though no clear evidence of the relationship between IBS and ED is present, our study found a positive correlation between the duration of the IBS and the presence of psychiatric disorders.10 Studies investigating the relationship between IBS sub-type and psychiatric disorders reported conflicting results.6,10 Some studies did not find a significant association between IBS sub-type and ED.9,18 Similarly, our study could not show such a relationship.
Especially in patients with gastrointestinal dysfunction such as abnormal esophageal activity, delay in gastric emptying, prolongation in gastrointestinal transit, developing secondary to eating disorder, correction of the pathological mechanisms occurring with correction of the eating disorder can be achieved. In addition, it will be contributed to the correction of psychiatric diseases such as anxiety secondary to edible foods. As a result of the correction of the underlying pathological mechanisms, it may be thought that the symptoms and severity of IBS may improve.
ConclusionAs a result, IBS and psychiatric disorders should be treated concomitantly. Several psychological factors lead to exacerbation of IBS symptoms. Thus, a multidisciplinary approach with a combination of medical and behavioral treatments is mandatory. Attention should be given not only to IBS symptoms and their severity but also to treatment of the coexisting ED. Management of behavioral pathologies, like vomiting, continuous laxative use and refusal to eat may help the patient achieve an optimal body weight. This may also help treating any underlying psychiatric disorder which facilitates controlling IBS symptoms.
Financial disclosureNo financial support was received.
Conflict of interestsThe authors declare that they have no conflict of interest.