Primary eosinophilic gastrointestinal disorders are a group of rare clinical entities (except for eosinophilic oesophagitis), with a broad clinical spectrum. We believe this case is of interest due to the fact that there are few published cases at the patient's age, and the seriousness of her initial signs and symptoms.
A 15-year-old female patient was admitted due to vomiting and abdominal pain for the last 3 months that had worsened in the last 48h, accompanied by tetany of all 4 limbs and retrosternal pain.
Her personal history included gastrointestinal symptoms classified as a possible eating disorder with epigastralgia, leading to different consultations. She did not ingest toxins, take drugs or have any purging behaviours. She was diagnosed with Helicobacter pylori infection with a breath test and treated with triple therapy. She had no relevant allergies or familial diseases.
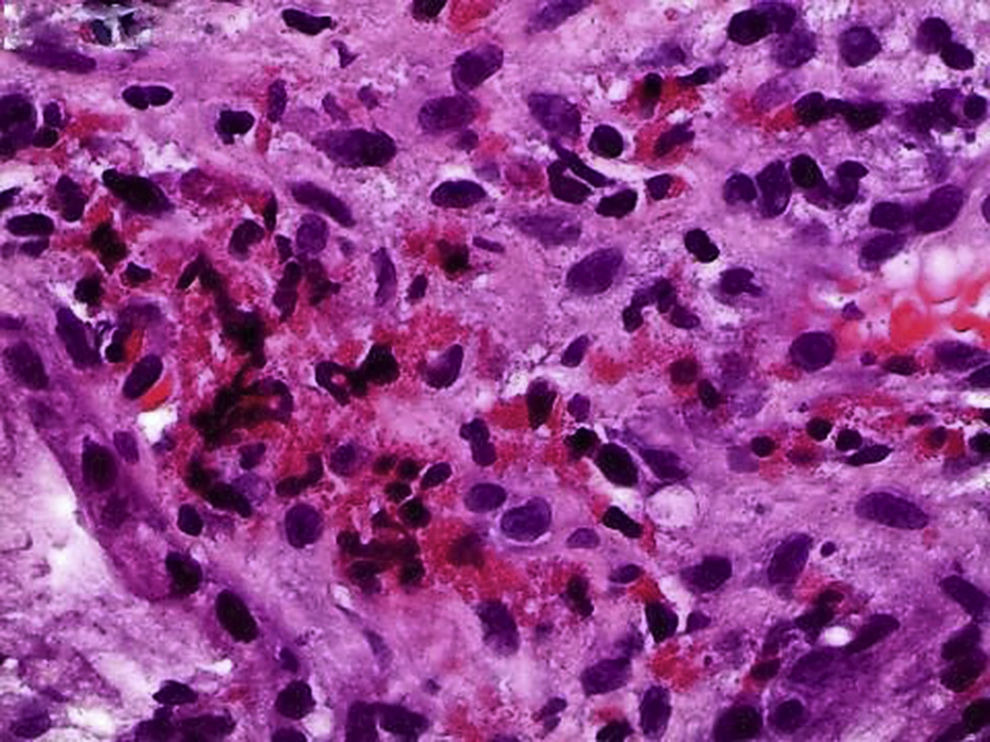
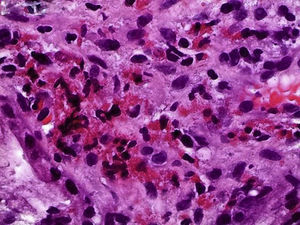
Notable findings on admission included her fair general condition, uncontrollable vomiting, tetany and abdominal pain. Initial laboratory testing showed hyperglycaemia with no ketonaemia, modest leukocytosis with a normal formula, CRP 0.6mg/dl and ESR 26mm, indicators of dehydration (urea 55mg/dl and creatinine 1.5mg/dl), and initially respiratory and, subsequently, metabolic alkalosis. Her fluid and electrolyte balance was corrected, and she was administered ondansetron, omeprazole and diazepam. After a few hours, she experienced clinical and laboratory deterioration with severe metabolic alkalosis (maximum pH 7.73, CO3H 38.4mmol/l and BE 17.6), hypokalaemia and hypochloraemia. This led to her transfer to the semi-intensive care unit. She required fluid and electrolyte replenishment, treatment with acetazolamide, an insulin pump and peripheral parenteral nutrition for 3 days. When she improved clinically and showed gradual tolerance to polymeric enteral formula, fibrogastroscopy was performed and revealed severe grade C peptic oesophagitis lesions from the middle third to the cardia, with confluent erosions without causing stenosis, a normal stomach and stenosis in the pyloric region. Biopsies reported eosinophilia with no malignancy. An abdominal CT scan was performed which ruled out a mass and reported thickening of the walls of the pylorus and duodenal bulb. After 7 days, for purposes of obtaining more information on the stenosed area, an endoscopic ultrasound was performed at another centre, and showed images of rings in the medial and distal oesophagus with a normal stomach, and stenosis at the duodenal bulb with a normal second part of the duodenum (Fig. 1). Biopsies reported fibrosis and oedema with more than 60 eosinophils/HPF in the medial and distal oesophagus, a normal stomach (with no Helicobacter pylori or parasites), and, at the duodenal bulb, oedema and fibrosis in the lamina propria and more than 100 eosinophils/HPF. These findings were consistent with eosinophilic gastroenteritis (Fig. 2). Subsequently, the study was completed and causes of secondary eosinophilia were ruled out.
With this diagnosis and obstructive clinical involvement, the patient was started on treatment with oral budesonide (9mg/day) and maintenance with azathioprine (following determination of thiopurine methyltransferase activity), in addition to treatment with omeprazole. To date, her clinical course has been satisfactory.
Primary eosinophilic gastrointestinal disorders (EGIDs) encompass a group of diseases characterised by symptoms that cause abnormal infiltration of eosinophils into any part of the gastrointestinal tract, in the absence of other secondary causes, and that may involve different layers. Depending on their location and infiltration, there may be a variety of symptoms. Their treatment and clinical course are variable depending on these parameters.1 The latest studies in the United States reported the following prevalences2: 6.3/100,000 for eosinophilic gastroenteritis, 8.4/100,000 for eosinophilic gastroenteritis, 3.3/100,000 for colitis and 57/100,000 for eosinophilic oesophagitis (EoO). They are reported at any age, but the vast majority are elderly and there is a predominance of women. Overall, they are rare at young ages, such as that of our patient.
Pathogenesis reportedly involves a mixed mechanism3 wherein eotaxin and allergens activate eosinophils, thereby stimulating helper T cells and causing IgE and IL5 to form. Subsequently, mast cells undergo degranulation and release histamine and serotonin, and the gastrointestinal smooth muscle contracts. Signs and symptoms1,4 vary depending on the involved gastrointestinal tract and layers. Mucosal involvement results in abdominal pain, diarrhoea, weight loss and malabsorption. Muscle involvement results in signs and symptoms of obstruction. Serous involvement may cause ascites. In our patient, involvement of the oesophagus and duodenal bulb, as well as muscle infiltration, caused signs and symptoms of obstruction. Our patient had no eosinophilia or history of allergy. Eosinophilia occurs in 20–80% of cases, and is more common in the serous form. Allergic comorbidity is very common and occurs in up to 45% of patients. Diagnosis is confirmed by biopsy which reports the eosinophil count per HPF and the number of layers involved.5
Treatment depends on the area involved and its infiltration. In our patient, dietary treatment was rejected,6 and it was decided to use oral budesonide4 and maintenance with azathioprine due to the possibility of recurrences, and omeprazole to treat her peptic oesophagitis.
We believe the case is interesting, considering the age of the patient; the serious form of onset in a teenager with a history of gastrointestinal symptoms classified as a possible eating disorder, which caused us to initially doubt its organic nature; and the severe impairment, which required us to consider long-term immunosuppressant treatment.
Please cite this article as: Masiques Mas L, Coll Sibina MT, Sans Tojo J, Conti R, Cuatrecases M. Gastroenteritis eosinofílica en una paciente adolescente: un diagnóstico poco común. Gastroenterol Hepatol. 2017;40:401–403.