Diverticula of the jejunum and ileum, together with diverticula of the stomach, occupy last place in terms of frequency of gastrointestinal diverticula. They account for approximately 0.9–1% of all diverticular disease. They mainly occur in older adults and are not normally suspected in differential diagnoses of abdominal pain. This leads to a delay in their suitable management.
Clinically, they are usually asymptomatic or have non-specific symptoms. Acute complications, such as perforation, haemorrhage and intestinal obstruction sometimes arise, and usually require emergency surgical treatment.
We present the case of an 86-year-old male patient with a personal history of transurethral resection due to bladder carcinoma in 2013 and cholecystectomy. He sought care as the colicky abdominal pain in his right flank that he had been experiencing for the last month had worsened in the last 24h and was accompanied by vomiting. His physical examination revealed a poor general condition, with tachycardia and a tendency towards hypotension. His abdomen was distended and his right flank was painful on palpation, with voluntary defence and signs of peritoneal irritation.
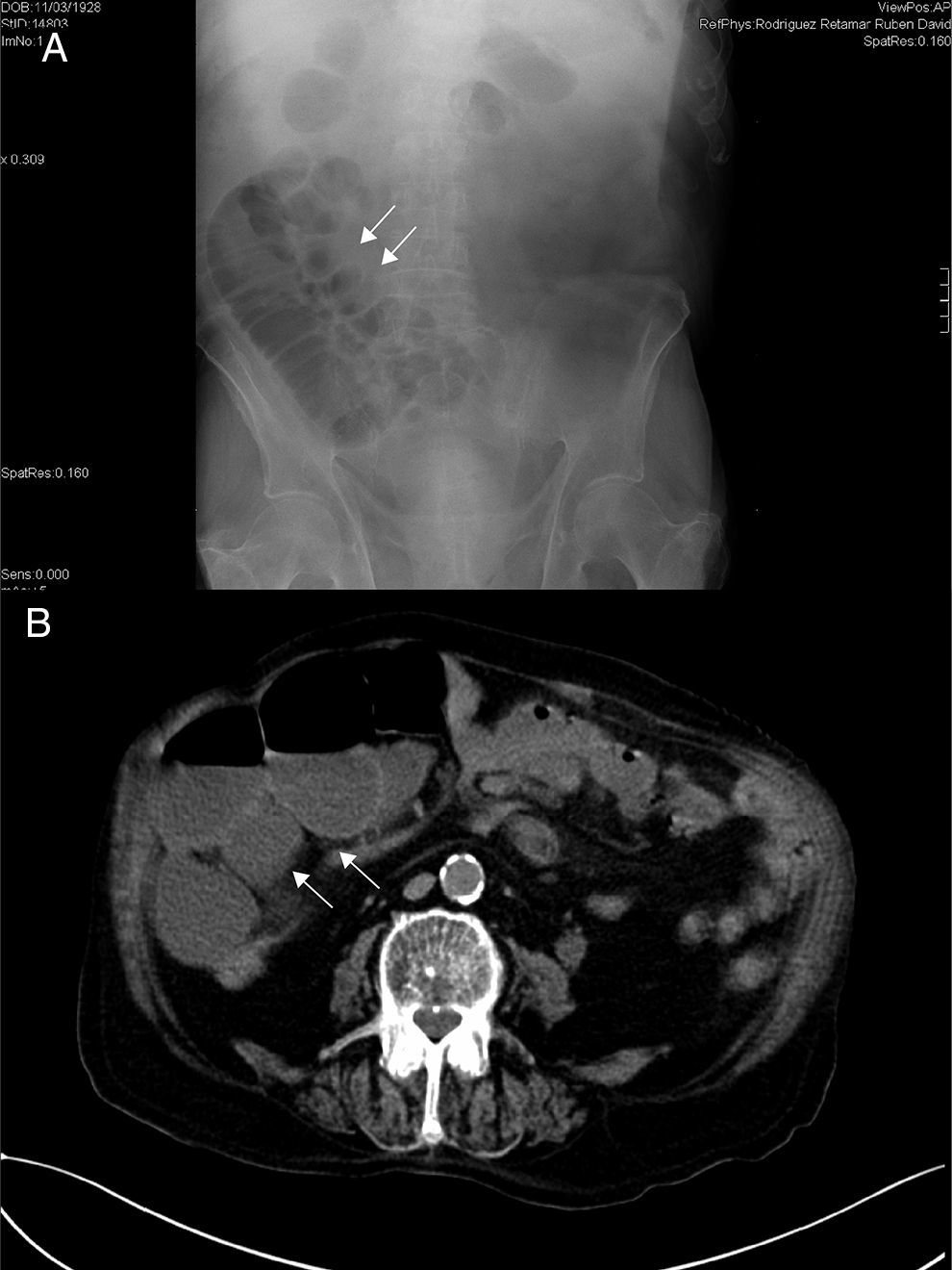
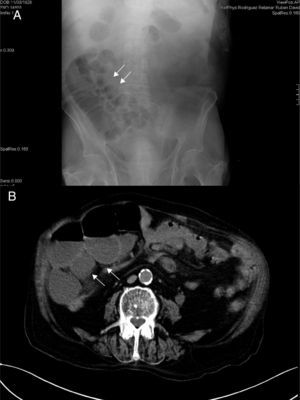
An abdominal X-ray showed small bowel loops with some air-fluid levels (Fig. 1A). His laboratory tests showed leukocytosis with left shift. Given the clinical context of the patient (advanced age and deterioration of general condition), an emergency abdominal computed tomography scan was ordered to complete the diagnosis, in view of the possible need for a surgical procedure. The scan reported distended small bowel loops, but could not identify the cause of obstruction (Fig. 1B).
With a diagnosis of intestinal obstruction, he underwent surgery, which found small bowel volvulus secondary to an adhesion. This involved a segment of jejunum with multiple large diverticula and signs of ischaemia (Fig. 2). Resection of the segment involved and anastomosis were performed. He had no diverticula in other locations.
After surgery, he developed acute pulmonary oedema and died on day 3 of the postoperative period.
Diverticular disease of the jejunum and ileum, excluding Meckel's diverticulum, is a rare, usually asymptomatic disease. It may be chronic or acute; this renders it difficult to make a suitable diagnosis. In addition, due to a lack of awareness of the disease, it is rarely considered as part of the differential diagnosis of gastrointestinal diseases. The first reports of jejunal diverticulosis were made by Sommervit in 1794, Voigtel in 1804 and Sir Astley Cooper in 1807.1 Since then, several articles reporting clinical complications of this disease have been published.
Jejunal and ileal diverticula are acquired pseudodiverticula (thin walls, with no muscle layer) that are seen in approximately 0.5–2.3% of X-ray examinations of the small bowel performed for multiple reasons, and in 0.06–4.5% of autopsy series.2 They present in patients in their 50s and 60s, although cases have been reported in patients as young as 20 years of age.3 There is no clear preponderance of one sex or the other, although some studies have demonstrated a higher prevalence in males.2 Most cases feature multiple proximal diverticula (80% jejunal, 15% ileal and 5% mixed).
Like diverticula of the colon, their pathogenesis appears to be multifactorial. Intraluminal driving forces, generated by the intestinal contents and peristaltic muscle contractions of the intestinal wall, distend sites of weakness in the wall where blood vessels penetrate to supply blood to the bowel mucosa and ultimately cause the mucosa and submucosa to herniate in the absence of the muscle layer. Thus, they are seen on the mesenteric side of the bowel only. They may be associated with diverticulosis of other sites in the gastrointestinal tract, such as the oesophagus (2.3%), duodenum (30%) or colon (61%).2–4 Around 50% of patients with jejunal and ileal diverticulosis have diverticula of the colon at the same time.
Most cases are asymptomatic. Symptomatic forms (10–19%) may be acute or chronic. Patients with chronic symptoms represent up to 60% of cases and have non-specific symptoms related to abnormalities in intestinal motility, as well as signs and symptoms of intestinal malabsorption. In 10–20% of cases, acute complications such as diverticulitis, perforation, obstruction, volvulus, intussusception, malabsorption and gastrointestinal haemorrhage may arise.4
Intestinal obstruction secondary to jejunal diverticulosis presents in 2.3–4.6% of cases,5 and in most cases requires surgical treatment. It may be secondary to adhesions deriving from prior inflammatory processes, volvulus, invagination or extrinsic compression by a loop with large diverticula; another common cause is enterolytes.1,3,6
Jejunal diverticulosis is a disorder that is difficult to diagnose since it lacks genuinely reliable diagnostic tests. In most cases, it is an incidental finding on imaging techniques or autopsies. A plain abdominal X-ray reveals a distended jejunal loop with air-fluid levels inside.6 Computed tomography identifies diverticula, as well as associated complications such as air, free fluid in the cavity, inflammatory masses and abscesses in the mesenteric fat.1,7
At present, different technological resources available, such as tomography enteroclysis and endoscopy (capsule and double-balloon) enable a more accurate diagnosis, although their usefulness in emergency situations is more limited.
Treatment should be focused depending on the type of symptoms and complications that the patient has. Acute complications of jejunal and ileal diverticula generally undergo surgery and are diagnosed as acute abdomen. The recommended technique is resection of the segment involved. The extent of resection depends on the length of bowel involved and the patient's perioperative requirements.8 Some series have reported a morbidity of 4% and a mortality of up to 30%.9 This very high figure is attributed to a delay in diagnosis and proper treatment. In cases of non-perforated diverticulitis, antibiotic treatment, together with gastrointestinal rest, is very useful. When there are intra-abdominal abscesses, percutaneous drainage achieves good results.1,10,11
In chronic forms, which manifest as chronic pain or abnormal motility, analgesics and intestinal motility regulators may be useful.10 Some authors support prophylactic resections due to the seriousness of some complications, such as perforation, while other authors affirm that they have demonstrated no greater benefits12 and that, furthermore, most patients are elderly and have multiple associated diseases.
In conclusion, diverticula of the jejunum represent a rare disease with multiple clinical manifestations that, due to its low incidence and a lack of awareness thereof, is diagnosed incorrectly. This delays its suitable management and increases its mortality due to complications identified late.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Romera-Barba E, Gálvez Pastor S, Navarro García MI, Torregrosa Pérez NM, Sánchez Pérez A, Vazquez-Rojas JL. Diverticulosis yeyunal: una causa rara de obstrucción intestinal. Gastroenterol Hepatol. 2017;40:399–401.