CASE REPORT
A 78-year-old man with a ten-year history of HCL, a silent clinic, without treatment required. He was in treatment with digoxin, acenicumarol, diltiazem and flutamide for a prostatic cancer.
The day of admission the patient was found to be lethargic and weak. Few days after the patient developed asthenia. In his physical exam he was found to be orientated, bradipsiquie, scleral ictericus, blood presure of 124/96 mmHg, and a temperature of 38.2 ºC. The abdomen was painful, overcoat in right side, with splenomegaly.
Admisión laboratory tests showed creatinine 1.7 mg/dl, blood urea nitrogen 49.2 mg/dl, sodium 129 mmol/l, potassium 4.4 mmol/l, calcium 7.4 mg/dl, total bilirubin 3.6 mg/dl, direct bilirubin 1.7 mg/dl, aspartate aminotransferase 1151 U/l, alanine aminotransferase 799 U/l, PCR 7.5 mg/dl, white blood cells 8530/µl, hemoglobin 8.3 g/dl, platelets 67,000/µl, partial thromboplastin time 96.6 sec, INR 4.69, IQ 18%. Previously he had normal liver enzymes. Hemocultures at the day of admission, as well as serologic tests for hepatitis A, B, C, cytomegalovirus, Epstein-Barr virus, VIH, herpes simplex, measles, Coxiella burnetti, rubella, toxoplasma and varicela were negative. Ultrasonographic and TC scan showed a normal liver size with an increased echogenicity of parenchyma and a splenomegaly of 22-24 cm.
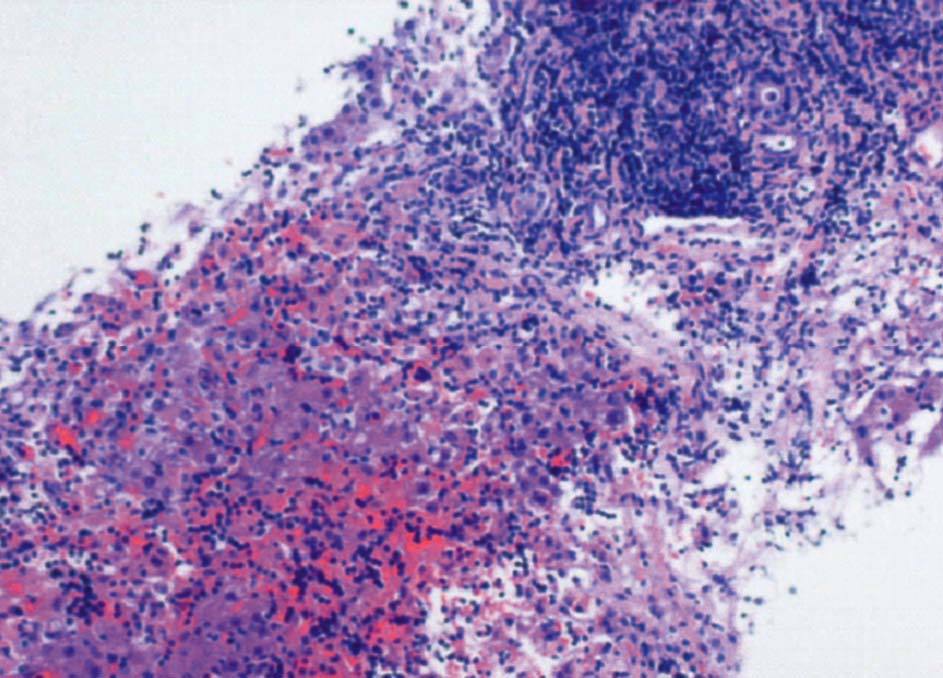
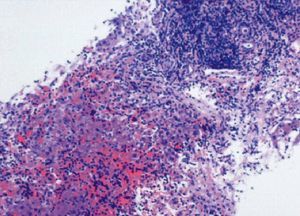
Since the first day of admission we observed an acute clinic and analytic deterioration (table I), despite red blood cells and plasma transfussion, vitamin K, antibiotics, and vasoactive drugs. Coma and death followed three days after the initial of symptoms and liver failure. A postmortem hepatic biopsy was obtained (fig. 1).
Fig. 1. Liver infliltration by hairy cell leukemia.
DISCUSSION
Fulminant hepatic failure carries a high mortality. It can result from a wide variety of causes, among which viral or toxin-induced hepatitis are the most common. Other less frequent etiologies are vascular causes, metabolic disorders, malignant infiltration of the liver, sepsis, heat stroke and autoimmune hepatitis1. We rejected a viral hepatitis by serologic tests. He was in treatment with flutamide since two years and diltiazem2,3. There are several cases of hepatotoxity due to these drugs. There are a few reports of acute hepatic injury including granulomatous hepatitis with the use of diltiazem. In the review made by Wysowski et al4 the post-mortem examination of the liver showed massive hepatocellular necrosis, collapse of lobules, ductal proliferation, and cholestasis without inflammatory cells. The findings in the liver biopsy in our patient were not compatible with these alterations.
Hepatic invasion by malignant lymphoma frequently affect the liver, but it is a rare cause of liver failure and usually has a fatal prognosis5-8. We only have found after a review one case of acute liver failure in a patient with hepatic invasion by HCL9. As in this case, acute advanced liver failure and death shortly after the onset of symptom. Liver biopsy of both demonstrated extensive portal and intralobular hairy cell infiltration with loss of normal architecture. Shehab et al10 have made a review of 23 cases of acute liver failure due to infiltration of the liver by hemotologic malignancies. All presented a clinic and biochemistry presentation compatible, without previous hepatic pathology and confirmation of microscopic infiltration of the hepatic sinusoids. The median survival is about 11 days. In another review of 25 similar patients, the average time of survival was about 7.8 days10.
Furthermore ischemia and injury due to cytokines released have been proposed as the mechanism responsible. TNF-*, interleukin (IL-1, IL-2, IL-6) and several eicosanoids active neutrophiles, endothelial cells of the sinusoids hepatic and kupffer cells induced necrosis of the hepatocytes11-13.
In conclusion, the association between HCL and acute liver failure is unusual, otherwise there are several mechanims, as ischemia and release of cytokines, that can explain something more than a coincidence.