Casos Clínicos en Gastroenterología y Hepatología
Más datosWe present the case of a 40-year-old woman diagnosed with celiac disease 5 years ago, without treatment or follow-up, and with a cyclic colicky central abdominal pain, that had evolved over the course of 4 months. She presented to our emergency department with a 4-day history of worsening of her abdominal pain. She complained about associated generalized abdominal distension, vomiting and constipation. Her menstrual periods were regular with no menorrhagia, dysmenorrhea or dyspareunia reported. On physical examination her bowel sounds were hyperactive, and her abdomen presented diffuse tenderness with a voluntary component in the right lower quadrant.
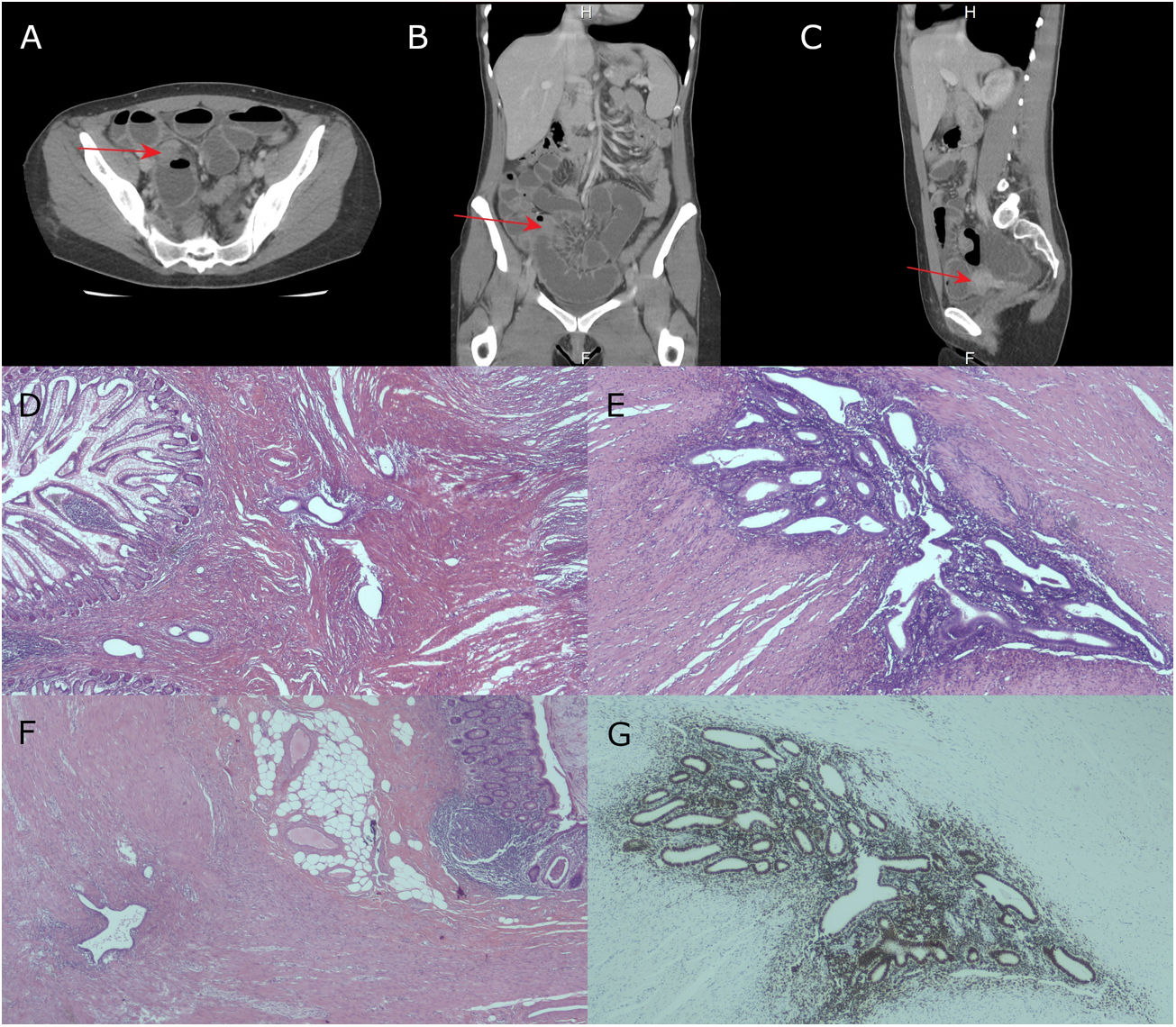
An abdominopelvic CT scan revealed a concentric thickening of 3cm in the distal ileum, with significant luminal narrowing and proximal ileal dilatation (Fig. 1A–C).
(A) Axial image of an abdominopelvic CT scan showing concentric mural thickening of the distal ileum, consistent with complete small bowel obstruction. (B) CT coronal image. (C) CT sagittal image. (D) HE staining (4×): focus of endometriosis in the distal ileum. (E) HE (10×) Detail of a nest rich in glands and endometrial stroma in the ileal muscular layer. (F) HE (4×) Focus of endometriosis within the appendicular wall. (G) HE (10×). Positivity for estrogen receptors in the endometrial glands of the distal ileum.
With the preoperative diagnosis of a small bowel obstruction probably secondary to an intestinal lymphoma on previous celiac disease, an urgent laparotomy was performed. Intraoperatively, a tight ileal stricture at the level of the terminal ileum (20cm to the ileocecal valve) and dilated proximal ileum was observed. During the exploration a lump was seen at the tip of the appendix; however, the base appeared normal. An ileal segmental resection with a side-to-side anastomosis, and appendectomy was performed. No more implants or lymph nodes were seen neither in the small bowel nor in the pelvis.
Pathologically, the ileum showed multiple endometrial glands surrounded by stroma within the muscular layer (Fig. 1D and E). The appendix also showed multiple endometriotic foci (Fig. 1F). The immunohistochemistry studies showed the glands to be positive for estrogen receptors, confirming the endometrial origin (Fig. 1G). However, the caecum and ascending colon were free from endometriosis. After ensuring that no postoperative complications occurred, the patient was discharged and referred to a gynecologist.
Reports of small bowel endometriosis are highly uncommon (0.03–2.5% of endometriosis cases) and complete intestinal obstruction due to this pathology is exceptional, ranging from 0.15% to 0.7% of all cases with intestinal involvement.1 The prevalence of appendiceal endometriosis is <1% of endometriotic cases and accounts for less than 1% of all appendicular pathologies.1 Only three cases of ileal obstruction due to endometriosis, and isolated synchronous appendicular involvement, have been reported so far.1
Establishing a preoperative diagnosis of intestinal endometriosis has proven to be a challenge, being usually found as an incidental finding on surgery,1,2 as it occurred in our case.
Firstly, misdiagnoses are common because of the decreased index of suspicion, due to the rarity of this entity.1,2 Secondly, gastrointestinal endometriosis is clinically similar to the multiple other causes of small bowel obstruction such as inflammatory or infectious bowel disease, irritable bowel syndrome, ischaemic enteritis and tumours.1,2 The most common presentation is cramp lower abdominal pain (76.5%), with a cyclic pattern increasing in intensity (41.2%), that may hint towards endometriosis in a menstruating patient, as a cause of small bowel obstruction.1,2 Abdominal mass is present in the 34% of cases.1,3 Thirdly, no radiological gold standard currently exists as imaging findings are quite non-specific and usually indistinguishable from other gastrointestinal problems, leading to the diagnostic dilemma.3 Biscaldi et al.4 demonstrated the efficacy of multislice CT combined with water enteroclysis (MSCTe) in distinguishing endometriotic lesions from chronic inflammatory and neoplastic lesions, but it remains unsuitable for patients with obstructive symptoms.4 Magnetic Resonance Imaging is the diagnostic test with the highest sensitivity and specificity rates, although it fails to diagnose extrapelvic endometriosis.3 On the other hand, since the disease does not involve the mucosa, barium enema and endoscopy are not helpful,1,3 as it happened with our patient. The diagnosis can be confirmed only on histology of the resected specimen.1,2
Asymptomatic and mildly symptomatic cases may be treated using hormonal treatment.1 However, resection of the involved bowel remains the choice of treatment for complicated or unresolved cases.2,5 Although the gold standard in endometriosis is laparoscopy, in case of bowel obstruction, urgent laparotomy and resection of the affected segment, a laparotomy is indicated.1,2 Suspicion of malignancy may also warrant a radical resection.2,5
In conclusion, endometriosis as a cause of small bowel obstruction, with appendicular involvement, is a unique entity. Our case highlights the preoperative diagnosis dilemma, and we give the clues for a prompt diagnosis and for the management of this exceptional situation.
The paper is NOT based on a previous communication to a society or meeting.