Information received by IBD patients about their disease is of particular importance. The objective of the study was to determine the information resources these patients used, together with their perceived information gaps and expected preferences.
Patients and methodsA prospective, observational, cross-sectional study conducted on IBD patients attending 13 Spanish hospitals during 2008. Patients completed a semi-structured 52-question survey.
ResultsSurvey was adequately completed by 379 of 385 patients (98%), of whom 57% had Crohn's disease and 43% ulcerative colitis. Mean patient age was 37.9 years (range, 16–76 years). Gastroenterologists were the most commonly used resource (98%), followed by the Internet (60%), and general practitioners (50%). More than 90% reported good to excellent satisfaction with gastroenterologists, nurses, and patients’ associations. Only 56% considered their information needs to be covered. The Internet was mostly used by young patients and those with a high education level. In the future, 85% of the patients would like to receive information from the gastroenterologists, and 92% by face-to-face interviews. Patients mainly want additional information on treatment (medical and surgical), clinical manifestations, cancer, and mortality risks. They also think that they are poorly informed about their social and work rights, risks of cancer and death, and research trials.
ConclusionsPatients with IBD use and prefer gastroenterologists as the main source of information, but only half of them consider their information needs to be covered.
La información recibida por los pacientes con EII sobre su enfermedad es de particular importancia. El objetivo de este estudio fue determinar los recursos informativos que utilizan estos pacientes, así como las lagunas de información que perciben y sus preferencias.
Pacientes y métodosEstudio prospectivo, observacional y transversal realizado en pacientes con EII atendidos en 13 hospitales españoles durante el año 2008. Los pacientes cumplimentaron un cuestionario semiestructurado de 52 preguntas.
ResultadosEl cuestionario fue cumplimentado adecuadamente por 379 de los 385 pacientes participantes (98%). De ellos, el 57% presentaban enfermedad de Crohn y el 43% colitis ulcerosa. La edad media de los pacientes fue de 37,9 años (intervalo: 16-76 años). Los gastroenterólogos fueron el recurso más utilizado (98%), seguido de Internet (60%) y de los médicos de familia (50%). Más del 90% de los pacientes señaló un grado de satisfacción con el gastroenterólogo, el servicio de enfermería y las asociaciones de pacientes de buena a excelente. Solo el 56% considera que sus necesidades informativas están cubiertas. Los pacientes jóvenes y aquellos con un nivel educativo alto son los que más utilizan Internet. Al 85% de los pacientes le gustaría recibir información de los gastroenterólogos en el futuro, y el 92% preferiría tener entrevistas presenciales. Los pacientes quieren principalmente información adicional sobre tratamientos (médicos y quirúrgicos), manifestaciones clínicas, cáncer y riesgos de mortalidad. También piensan que están mal informados acerca de sus derechos sociales y laborales, los riesgos de cáncer y la mortalidad, así como sobre los estudios de investigación.
ConclusionesLos pacientes con EII utilizan y prefieren tener a los gastroenterólogos como fuente principal de información, pero solo la mitad de ellos consideran que sus necesidades informativas están cubiertas.
The onset of chronic inflammatory bowel disease (IBD) tends to occur in young adults. It has a typical course with exacerbations and remissions, with the resulting long-term morbidity (including hospitalisations, surgery, etc.).1 As with other chronic and disabling diseases, an adequate doctor–patient relationship is required to improve the communication and well-being of patients and their relatives. Moreover, adequate information is an important factor to improve self-management of the disease.
Healthcare professionals who care for IBD patients should be aware of their information needs, as well as their concerns and degree of satisfaction with care received.2 Improvement in health-related quality of life (HRQL) should be one of the essential objectives in the treatment of IBD.3 Specialised clinics and multidisciplinary IBD units are proliferating in Spain and other countries to provide appropriate care to these patients. They allow for a more personalised and efficient relationship, with coordinated involvement of various departments and implementation of cross-disciplinary, patient-focused management models.4 Provision of adequate information is considered a key element because: (1) there are very different ways to provide it (brochures, books, healthcare staff, the Internet, conferences, etc.)5; (2) adequate information seems to have a positive impact on quality of life3; and (3) acquisition of knowledge about the disease and the emotional adjustment to living with it seem to be closely related.6,7 Recent studies have shown the importance of providing good information on aspects related to IBD2 both after diagnosis and during disease progression.8
However, there are few data on the specific needs of the Spanish population (information systems used and preferred, degree of satisfaction with them, priority issues for which information is sought, shortcomings in means used, etc.).6 Moreover, the increasing use in recent years of new information technology tools such as the Internet (websites, forums, social networks, etc.) may have changed the information needs and expectations of our patients.9–11
This study was therefore undertaken to determine, in a large sample of Spanish patients with IBD, the resources and methods used to get information; to assess the degree of satisfaction with the information received; and to provide an objective view of the shortcomings and patients’ preferences in order to optimise acquisition of information.
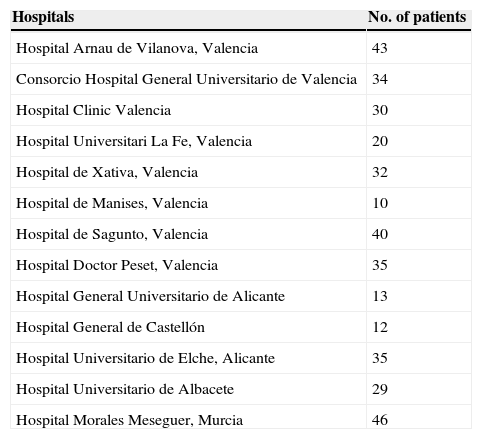
Patients and methodsPatients and centresA multicentre, prospective, observational, cross-sectional cohort study conducted on IBD patients over 18 years of age attending outpatient gastroenterology clinics specialised on IBD at 13 Spanish hospitals in the Autonomous Regions of Valencia and Murcia and in the province of Albacete (Table 1). Five of these are attending mainly urban population, and the rest take care of mixed urban–rural population. Six of them take care of between 250 and 499 patients, four between 500 and 749 and three more than 750 IBD patients. All clinics have experienced surgical teams in the management of IBD, including ileo-anal pouches. From all hospitals, only two have specialised IBD nurses, two have specific telephone service for IBD patients, and one provides Internet consultation.
Hospitals and number of patients included.
| Hospitals | No. of patients |
|---|---|
| Hospital Arnau de Vilanova, Valencia | 43 |
| Consorcio Hospital General Universitario de Valencia | 34 |
| Hospital Clinic Valencia | 30 |
| Hospital Universitari La Fe, Valencia | 20 |
| Hospital de Xativa, Valencia | 32 |
| Hospital de Manises, Valencia | 10 |
| Hospital de Sagunto, Valencia | 40 |
| Hospital Doctor Peset, Valencia | 35 |
| Hospital General Universitario de Alicante | 13 |
| Hospital General de Castellón | 12 |
| Hospital Universitario de Elche, Alicante | 35 |
| Hospital Universitario de Albacete | 29 |
| Hospital Morales Meseguer, Murcia | 46 |
Over the course of two months of 2008, consecutive patients were asked to self-complete a semi-structured, anonymous 52-question (q) survey. All patients requested filled the survey form. The questionnaire was prepared by consensus among the principal investigators of the participating centres. A draft semi-structured questionnaire was prepared where answers regarding information preferences were already stated, with one last field available for suggestions. Patients only had to rank the answers by preference. To assess patient comprehension of the survey, 10 pilot surveys were conducted before the final questionnaire was obtained. The survey was completed by the patients, who had a physician or nurse available to answer any questions they could have. Informed consent was obtained from all patients.
The questionnaire covered the following aspects:
- a.
Demographic and disease-related data:This section included questions about gender, age, level of education (3q), disease type and characteristics (age at diagnosis, years since diagnosis, surgical procedures due to the disease, whether or not they carry a permanent ileostomy or colostomy, need for hospitalisation), and medical treatments received: aminosalicylates, corticosteroids, immunosuppressants, biologicals, leucocyte apheresis, and enteral diet, followed by one open option (others) (8q).
- b.
Questions on how patients obtained information about their disease: types and means used (general practitioner, gastroenterologist, surgeon, nurses, Internet sites, books, magazines, brochures, meetings at patients’ associations, Internet forums, and other). Patients were asked to assess their satisfaction with information received by each of these means using an analogue scale with five possible answers (1. excellent/2. very good/3. good/4. fair/5. poor), and to provide their frequency of use per month and year (36q).Patients were finally asked to assess their satisfaction using the following question: Do you think that the information means you currently have fully covered your needs? (1q).
- c.
Questions relating to future information preferences.Four questions assessing information preferences were included: (1) Preferred resources for receiving information, which included 13 options (the internet, magazines, books, manuals, explanatory brochures, general practitioner, gastroenterologist, surgeon, patients’ associations, the press, specialised conferences, nursing services, and other). Patients had to write “1” next to the resource they considered most appropriate, and consecutively rank the other options by decreasing order of preference. (2) Preferred systems for receiving information: 10 options were provided (face-to-face or telephone conversation with the gastroenterologist, written dialogue with specialists over the Internet, pocket manuals, books, magazines, explanatory brochures, face-to-face or Internet-based discussion forums and other). Patients had to write “1” next to the system they considered most appropriate, and consecutively rank the other options by decreasing order of preference. (3) Priority issues in receiving information, where patients were asked to write “1” next to the top priority aspect on which they needed information, and to subsequently rank all other options by decreasing order of interest. Options included: clinical aspects of the disease, medical treatment, surgical treatment, risk of cancer, risk of transmitting the disease to their offspring, risk of death, relationship between disease and pregnancy or fertility, risks of medical treatments, importance of diet for their disease, importance of sport for their disease, preventive actions to be taken when travelling abroad, vaccination risks, impact on work relationships, social rights, work rights, risks of commonly used diagnostic methods, treatment breakthroughs, finding out about research trials, and others. (4) Aspects of the disease on which they thought they were more poorly informed, or for which there were fewer information resources. Patients had to rank the 19 options given, assigning number “1” to the aspect on which they felt they had the poorest information.
Data were analysed using SPSS Version 17.0 for Windows (SPSS Inc. – Chicago, IL. USA). Independent variables used included gender, age (<50, >50 years), diagnosis (Crohn's disease, ulcerative colitis), level of education (low or high), and time from diagnosis to survey completion (< or > two years). In the analysis of the degree of satisfaction with each of the resources commonly used by patients, mean ranking of each resource and the difference in means were analysed using a Wilcoxon test for non-parametric variables. The variable was also reconfigured as qualitative, considering those who answered 1, 2 or 3 as “satisfied”, and those who answered 4 or 5 as “dissatisfied”. For the analysis of preferences, the set of the different variables was taken as a ranking list, and the methodology proposed by Dunn–Rankin and King12 was applied. The sum of the positions assigned by the different respondents in their order of preference (sum of ranks) was calculated for each variable, and the formula (13) V=100−[(ΣR−N/N×K)×100] was applied, where ΣR is the sum of ranks, N is the number of subjects, and K is the number of options in the ranking list. This calculation allows for transforming the sum of ranks into a variable that is simpler to interpret, the V variable (preference value), which takes values from 0 to 100 depending on intensity of the preference. Thus, zero would be the value taken if all respondents ranked it last, and 100 would be the value in the event that the variable was always ranked first by order of preference.
Categorical values were expressed as percentages. Differences between these variables were calculated using a Chi-square test. Variables were correlated with a Pearson's test. Values of p≤0.05 were considered statistically significant. Forward stepwise multivariate logistic regression was used to assess the predictive power in the relationship between variables and use of resources, assessing the likelihood ratio.
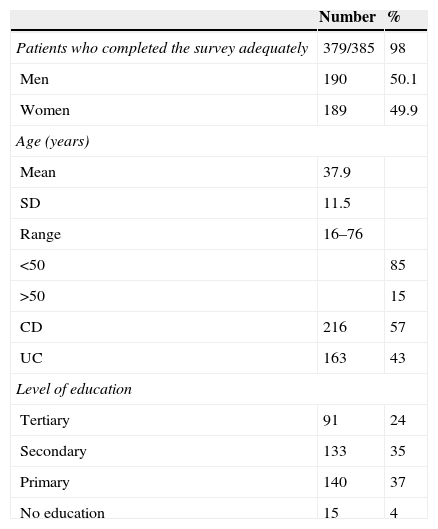
ResultsPatient characteristicsA total of 385 patients completed the questionnaires, of which 379 (98%) were assessed. All surveys with any missing independent variable were considered as non-assessable. 216 patients (57%) had Crohn's disease (CD), and 163 (43%) ulcerative colitis (UC). The assessed group consisted of 190 males (50.1%) and 189 females (49.9%) with a mean age of 38 years (range, 16–76). Most patients reported primary (37%) and secondary education (35%) (Table 2). Mean age at disease diagnosis was 30 years (range, 7–64), and mean time since disease onset at survey completion was 8 years (range, 1–37 years). Patients with a disease duration less than two years (23.1%) were considered to be recently diagnosed. A total of 126 patients (33%) had undergone surgery for their disease, with a mean of 2.3 procedures/life (range, 1–10), and 17 patients (4.5%) carried an ileostomy. CD patients had required surgery more frequently than patients with UC (45% vs. 17%, p<0.001). Hospitalisations had been required by 68.5% of patients, with a mean number of four hospital admissions (range 1–30). Hospitalisation had been required by 77% of CD patients, as compared to 56% of patients with UC (p<0.001).
Of all patients, 84.7% had taken corticosteroids, 71.8% aminosalicylates, 62.5% immunosuppressants, and 26.6% biologicals, and 4.2% had undergone leucocyte apheresis.
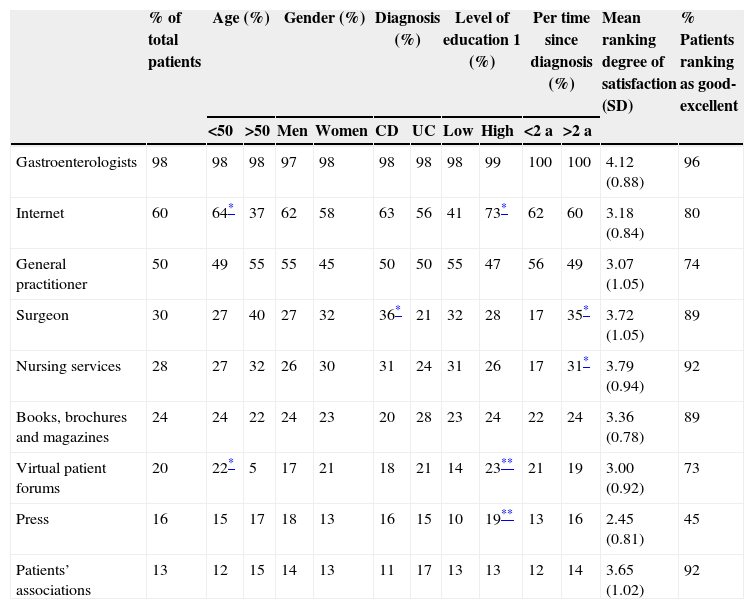
Current sources of information and degree of satisfactionTable 3 shows the main information sources used by gender, diagnosis, age, educational level, and disease duration. Patient assessment of the different resources is also given.
Information sources currently used by patients.
| % of total patients | Age (%) | Gender (%) | Diagnosis (%) | Level of education 1 (%) | Per time since diagnosis (%) | Mean ranking degree of satisfaction (SD) | % Patients ranking as good-excellent | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <50 | >50 | Men | Women | CD | UC | Low | High | <2 a | >2 a | ||||
| Gastroenterologists | 98 | 98 | 98 | 97 | 98 | 98 | 98 | 98 | 99 | 100 | 100 | 4.12 (0.88) | 96 |
| Internet | 60 | 64* | 37 | 62 | 58 | 63 | 56 | 41 | 73* | 62 | 60 | 3.18 (0.84) | 80 |
| General practitioner | 50 | 49 | 55 | 55 | 45 | 50 | 50 | 55 | 47 | 56 | 49 | 3.07 (1.05) | 74 |
| Surgeon | 30 | 27 | 40 | 27 | 32 | 36* | 21 | 32 | 28 | 17 | 35* | 3.72 (1.05) | 89 |
| Nursing services | 28 | 27 | 32 | 26 | 30 | 31 | 24 | 31 | 26 | 17 | 31* | 3.79 (0.94) | 92 |
| Books, brochures and magazines | 24 | 24 | 22 | 24 | 23 | 20 | 28 | 23 | 24 | 22 | 24 | 3.36 (0.78) | 89 |
| Virtual patient forums | 20 | 22* | 5 | 17 | 21 | 18 | 21 | 14 | 23** | 21 | 19 | 3.00 (0.92) | 73 |
| Press | 16 | 15 | 17 | 18 | 13 | 16 | 15 | 10 | 19** | 13 | 16 | 2.45 (0.81) | 45 |
| Patients’ associations | 13 | 12 | 15 | 14 | 13 | 11 | 17 | 13 | 13 | 12 | 14 | 3.65 (1.02) | 92 |
The “low” educational level group includes patients with primary or no education. The “high” group includes those with secondary or tertiary education. The information ranking scale values are: 1 – poor, 2 – fair, 3 – good, 4 – very good, 5 – excellent.
98% of study patients used gastroenterologists as information source, while 50% consulted their general practitioners and 30% surgeons; the proportions of patients satisfied with these sources were 96%, 74%, and 89% respectively. Up to 28% of surveyed patients used nursing services, with a high degree of satisfaction (92%).
About 92.5% used more than one information source. The most frequent combination used was: gastroenterologist and the Internet (58.7%), followed by gastroenterologist and the family physician (49.2%) and family physician and the Internet (28.5%).
The Internet was the tool most commonly used as an information source (60% of patients). Virtual Internet patient forums were also used by 20% of patients, while 24% used books, brochures and/or magazines, 16% received information from the press, and 13% from patients’ associations.
Mean ranking of the degree of satisfaction with gastroenterologists was high, and significantly greater as compared to all other information means (p<0.001). The press ranked lowest among information means.
Patients with a high educational level made more frequent use of Internet websites (p=0.01), Internet discussion forums (p>0.05), and mainstream press (p=0.05). Patients under 50 years used the Internet (websites and discussion forums) more frequently (p<0.001).
Analysis of patients with long-standing disease and prior surgical procedures revealed greater use of surgeons and nursing services (p<0001). CD patients also used surgeons more frequently (p=0.001).
The multivariate logistic regression analysis showed a greater use of surgeons and nursing services by patients undergoing surgery (p<0.001), and greater use of the Internet among young patients (<50 years) (p<0.001), and patients with a high educational level (p<0.001).
The different medical treatments were also independently related to use of resources. Thus, use of aminosalicylates and corticosteroids was related to use of gastroenterologists as information source (p<0.001), and prior use of antibiotics correlated with previous surgery.
Percentage differences are shown in Table 3.
Fifty-six percent of surveyed patients answered yes to the question as to whether the resources used fully covered their information needs. The only variables in the multivariate analysis that were related to this positive response were non-use of the Internet (p<0.006) and male gender (p<0.01).
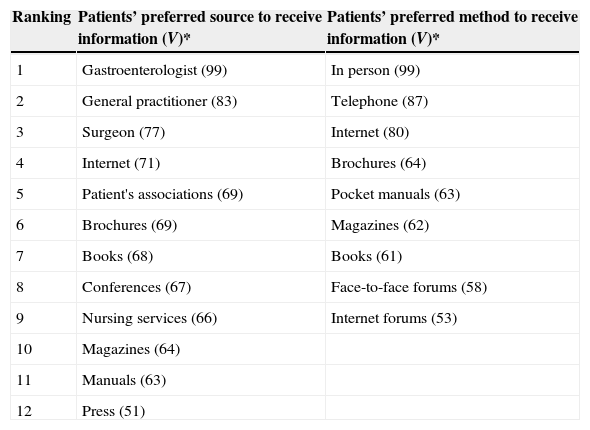
Future information preferences (order of preference)As regards patient preferences for provision of information in the future, gastroenterologists were most commonly cited, followed by general practitioners and surgeons. The press ranked last (Table 4).
Patients’ order of preference to receive information (source and method).
| Ranking | Patients’ preferred source to receive information (V)* | Patients’ preferred method to receive information (V)* |
|---|---|---|
| 1 | Gastroenterologist (99) | In person (99) |
| 2 | General practitioner (83) | Telephone (87) |
| 3 | Surgeon (77) | Internet (80) |
| 4 | Internet (71) | Brochures (64) |
| 5 | Patient's associations (69) | Pocket manuals (63) |
| 6 | Brochures (69) | Magazines (62) |
| 7 | Books (68) | Books (61) |
| 8 | Conferences (67) | Face-to-face forums (58) |
| 9 | Nursing services (66) | Internet forums (53) |
| 10 | Magazines (64) | |
| 11 | Manuals (63) | |
| 12 | Press (51) |
V*=preferential value.
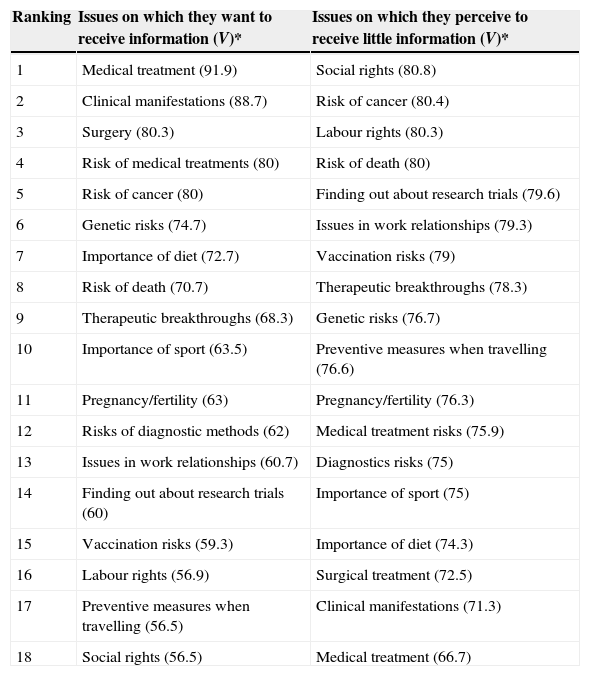
Aspects on which they wanted to receive more information in the future mainly included those related to medical treatment, followed by clinical manifestations and surgical treatment (Table 5).
Ranking by patients of the issues about which they want to receive most information, and those about which they receive the poorest information.
| Ranking | Issues on which they want to receive information (V)* | Issues on which they perceive to receive little information (V)* |
|---|---|---|
| 1 | Medical treatment (91.9) | Social rights (80.8) |
| 2 | Clinical manifestations (88.7) | Risk of cancer (80.4) |
| 3 | Surgery (80.3) | Labour rights (80.3) |
| 4 | Risk of medical treatments (80) | Risk of death (80) |
| 5 | Risk of cancer (80) | Finding out about research trials (79.6) |
| 6 | Genetic risks (74.7) | Issues in work relationships (79.3) |
| 7 | Importance of diet (72.7) | Vaccination risks (79) |
| 8 | Risk of death (70.7) | Therapeutic breakthroughs (78.3) |
| 9 | Therapeutic breakthroughs (68.3) | Genetic risks (76.7) |
| 10 | Importance of sport (63.5) | Preventive measures when travelling (76.6) |
| 11 | Pregnancy/fertility (63) | Pregnancy/fertility (76.3) |
| 12 | Risks of diagnostic methods (62) | Medical treatment risks (75.9) |
| 13 | Issues in work relationships (60.7) | Diagnostics risks (75) |
| 14 | Finding out about research trials (60) | Importance of sport (75) |
| 15 | Vaccination risks (59.3) | Importance of diet (74.3) |
| 16 | Labour rights (56.9) | Surgical treatment (72.5) |
| 17 | Preventive measures when travelling (56.5) | Clinical manifestations (71.3) |
| 18 | Social rights (56.5) | Medical treatment (66.7) |
V*=preferential value.
No statistically significant differences were found when analysing the data with respect to the characteristics of the hospital or the presence of specialised IBD nurse in the clinic.
Preferred method to receive information from a specialised clinicThe order of preference of methods for provision of information was as follows: face-to-face conversation with the gastroenterologist, telephone conversation with the gastroenterologist, and written dialogue with the gastroenterologist over the Internet.
Most poorly informed aspectsThe aspects on which patients think they have the poorest information, or have fewer resources to access information included: social rights (disability, financial aid management, tax benefits, etc.), risk of cancer, work rights, and risk of death.
DiscussionThis paper emphasizes the significance of gastroenterologists in the management of information for IBD patients, as well as the predominant role currently played by the Internet as a resource.
Use of information is analysed in a large patient sample, the largest on which this subject has been studied to date in Spain. The multicentre and collaborative nature of the study, which allowed for recruitment of IBD patients from both specialised practices and hospital units from several Spanish autonomous regions, makes it more representative of patients in our country.
Weaknesses of our study may be its exclusive sourcing of patients from specialised gastroenterology clinics, as selection of patients with more severe disease may involve bias.
Another limitation is that the survey was completed in 2008. That may underestimate the use of the Internet and other new technologic tools which use has spread in the recent years (60% at the moment of the survey). However we believe that this large data provide very valuable information about other important aspects poorly studied in the IBD population in Spain before this multicentre survey.
In this setting, recruitment of patients with long-standing disease (eight years on average), who have good access to the specialist, may also involve a greater satisfaction with information received.
It should also be noted that all patients were recruited by gastroenterologists, who, as discussed below, are the source of information preferred by patients. This result may involve bias, because IBD is a chronic disease that requires frequent controls by the gastroenterologist. Therefore it seems logic that they use and preferred the gastroenterologist as an information source.
Current organisation of care for IBD patients is changing in Spain with the implementation of specialised clinics and multidisciplinary specialised units.4 In order to be able to efficiently organise these units, it is of paramount importance to know the preferences for information of the patients, as well as the options available to access the various information sources and dissemination methods, including new technologies.
As discussed, gastroenterologists are the most frequently used and preferred information source, considered highly satisfactory by 96% of patients. These data are in contrast with the results of the Politi2 study, where only 66% of patients selected gastroenterologists as their main source of information, and their degree of satisfaction, while also high, was somewhat lower (77%). According to data collected in the Mayo Clinic from a survey conducted on 169 patients, 59% chose gastroenterologists as their main information source.10
In a Canadian study published in 20118 which only analysed recently diagnosed patients (less than two years before), the two most commonly used information sources were gastroenterologists (36%) and websites specialising in IBD (38%). According to the analysis performed in this study of patient satisfaction during the first two months following diagnosis, 24% were dissatisfied, 31% moderately satisfied, and 45% very satisfied.8
Results similar to those of our study were reported by Limdi et al.13 based on a survey of 160 IBD patients in the United Kingdom. Gastroenterologists were the first information source for 83% of patients surveyed, with a degree of satisfaction of 54.1%, followed by general practitioners (54.3%) and the Internet (40%).
In our study, 56% of patients felt that their information needs were fully covered by the resources they were using. This proportion is rather low, particularly because these patients come from hospitals with monographic IBD clinics or IBD units. The reasons why 44% of our patients felt that their information needs were not fully covered remain unclear. We can speculate that the short time available for the outpatient visit and the lack of specialised IBD nurses in most of our units can play an important role, but further investigation is needed.
Data also published in Spain in 2004 revealed that only 13% of patients with Crohn's disease and 16% of those with ulcerative colitis thought that they did not receive adequate information, while most felt they were adequately informed.6 Our data reinforces the importance of identifying the possible shortcomings in management of this information, in order to provide effective and focused information to ensure quality care.
As noted above, the fact that our study did not enrol recently diagnosed patients, but rather those with long-standing disease (which may be expected to be more stable), who may be less eager to receive data and information about their condition, may explain the higher satisfaction rates found in our sample. It should be noted that in the sub-analysis performed in our study on patients with a disease duration of approximately two years, gastroenterologists were the main information source in both groups, the only significant item being greater use of surgeons by patients with long-standing disease. This could be explained by the greater need for surgery over time, mainly in Crohn's disease.
As regards use of new technologies, 60% of our patients stated that they used the Internet as information source, with a degree of satisfaction of 80%. This is a greater proportion than the 42% also found in Spain and reported in 2002 by Panes et al.5 and the 24% found in the Politi2 study (which included data from 2002 to 2004). Obviously, these differences may be explained by the proliferation of Internet use in Spanish and European homes in recent years. In fact, in the more recent study conducted by Bernstein in 2011, websites ranked second as information sources on IBD.8
Data similar to ours were reported by Cima et al.10, who found that 54% of patients searched information about IBD on the Internet, which also ranked second as source of information, followed by general practitioners. Most these patients (57%) described the information as “trustworthy” or “highly reliable”. Limdi et al.13 showed that 58% of patients used the Internet to search for information on their disease, but reported a lower degree of satisfaction (21%).13
In our study, patients with a high educational level used the Internet as information source more frequently, which is consistent with studies by Politi et al.2, where this difference was also found between northern and southern European countries. Age under 50 years was also significantly associated to use of the Internet. Cima et al.10 also noted that 73% of patients under 40 years of age used the Internet as information source, as compared to only 37.5% of those over 65 years of age. These results may lead to the creation of customised programmes to deliver information in whom aspects such as educational level or age should be considered.
Our study found that only 13% of Spanish patients used patients’ associations as information sources, but they were very satisfied (92%). These data are consistent with the results of Politi2 and the Canadian study, in which these associations ranked sixth among the preferred means for receiving information in the future after websites.8 In our study, patients’ associations ranked fifth, preceding any printed media and following the Internet. This low rate of use of patients’ associations is a surprising finding, given the good perceived quality of the information received, and requires further study.
Another important aspect in this study was the analysis of the issues on which patients felt to be most poorly informed, or to have fewer resources to access information. Occupational aspects and social rights, risk of cancer and death, and information on research and new treatments are the most demanded aspects (data consistent with other previous European studies2). In another Spanish study by Casellas et al.6, the main issues on which patients considered to have no adequate information were: “causes of the disease,” “disease progression” and “disease complications”.6
It is remarkable that although cancer ranked fifth in our study by order of preference for receiving information, it ranked second in the perception of the poorest information provided.
Recently diagnosed patients expressed greater concern about long-term prognosis and issues relating to cancer development and fertility.8 In the Bernstein et al.8 study, patients also stated that they received little information on disease self-management, both as regards therapy and nutritional aspects, an aspect which was not analysed in our study.
With regard to future preferences, patients prefer to be directly informed by gastroenterologists, and face-to-face conversations with physicians are the preferred way. This suggests that gastroenterologists will probably continue to be the main information channel, despite the increasing use of the Internet and the development of new technologies. This preference has also been reported in patients from other countries.8
This study identified four aspects about which patients wanted to receive better information in the future: medical and surgical treatment, clinical aspects of the disease, adverse effects of the treatments, and risk of cancer. It is noteworthy that some authors reported that concern over potential side effects was a very important issue for 91% of patients, while up to 45% reported they felt to be poorly informed about, or not informed about at all.8 These data highlight that patients want to receive more accurate information about the drugs used for IBD.
In our study, men felt that the currently available means covered their information needs to a significantly greater extent than women.
The subgroup of patients with a more severe course of disease (on treatment with an immunosuppressant or biological) made greater use of general practitioners, nursing services, and patients’ associations as information sources, which probably shows a better coping with the disease.
No significant differences were found between patients with CD and those with UC (as in the Bernstein8 study). However, the multicentre European study2 showed that CD patients made greater use of general practitioners and expressed greater interest in patients’ associations and in receiving information via the Internet.
To sum up, these data show the importance of gastroenterologists as information sources, the growing importance of the Internet as a reference tool for information about the disease, and the future needs and preferences of our IBD patients. Continued research of these aspects is required to adapt our clinical practice to their needs and preferences, ensuring an efficient information management that improves the doctor–patient relationship and the quality of life of these patients.
Conflict of interestThe authors declare no conflicts of interest.
Our sincere gratitude to María Pilar Ramón-Monllor, for having coordinated this study with such dedication.
List of centers and investigators of the Levante forum for the study of Chronic Inflammatory Bowel Disease:
Hospital Arnau de Vilanova de Valencia: Ignacio Catalán-Serra, Rafael Gil-Borras, Amparo Escudero and Miguel Bixquert.
Hospital General Universitario de Valencia: Jose M. Huguet, Patrícia Suárez, Ana Monzó, Luis Ferrer and Pilar Canelles.
Hospital Clínic Universitario de Valencia: Miguel Minguez, Joan Tosca, Maia Bosca, Isabel Pascual and Francisco Mora.
Hospital Morales Meseguer: Emilio Torrella.
Hospital Universitario Dr. Peset Valencia: Jose M. Paredes.
Hospital General Universitario de Elche: Mariana F. García-Sepulcre, Rolando Illescas and Narciso Vázquez-Romero.
Hospital Lluís Alcanyís de Xativa: Jose J. Ramírez, Miguel Pastor and Amparo Machancoses.
Hospital General Universitario de Albacete: Felix Calvo, María Nieves Martinez and Pedro Rivera.
Hospital Universitari i Politènic La Fe: Pilar Nos, Mariam Aguas, Guillermo Bastida, Belen Beltran and Marisa Iborra.
Hospital General Universitario de Alicante: Ana Gutiérrez
Hospital General Universitario de Castellón: Antonio Palau-Canós, Antonio Palau-Romero and María Alonso Burgal.
Hospital de Sagunto: Xavi Cortés and Jose R. Molés.
Hospital de Manises: Joaquín Hinojosa, Nuria Maroto, Isabel Ferrer and Maria Mora.