Casos Clínicos en Gastroenterología y Hepatología
Más datosJejunal diverticula are false diverticula as they are the herniation of the mucosa and submucosa through the muscular layer of the small bowel. The specific ethology is not well known, although small bowel dysmotility may be associated to this condition.1
It is an uncommon entity whose prevalence ranges from 0.4 to 4%.1 Jejunal diverticula are usually asymptomatic or cause unspecific symptoms, and the diagnosis of its complications may be a diagnostic challenge.
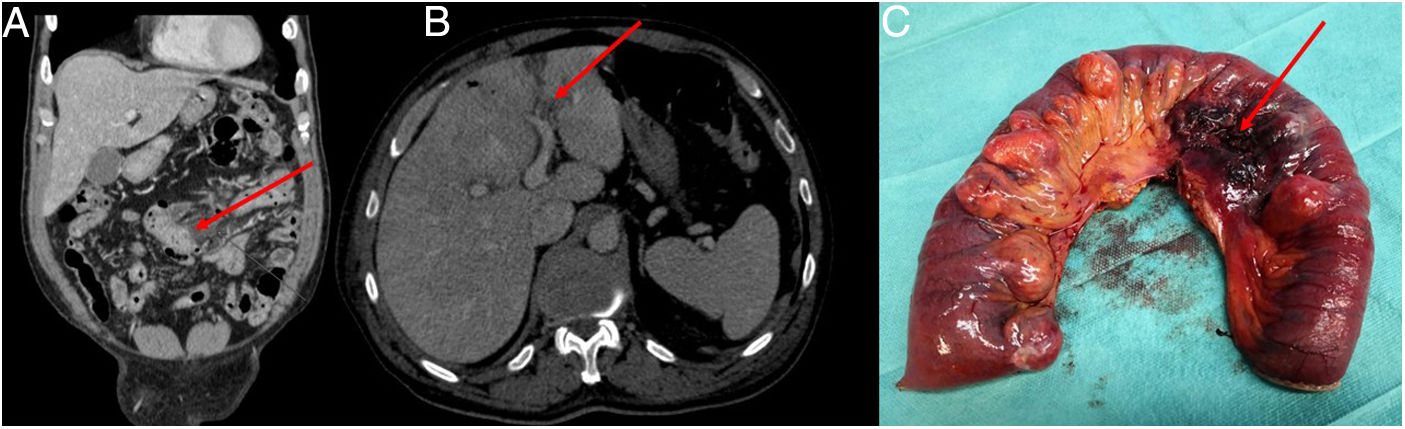
A 78-year-old man was admitted to hospital with abdominal pain and vomiting. Abdominal examination showed tenderness without peritoneal irritation signs. Laboratory data revealed a white count of 16.900/μl with absolute neutrophil count of 15700, the rest of parameters were within normal limits. An abdominal CT showed a contained perforation of jejunal diverticulum in relation to jejunal diverticulitis (JD), without evidence of fluid collections (Fig. 1A). Non-operative treatment based on intravenous antibiotics was tried. Consecutive blood tests showed an improvement of leucocytosis until 15.200/μl. However, 48h later the patient presented fever peaks and worsening in abdominal exploration. A new CT revealed the progression of the inflammatory process and partial thrombosis of the left portal vein (pylephlebitis) as a new finding (Fig. 1B).
Surgical exploration found multiple diverticula along a segment of 50cm of jejunum (Fig. 1C), especially along the mesenteric side of the intestine, associating a contained perforation of one of them and a small abscess. Intestinal resection with primary anastomosis was performed. Histopathological analysis informed of a perforated acute diverticulitis, with fibrino-leucocyte serositis and haemorrhage of the meso.
Small bowel diverticulosis prevalence varies from 0.4 to 4%.1,2,4 The proposed aetiopathogenesis is intestinal dyskinesia and very high intraluminal pressure, with diverticulum arising at the site where mesenteric vessels enter into the muscular layer.3
Jejunal diverticula are twice more common in men than women and usually present with complications in the 6th and 7th decade of life.1 They are usually multiple and can be associated to diverticula at other locations, such as colon, esphageous or stomach.2
Clinically, patients are usually asymptomatic, although up to 40% may present chronic symptoms such as unspecific abdominal pain or bowel dysmotility.3 The most frequent complications are acute diverticulitis associated or not to perforation, diverticular haemorrhage and small bowel obstruction. Jejunal diverticulitis (JD) cause similar signs and symptoms than other intra-abdominal infections. In this case, the patient presented not only an unusual intra-abdominal infection as JD is, but also a pylephlebitis, which is a rare but potentially severe condition associated with intraabdominal sepsis, mainly with colonic diverticulitis and appendicitis. In that sense, JD must be considered in the differential diagnosis of abdominal pain, and severe complications must be suspected when jaundice and fever appear.
Small bowel diverticula are usually diagnosed as an incidental finding on radiological or endoscopic exams.2 In case of acute JD, abdominal TC reveals asymmetric small bowel wall thickening, associated to oedema and rarefaction in the surrounding diverticular fat and even abscess, pneumoperitoneum or intraabdominal free fluid.4 When associated to pylephlebitis, TC may show a filling defect in the spleno-portal vein system or even portal gas.
The best option for treatment of acute JD is controversial. Conservative treatment, based on digestive rest ant antibiotics, has been widely accepted for non-complicated acute diverticulitis.4 However, there are not clinical guidelines for therapeutic management of perforated jejunal diverticulitis.1 In cases of acute diverticulitis associated to fluid collections, intravenous antibiotics with percutaneous drainage when required has been accepted as first line of treatment.1,4 Novak et al., reported two cases of perforated JD treated successfully with intravenous antibiotics and percutaneous drainage.5 In the same way, Levack et al managed just with antibiotherapy a case of acute diverticulitis associated to a small abscess.4,5 Intestinal resection with primary anastomosis is necessary in cases of perforation with free fluid causing generalised peritonitis.1,2,5 Resections must be limited to the affected part of the intestine if the diverticulosis is so extent to cause shirt bowel syndrome.2 Even though conservative management could be effective in cases of abscessed diverticulitis, most authors prefer early intestinal resections, reserving the conservative treatment for patients with high surgical risk.
FundingNone declared.
Author contributionsAll authors have contributed, read and approved the final manuscript.
Conflict of interestThe authors have no conflicts of interest to declare.