Casos Clínicos en Gastroenterología y Hepatología
Más datosAlthough bleeding due to portal hypertension is the main cause of bleeding in cirrhosis, there are other causes unrelated to portal hypertension that should be ruled out.1 It is important to perform an upper gastrointestinal endoscopy in the setting of the haemorrhage in a patient with advanced liver disease.1
43-Year-old man with alcoholic cirrhosis (Child–Pugh=B7, MELD=7). In the last 6 months he had presented mild ascites and two episodes of esophageal variceal haemorrhage for which he started secondary prophylaxis with propranolol and band ligation (last banding session 2 months ago).
He was admitted to the hospital suffering from hematochezia (hemoglobin 5g/dL, previous 9.7g/dL) followed by hemodynamic instability. Intravenous somatostatin and pantoprazole were started.
Upper gastrointestinal endoscopy was performed: small esophageal varices and a large subepithelial lesion suggestive of ectopic varix with red wale marks and a fibrin clot extends along the lesser gastric curvature from medium gastric body to incisura angularis. It was treated with cyanoacrylate injection but the bleeding was uncontrolled.
A transjugular intrahepatic portosystemic shunt (TIPS) was placed with a portal pressure gradient (PPG) decreased to 12mmHg (initial=20mmHg). Despite the above intervention, hematochezia and anemization persisted. Computed tomography angiography (CTA) was performed which revealed cirrhosis with portosystemic collaterals without contrast extravasation in arterial or venous phase. We performed a new liver catheterization (PPG=18mmHg) and TIPS revision with stent dilatation (final PPG=12mmHg). Residual gastric varices dependent on the short gastric vessels were embolized percutaneously with ethylene vinyl alcohol (Onyx®).
However, hematochezia and anemization persisted and a new revision of the TIPS showed its permeability (PPG=15mmHg). We decided to lengthen the TIPS given the risk of malposition with placement of an intra-TIPS stent without modifying the gradient.
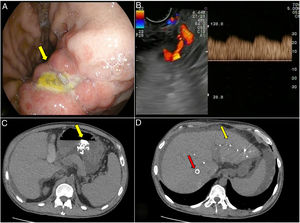
In addition, we performed an endoscopic ultrasound. The sclerosis zone, an ulcer, was located in the lesser gastric curvature (Fig. 1A). We observed in the wall of the vessel and adjacent thereto an echogenic nodular image (10mm×25mm) with hyperechoic areas that probably corresponded to the cyanoacrylate injected in previous endoscopic procedures. Adjacent to this area we identified a 5mm diameter vessel with arterial flow and direction towards the gastric wall in the ulcer (Fig. 1B).
(A) Upper gastrointestinal endoscopy image shows a large vessel extends along the lesser gastric curvature with an ulcer. (B) Endoscopic ultrasound with vessel with arterial flow and direction towards the gastric wall in the ulcer. (C) Particles of embolization in the gastric wall detected in the abdominal-CTA. (D) Particles of embolization in the liver parenchyma (yellow arrow) and TIPS (red arrow).
Arteriography allowed to identify an enlarged left gastric artery and a hypertrophied right gastric artery feeding an arteriovenous malformation with perigastric venous return. The afferents were successfully embolized by injecting Glubran-lipiodol® from the right gastric artery (endoscopist) and coils from the left gastric artery (angioradiologist).
No other malformations were detected in the thoracic-abdominal CTA (Fig. 1C and D) or cerebral magnetic resonance angiography.
The patient evolved well. However, a month later he was re-admitted due to melena. In upper gastrointestinal endoscopy an ischemic ulcer (70mm in greatest diameter) with 3 visible vessels was visualized in greater gastric curvature. Endoscopic treatment was not possible due to the ulcer's size and a subtotal gastrectomy was performed without complications.
After one year of follow-up, the patient has not presented bleeding recurrence.
Gastric arteriovenous malformations (GAVM) are an uncommon cause of upper gastrointestinal bleeding and represent 1–2% of all gastrointestinal malformations.2
The location and endoscopic presentation are very variable and range from flat or nodular bright red lesions, thickening of tumours, submucosal tumours, telangiectasia, etc. to the visualization of a vessel.2,3
Sometimes, GAVM can be associated with Rendu–Osler–Weber disease. This diagnosis is likely with two criteria: epistaxis, teleangectasias, visceral arteriovenous malformations or a first degree relative affected.4 Our patient only met one of these two criteria, being the rest of the complementary tests and the physical examination normal.
Although the diagnosis is usually initiated with an endoscopy, other techniques such as CTA and angiography are necessary.2 In this case, endoscopic ultrasound with colour Doppler confirmed the vascular nature of the structure and proved useful in guiding endoscopic therapy.
The treatment is usually surgical3 although the nidus can be devascularized utilizing embolization of a single feeding artery. However, if the arteriovenous malformation has multiple arteries or multiple shunts between the arteries and veins which supply the nidus, arteriovenous malformation may increase in size,5 as indicated in our case report. Intestinal ischemia is the most severe complication of embolization, occurring in 14–20% of cases.2
In conclusion, the endoscopic diagnosis of GAVM presents some difficulties due to the wide range of possible presentations. Its presence should be ruled out in cirrhotic patients in whom endoscopic and endovascular haemorrhage cannot be controlled. Additional diagnostic techniques should be applied (such an endoscopic ultrasound) before placing a TIPS for the treatment of ectopic varices or of bleeding from an unknown origin in order to discard a non-portal hypertension related haemorrhage. Embolization can control GAVM bleeding, although ischemic injury may require further surgery.
Grant supportNo funding received.
Conflicts of interestThe authors declare no conflicts of interest.