Somatostatin and somatostatin analogues are considered very useful for the treatment of hormone producing tumors and acute variceal bleeding. They have also been proposed for the treatment of acute pancreatitis and for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis although clinical trials have failed to show any efficacy. The authors report the case of a 45-year-old man, recently diagnosed of acromegaly, which developed an acute pancreatitis shortly after his first injection of lanreotide autogel. The patient developed a severe dilatation of his hypocontractile gallbladder with distension of the intra and extrahepatic biliary ducts, the choledochus and the main pancreatic duct, without lithiasis or other abnormalities at the papilla, which resolved spontaneously in a month. We consider that lanreotide most likely induced a functional spasm of the Sphincter of Oddi, with impairment of the biliary-pancreatic outflow, leading to an acute pancreatitis, and review the literature concerning this drug related pancreatitis.
La somatostatina y los análogos de la somatostatina se consideran muy útiles para el tratamiento de tumores productores de hormonas y de hemorragias agudas por varices. También se han propuesto para el tratamiento de la pancreatitis aguda y para la prevención de pancreatitis tras una colangiopancreatografía retrógrada endoscópica, aunque los estudios clínicos no han podido demostrar eficacia alguna. Los autores reportan el caso de un hombre de 45 años de edad, con un diagnóstico reciente de acromegalia, que desarrolló una pancreatitis aguda poco después de su primera inyección de lanreótida autogel. El paciente desarrolló una severa dilatación de la vesícula biliar hipocontráctil con distensión de las vías biliares intra y extrahepáticas, el colédoco y el conducto pancreático principal, sin litiasis ni otras anormalidades en la papila, y que se resolvió espontáneamente al mes. Consideramos la posibilidad de que la lanreótida causara un espasmo funcional del esfínter de Oddi, que afectase el flujo biliar-pancrático y condujese a la pancreatitis aguda, y revisamos la literatura sobre pancreatitis relacionada con este fármaco.
Somatostatin and somatostatin analogues have proven to be very effective in the treatment of various hormone-producing tumors (e.g. pituitary or gastrointestinal tumors) and in lowering the rates of complications associated with acute variceal bleeding. It has even been speculated that they could have a beneficial effect in the prevention and/or treatment of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis, but the results of several clinical trials, so far, remain controversial and its real importance is open to discussion. Nevertheless, in these last years, a small number of case reports describing acute pancreatitis induced by somatostatin analogues (both octeotride and lanreotide) have been published, leading to more concerns regarding the effects of these agents at a biliary and pancreatic level. We describe the case of a 45-year-old acromegalic man who developed an acute pancreatitis shortly after his first administration of lanreotide autogel and review the literature concerning this rare, but sometimes lethal, association.
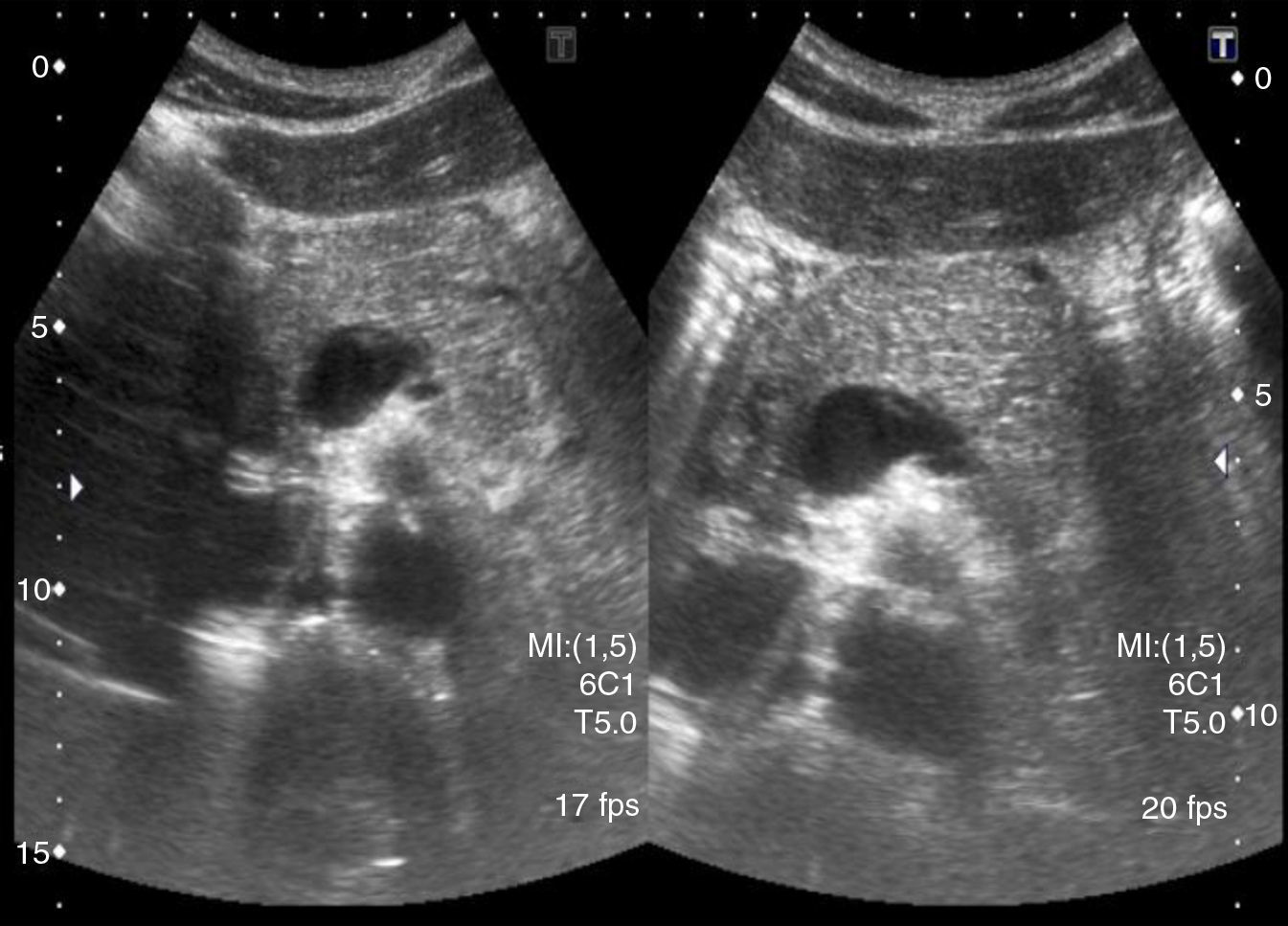
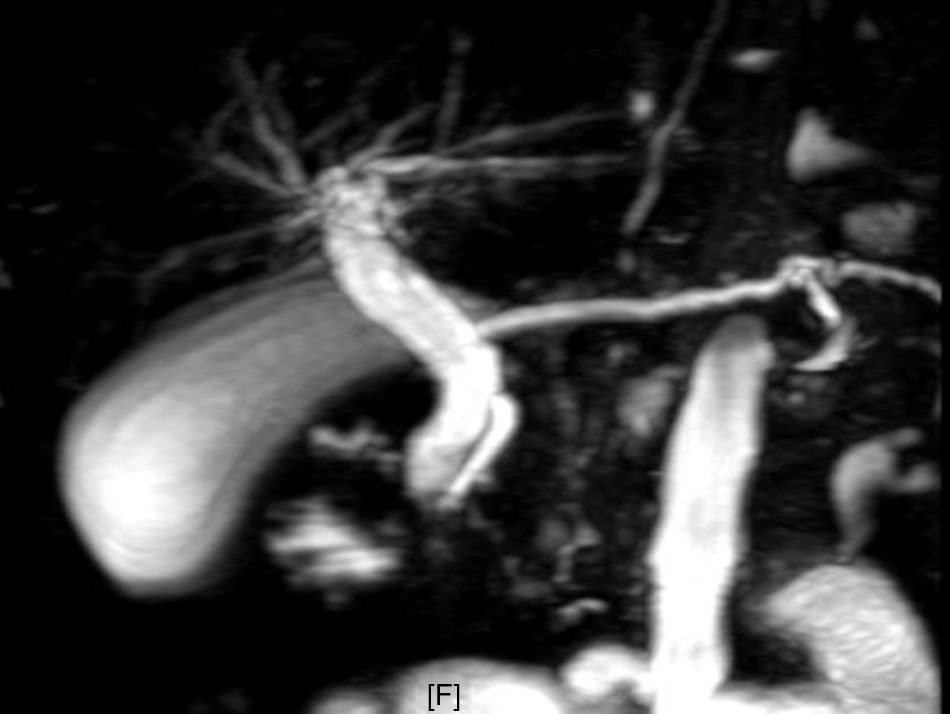
Case reportA 45-year-old man attended the Emergency Department (ED) of our Hospital complaining of a severe epigastric pain. The patient had recently been diagnosed of acromegaly due to a pituitary macroadenoma and his endocrinologist had prescribed him lanreotide autogel 90mg every 28 days, while waiting for neurosurgery. The patient mentioned that the abdominal pain had started just 7h after his first administration of the drug. He denied any alcohol intake. Physical examination was normal, except for some tenderness in the epigastric area. The serum amylase level was 1340UI/I, with normal glucose, renal function, electrolytes and transaminases values. A transabdominal ultrasonography performed at that moment revealed a normal gallbladder and non-dilated biliary tree (Figs. 1 and 2). No lithiasis was seen. The patient was admitted to our Department with the diagnosis of acute pancreatitis of unknown origin/etiology. The next day, amylase reached 2030UI/I, without transaminasemia. 72h after admission the patient was well and mentioned that the epigastric pain had improved. An abdominal computed tomography (CT) and a magnetic resonance cholangiopancreatography (MRCP), performed 4 days after admission, showed a distended gallbladder accompanied by severely dilated intra and extrahepatic bile ducts and a choledochus duct with a diameter of approximately 2cm, which was distended up to its intrapancreatic terminal segment (Figs. 3 and 4). Although biliary sludge was noticed, no gallstones and no distal calculi within the choledochus were seen in both the procedures. The main pancreatic duct (MPD) was also dilated but no pancreatic fluid collections or signs of necrosis were reported. Aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyltransferase (GGT) and alkaline phosphatase (AP) had increased to 113UI/I, 223UI/I, 112UI/I and 164UI/I, respectively. Amylase was at that moment of 474UI/I. Bilirubin, calcium and triglycerides were normal. The study for an autoimmune disease (antinuclear antibodies, anti-DNA antibody, anti-Smith antibody, rheumatoid factor, anti-liver-kidney microsomal type 1 antibody, anti-smooth muscle antibody, antimitochondrial antibody, anti-carbonic anhydrase II antibody) was considered negative. Transdermal patches of glyceryl trinitrate (5mg the first 2 days and 10mg the following days) were prescribed due to the suspicion of a functional obstructive spasm of the Sphincter of Oddi (SO). 10 days after admission a new transabdominal ultrasonography was requested, revealing a distended gallbladder and a dilated choledochus of 1.6cm up to its intrapancreatic part, without any visible lithiasis (Fig. 5). A Boyden meal test, consisting of the ingestion of three beaten up eggs in milk followed by three successive echographies separated by an hour and an half approximately, in order to study the evacuation time of the gallbladder, showed a very small gallbladder contraction with a very small diminished choledochus diameter (1.5cm). Again, no abnormalities were seen around the papilla. During this time, the patient was asymptomatic, denying any abdominal pain and tolerating oral feeding, without nausea or vomiting. A new laboratory test, extracted 7 days later, revealed that the transaminases and the cholestatic liver enzymes had lowered: AST, ALT, GGT and AP of 41UI/I, 128UI/I, 95UI/I and 114UI/I, respectively. The patient was discharged pending a blood test the following week and a new abdominal ultrasound examination. Lanreotide was not reintroduced. The laboratory test results continued to improve, with AST, ALT, GGT and AP of 20UI/I, 56UI/I, 61UI/I and 107UI/I. At last, the new transabdominal ultrasonography, performed two weeks after discharge, revealed a normal diameter, stone-free gallbladder, with an intrahepatic bile duct that was not dilated, a choledochus that globally did not appear dilated, with a maximum diameter of 0.8cm and a MPD of 1.5mm. The patient remained asymptomatic and had not needed to attend the ED again.
The incidence of acute pancreatitis in the past two decades has been increasing, accounting every year for approximately 200,000 hospital admissions in the USA.1 The most frequent causes of pancreatitis in adults are migrating gallstones that obstruct the common bile duct, the pancreatic duct or both (38% of all cases) and alcohol abuse (36% of all diagnosed pancreatitis, almost 10% of all chronic alcohol abusers).2 Drugs rarely induce acute pancreatitis, and most studies rely on case reports of few patients. Most of the drugs related reactions are idiosyncratic.2
Lanreotide, a somatostatin analogue, is very effective in treating acromegaly, lowering significantly the GH and IGF-1 levels in the serum and inducing the shrinkage of the pituitary tumor in half of the followed patients, which is accompanied by a significant improvement of the headache, the fatigue and the peripheral soft-tissue swelling that most patients complain of.3 Lanreotide autogel is a long-acting aqueous-gel preparation of lanreotide acetate, which reaches a maximum plasma level in about 6h and has a half-life of 33±14 days, allowing for injections every 28 days, although maintaining a high drug serum level during this period of time.4 Most side effects are mild, such as pain at the injection site, nausea, transient diarrhea and abdominal discomfort that usually resolves in 8–10 weeks, but up to 20% of patients can develop gallbladder sludge or asymptomatic gallstones, especially within 18 months of continuous treatment.3,5 The most serious, but fortunately uncommon, side effect is an acute, alithiasic pancreatitis, described in a series of case reports and in long-term effectiveness and tolerability studies.6
Since the first published case of octeotride-induced acute pancreatitis in 1991 by Gradon et al.,7 many studies have been conducted in an attempt to explain the pathophysiology of the pancreatitis induced by somatostatin analogues. SO manometric studies, like the ones performed by Di Francesco et al.8 and Binmoeller et al.,9 have proven that the acute administration of octeotride induces a high phasic contraction frequency at the SO, in all cases with more than 7 contractions/min. This “tachyoddia” reduces the diastolic filling time between contractions, thus impairing biliary and pancreatic drainage.8 These findings have been confirmed by ultrasonography-secretin test pattern studies, like the one performed by Cavallini et al.,10 which reported that the administration of a single dose of octeotride interfered with the SO mechanisms, inducing a persistent dilatation of the MPD even before secretin stimulation, and by quantitative hepatobiliary scintiography (QHBS) studies,11 which demonstrated a significant increase of the half-life of bile excretion, essentially in the hepatic hilum and the common bile duct, but not the liver parenchyma, indicating a continued spasm of the SO. The diminished pancreatic outflow and the collection of pancreatic juice within the MPD would lead to an increase of intraductal pressure,8 one of the many mechanisms that has been considered to be the cause of the inappropriate and unregulated activation of trypsinogen to trypsin within the pancreatic acinar cells,2,12 the first step of an acute pancreatitis. This would be rapidly followed by intra and extrapancreatic inflammation (interestingly, 5 of the 6 patients that participated in Di Francesco's manometric study developed a mild acute pancreatitis after the procedure, attributed to the reduction of pancreatic juice drainage8). The augment of the SO basal pressure and of the phasic contractile activity caused by octeotride could be related to its inhibitor effect over cholecystokinin (CKK) and vasoactive intestinal peptide (VIP), both substances that increase the gallbladder motility and relax the SO.11 The altered bile formation, the decreased motility of the gallbladder and the diminished excretion of bile into the duodenum could explain the tendency to gallstone formation during somatostatin analog treatment.9,11 Lanreotide's effect on the SO is most likely similar to the one produced by octeotride and would explain why the same patient can develop pancreatitis to both these agents on separate occasions.13,14
Velõsy et al. have also found that the administration of glyceryl trinitrate after octeotride led to the augment of the transpapillary bile flow, proposing that the nitric oxide donated by the first had a relaxing effect on the SO, overwhelming the functional spasm induced by octeotride.11 However, this phenomenon remains to fully demonstrate.
Our patient developed an acute pancreatitis shortly after his first administration of lanreotide, which indicates a close temporal relationship between the administration of the agent and the onset of the pancreatitis. No predisposing factors for pancreatitis such as gallstones, alcohol abuse, hypertriglyceridemia, hypercalcemia, autoimmune diseases or family history of pancreatitis were found. The decrease of our patient's gallbladder motility and the changes of the pancreaticobiliary tree reported by the different imaging studies (that were not present at the moment of admission and that had resolved spontaneously 37 days after the administration of the drug), could all be explained by the lanreotide's effect on the gallbladder and the SO, by the same mechanisms that we have previously explained. Although biliary sludge, which is commonly seen in patients with recurrent acute pancreatitis of unknown origin,2 was described in the abdominal CT and the MRCP performed 4 days after admission, we considered that in the case of our patient it was due to biliary stasis, since it was not seen in the first or the last transabdominal ultrasonography. We also decided not to perform an ERCP with sphincterotomy since our patient became asymptomatic shortly after his admission, showed a progressive improvement of his liver function and because his acute pancreatitis was not related to lithiasis but rather a time-limited SO dysfunction. We were particularly concerned that the ERCP could worsen his previous pancreatitis. Nevertheless, we regret the fact of not being able to perform a manometric study of our patient's SO, which could have been helpful in confirming the increase of the basal pressure and frequency of the phasic contractions of the SO. At last, the improvement of the transaminases and the cholestatic liver enzymes levels after starting treatment with transdermal patches of glyceryl trinitrate could be related to this agent's relaxing effect on the SO, but as we have previously mentioned, the role of nitrates remains controversial.
As for the use of somatostatin and somatostatin analogues for the treatment of pancreatitis, several clinical trials have failed to show any efficacy in altering the course of the disease1 and, at the present moment, the use of these agents for the prevention of ERCP-induced pancreatitis is not supported by any published study.12 Post-ECRP pancreatitis can be avoided by a careful selection of patients, by mastering the technique (complications are relatively low when the procedure is performed by an experienced and competent endoscopist1,12), by prescribing periprocedure nonsteroidal anti-inflammatory drugs in low-risk ERCPs and by prophylactic pancreatic stent placement in high-risk ERCPs.15
In conclusion, the authors would like to point out that the diagnosis of acute pancreatitis should always be considered in patients who complain of abdominal pain while exposed to a somatostatin analog agent, and would also like to suggest, in this type of patients, a careful and continuous monitoring of gallstones.