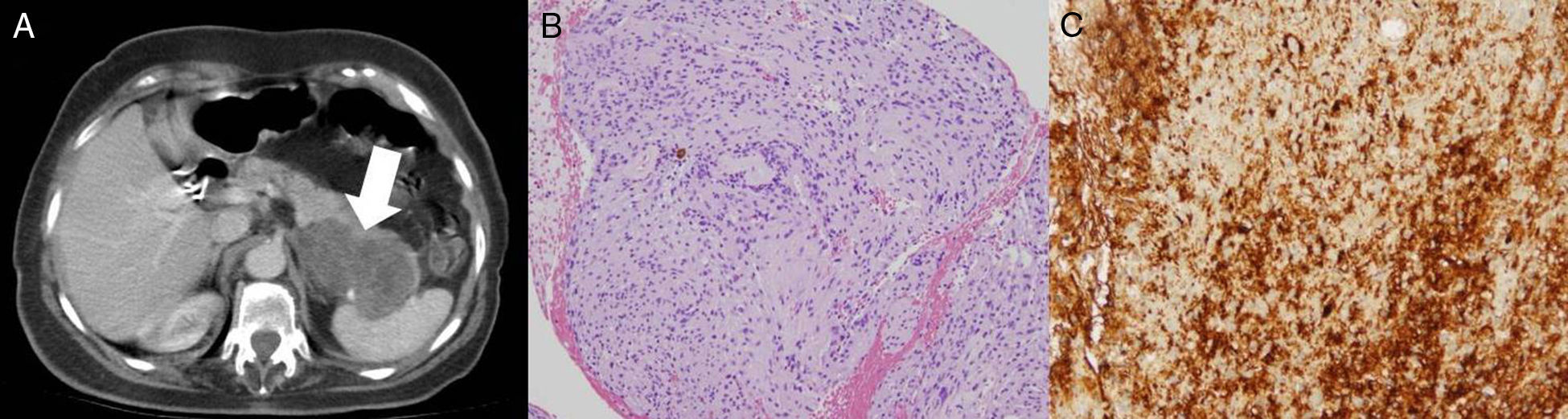
A 75-year-old woman with a history of hypertension, osteoporosis, and cholecystectomy presented with intermittent abdominal pain unrelated to meals and weight loss of 6kg over the past four months. Physical examination and all laboratory investigations were normal. Upper endoscopy was normal, whereas an abdominal ultrasound revealed a 6-cm, irregular, solid mass in the tail of the pancreas. Computed tomography (CT) scan (Fig. 1A) showed a 7×5cm diameter, encapsulated, solid heterogeneous tumor, without any cystic component. There were no other intra-abdominal lesions or pathologic lymphadenopathy noted. Magnetic resonance cholangiopancreatography showed normal caliber of the biliary tree and pancreatic duct. CT-guided fine-needle aspiration exhibited cellular spindle cell neoplasm with mild atypia (Fig. 1B). On immunochemistry, the spindle cells were strongly positive for S-100 protein (Fig. 1C) and negative for pan-cytokeratin, CD-34, CD-117, smooth muscle actin and Melan A, consistent with the diagnosis of a pancreatic schwannoma. Distal pancreatectomy with splenectomy was performed and the patient recovered uneventfully, without relapsing disease after a 2-yr follow-up.
(A) Abdominal computed tomography (CT) scan showing a 7×5cm solid heterogeneous mass in the pancreatic tail. (B) Spindle cell neoplasm on tissue obtained with CT-guided fine needle aspiration. (C) Strong positivity of spindle cells for S100 on inmmuno-staining, consistent with schwannoma.
Schwannomas (also called neurilemmomas) are encapsulated tumors made entirely of benign neoplastic Schwann cells, which represent the most common peripheral nerve tumors. They grow eccentrically from peripheral nerves or nerve roots with the nerve itself usually incorporated into the capsule. The most frequent locations for schwannomas are lower and upper limbs, head and neck, retroperitoneum, mediastinum, and pelvis.1 Symptoms and signs are caused by direct nerve invasion, involvement of surrounding tissues, or mass effect. Benign pancreatic schwannoma is a rare entity, with around 50 cases reported in the English literature in 2016.2 We have only found two previous reports of pancreatic schwannomas in Spain.3,4 Malignant transformation has been seldom reported in literature. The pancreatic head is the most common location (40%), followed by the body (20%), being tail and uncinate process the least common locations. The most common symptom is abdominal pain and jaundice with proximal tumors, but these lesions can also be found incidentally. As for CT findings, tumors that are predominantly or exclusively composed of Antoni A areas (cellular component) show inhomogeneous, hypodense, solid masses with contrast enhancement, whereas tumors predominantly composed of Antoni B areas (loose myxoid) may exhibit homogeneous cystic masses without significant contrast enhancement.5 Immunohistochemically, pancreatic schwannomas are positive for S100, Vimentin and CD 56. Conversely, spindle cells in pancreatic schwannomas stain negative for cytokeratin, CD117, desmin, CD34, AE1/AE3, alpha smooth muscle actin, and smooth muscle myosin. The management of pancreatic schwannomas should be strictly guided by symptoms and histologic results. With most of the tumors having a benign histology, tumor enucleation is the most common surgical procedure performed for symptomatic lesions. In cases where the tumor shows a malignant behavior (infiltration of tissue or close proximity to important vessels), margin negative resection is recommended. Malignant transformation of pancreatic schwannomas has been seldom reported in literature.6