Primary malignant melanoma of the esophagus (PMME) accounts for only 0.1–0.2% of all malignant esophageal tumours.1 Symptoms are usually dysphagia and retrosternal pain.
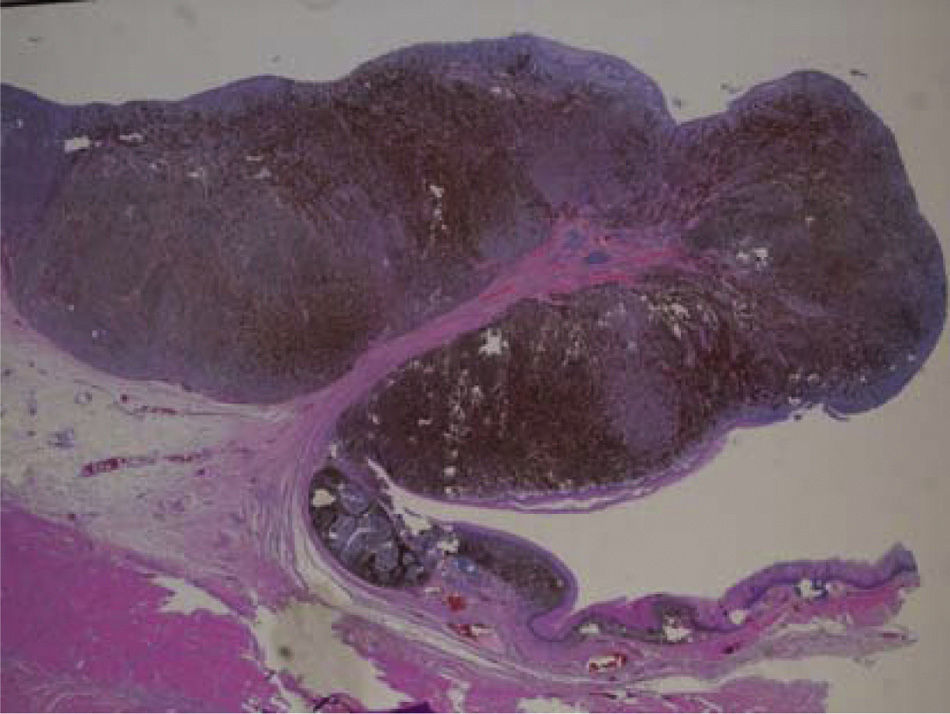
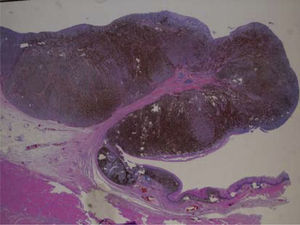
We present the case of a 68-year-old man, who was seen for symptoms of dysphagia beginning one month previously. Upper endoscopy revealed a 3-cm lesion with a polypoid appearance, 35cm from the dental arch. The surrounding mucosa had a bluish appearance, suggestive of increased vascularization at this level. The biopsy (Fig. 1) showed areas of melanosis and foci of activity at the junction, pointing to a primary esophageal origin. Skin and ophthalmological examination revealed no evidence of melanoma.
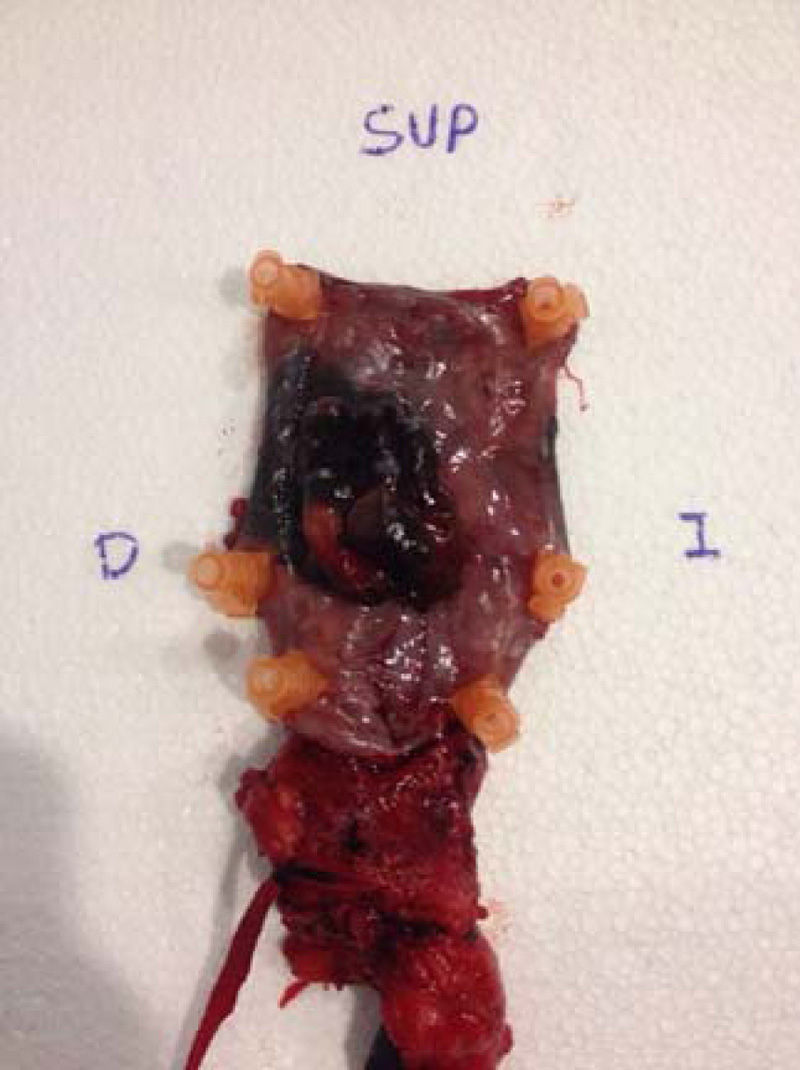
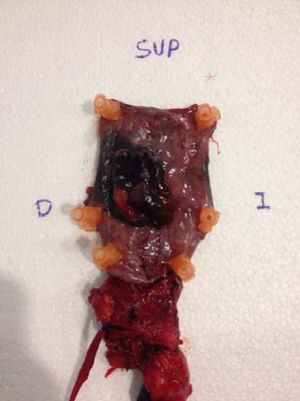
The thoracoabdominal computed tomography scan showed irregular thickening (2.5cm) of a 6-cm segment of the distal esophagus (extending to the cardia from 5cm distal to the carina) and mediastinal lymphadenopathies (right upper paratracheal, 0.9cm; lower paratracheal, 1.2cm and calcified; and para-esophageal, 1.1cm). The patient underwent transhiatal esophagectomy and subsequent transmediastinal tubular gastroplasty with cervical esophagogastric anastomosis. Histological analysis of the surgical specimen (Fig. 2) confirmed a diagnosis of primary melanoma with lymphatic invasion. Immunohistochemistry (IHC) staining was positive for S100, HMB45 and Ki67. The patient remained 22 days in intensive care, where he underwent a radiological swallowing study that revealed stenosis of the gastric plastica with pre-stenotic dilatation, requiring endoscopic dilatation. Following chemotherapy due to lymphatic invasion, the patient died from nosocomial respiratory infection 6 months after diagnosis.
Primary melanoma of the esophagus is a rare disease with high mortality. It presents between the sixth and seventh decades of life, predominantly in men (2:1 ratio).2 Cases have occasionally been described in young people and even children. The disorder usually involves the lower two thirds of the esophagus (86% of cases),3 and manifests clinically with dysphagia, weight loss, retrosternal pain and, occasionally, upper gastrointestinal bleeding. Macroscopically the tumour is polypoid, intraluminal, lobulated and usually pigmented.4,5 It is often diagnosed–as in our case–via endoscopic biopsy, although diagnosis for lesions with no pigment granules may be complicated; in these cases, IHC with HMB45 and S100 positive staining is useful. Around 40% of patients present lymphatic spread at diagnosis; the first organ affected is the liver, followed by the mediastinum, lung and brain in that order.1,4 Primary melanoma is defined according to the criteria described by Allen and Spitz,6 namely, that the lesion should have the structure of a melanoma and contain melanin pigment, present an area with junctional activity on the squamous epithelium and with melanocytes in the adjacent epithelium, and have a polypoid configuration. Although the most common form of presentation at diagnosis is a protruding mass, primary melanoma has also been described in the form of flat lesions.7 This fact, together with the rare nature of the condition, results in a high percentage of initial diagnostic error and poor prognosis. Melanoma should be ruled out in at least the skin, eye, anus and vagina. Surgical resection is the treatment of choice and is the only treatment that affects survival. Five-year post-operative survival is 37%.1 In some patients with inoperable tumours, intraluminal brachytherapy, radiotherapy, chemotherapy, immunotherapy or metal stenting may relieve the dysphagia. Nonetheless, prognosis for this type of tumour is poor, essentially due to its metastatic capacity.
Please cite this article as: Revilla Morato C, Mora Soler A, Prieto Bermejo AB, Piñero Pérez C, Pérez Corte D, Acosta Materán R, et al. Melanoma maligno primario esofágico: una causa infrecuente de disfagia. Gastroenterol Hepatol. 2016;39:47–48.