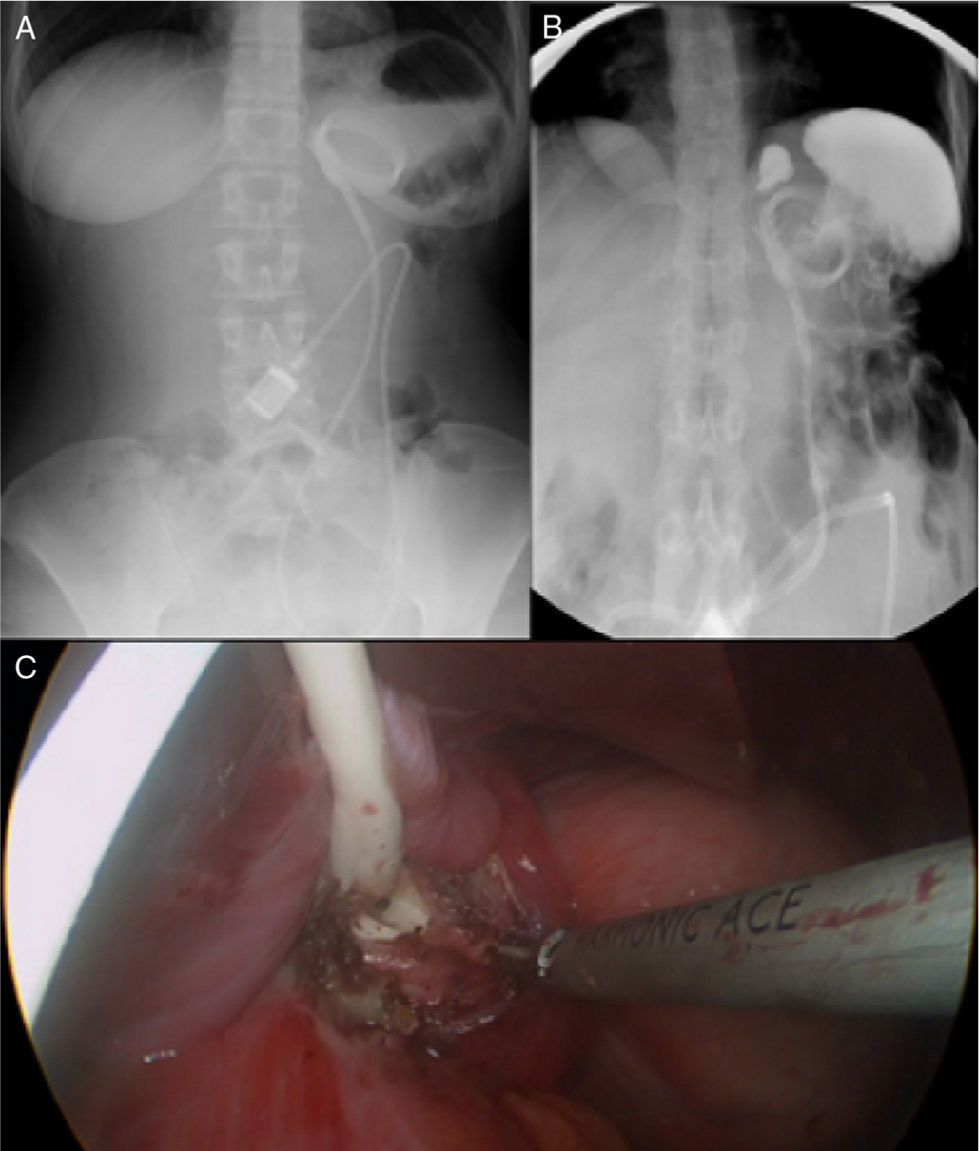
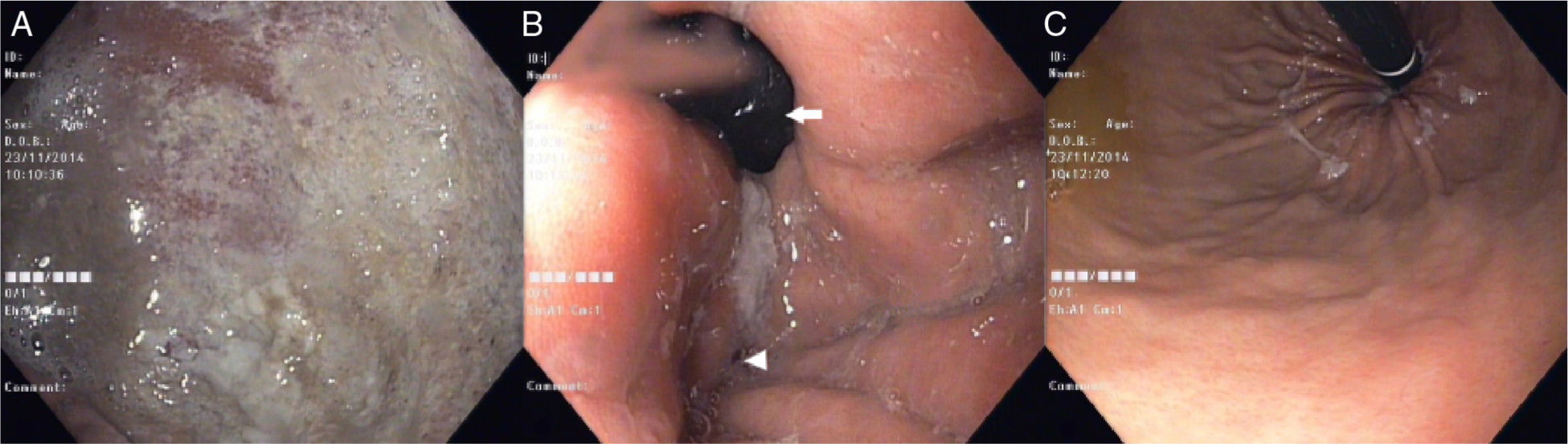
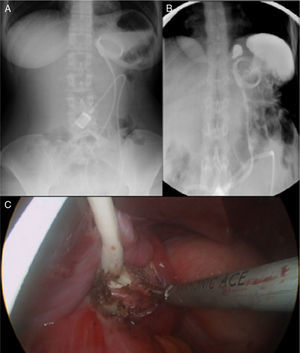
A 37-year-old woman with a laparoscopic adjustable gastric band (LAGB) placed 3 years earlier presented with a 1-day history of sudden onset vomiting, food intolerance and abdominal pain. Physical examination revealed epigastric tenderness and laboratory tests had no significant abnormalities. Abdominal X-ray showed a dislodged gastric band with an abnormal angulation and annular appearance (Fig. 1A). Upper gastrointestinal endoscopy revealed an enlarged eroded gastric pouch (Fig. 2A) with food stasis and an angulated constriction in the distal gastric body, easily traversed (Fig. 2B and C). Barium swallow confirmed the gastric band slippage with gastric pouch enlargement and no progression of oral contrast material into the distal stomach (Fig. 1B). The gastric band was surgically removed (Fig. 1C).
(A) Abdominal radiograph showing an enlarged gastric pouch with an air-fluid level and a dislodged gastric band with an abnormal angulation and annular appearance; (B) barium swallow depicting gastric band slippage with gastric pouch enlargement with retention of oral contrast; (C) laparoscopic image showing removal of the gastric band.
(A) Endoscopic image revealing an enlarged gastric pouch with mucosal erosions; (B) endoscopic image revealing herniation of the distal stomach (arrow) proximal to a narrowed impression (arrowhead) in the distal gastric body secondary to band displacement; (C) endoscopic image after retroflexion of the scope in the antrum, showing an easily traversed angulated constriction in the distal gastric body.
LAGB is an effective, safe and widely used bariatric surgery for treatment of morbid obesity.1,2 LAGB is positioned 1–2cm distal to the gastroesophageal junction, creating a gastric pouch approximately 20–30mL in size.3,4 A correctly positioned LAGB has a rectangular shape and an oblique angulation in the left upper quadrant on frontal abdominal X-ray.1 LAGB slippage is the most commonly reported complication of LAGB placement, affecting 2–4% of patients.3,4 LAGB slippage consists of prolapse of the distal stomach upward through the band, leading to eccentric pouch enlargement and constriction with partial or complete obstruction at the level of the band.1,2,4 While abdominal X-ray may reveal an air-fluid level in the gastric pouch, gastric obstruction and malposition of the band, endoscopy may depict an enlarged pouch, reflux esophagitis, gastritis, ulcers and necrosis.1,4,5 This report outlines the typical findings in gastric band slippage allowing clinicians to recognize similar aspects leading to early recognition of this complication and avoiding a potential deleterious delay in the institution of the appropriate management.