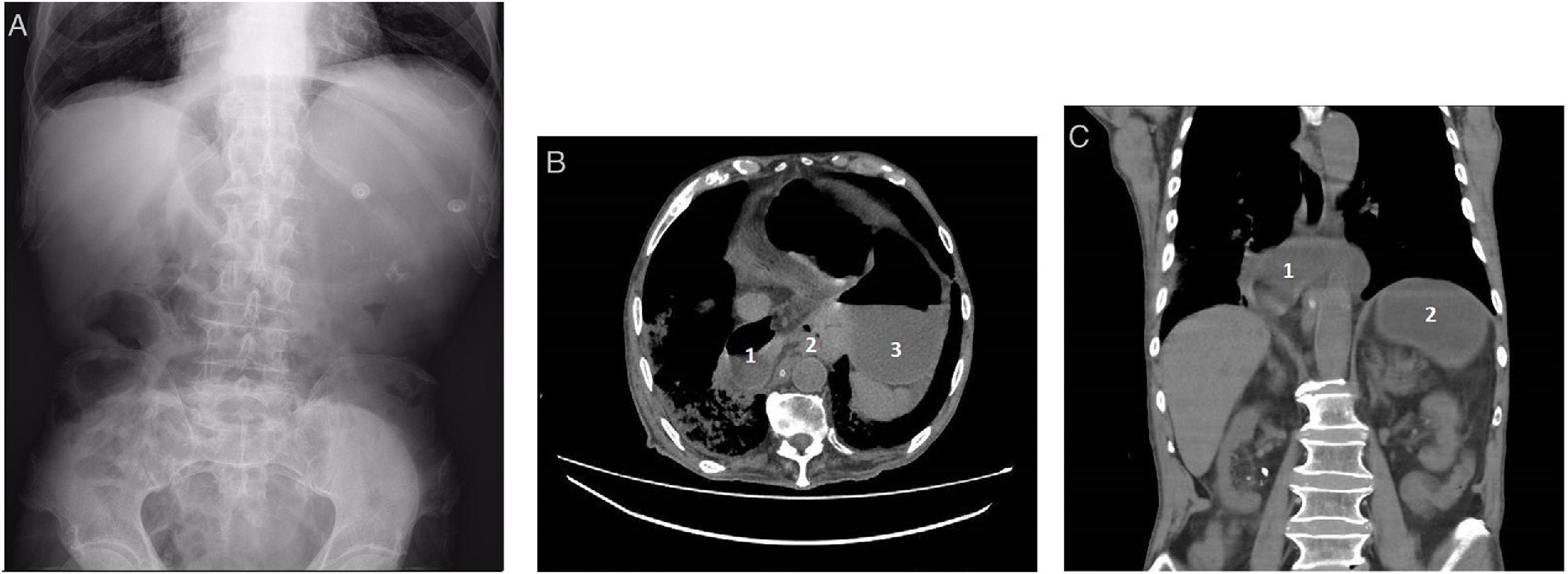
A 89-year-old man presented to the Emergency department with a 2-day history of vomiting and mild epigastric pain. He reported no fever, weight loss, diarrhea, melena or rectal bleeding. His past medical history was remarkable for chronic kidney disease, dilated cardiomyopathy and moderate dementia. Physical examination revealed a distended upper abdomen with dullness to percussion and epigastric pain with no rebound. Laboratory findings were within normal range but the abdominal X-ray showed a large gas bubble located in the epigastrium corresponding to a dilated stomach (Fig. 1A). A CT scan showed a 180° gastric rotation with the double air-fluid level sign, suggesting a mesenteroaxial volvulus, identifying the antrum displaced below the gastroesophageal junction (Figs. 1B and 1C). Considering age and comorbidities, the patient benefited from a non-surgical approach. An upper endoscopy allowed gastric derotation and resolution of the volvulus. A nasogastric tube was placed, per oral nutrition was progressively restarted and 10 days later an endoscopic gastrostomy was performed to fix the stomach to the abdominal wall and prevent further episodes. The patient was discharged with no other issues and was able to return to his usual activity.
(A) Abdominal X-ray with a large gas bubble corresponding to a dilated stomach. (B) Axial CT-scan showing an abnormal stomach disposition with accumulation of fluid and gas within the distended gastric cavity. 1, Ascended antrum on the right side of the abdomen; 2, Gastric volvulus’ axis of rotation; 3, Descended fundus on the left side of the abdomen. (C) Coronal CT-scan showing a mesenteroaxial gastric volvulus, where the stomach rotates around its short axis (perpendicular line connecting its greater and lesser curvatures). 1, Ascended antrum; 2, Descended fundus.
The authors declare no conflicts of interest.