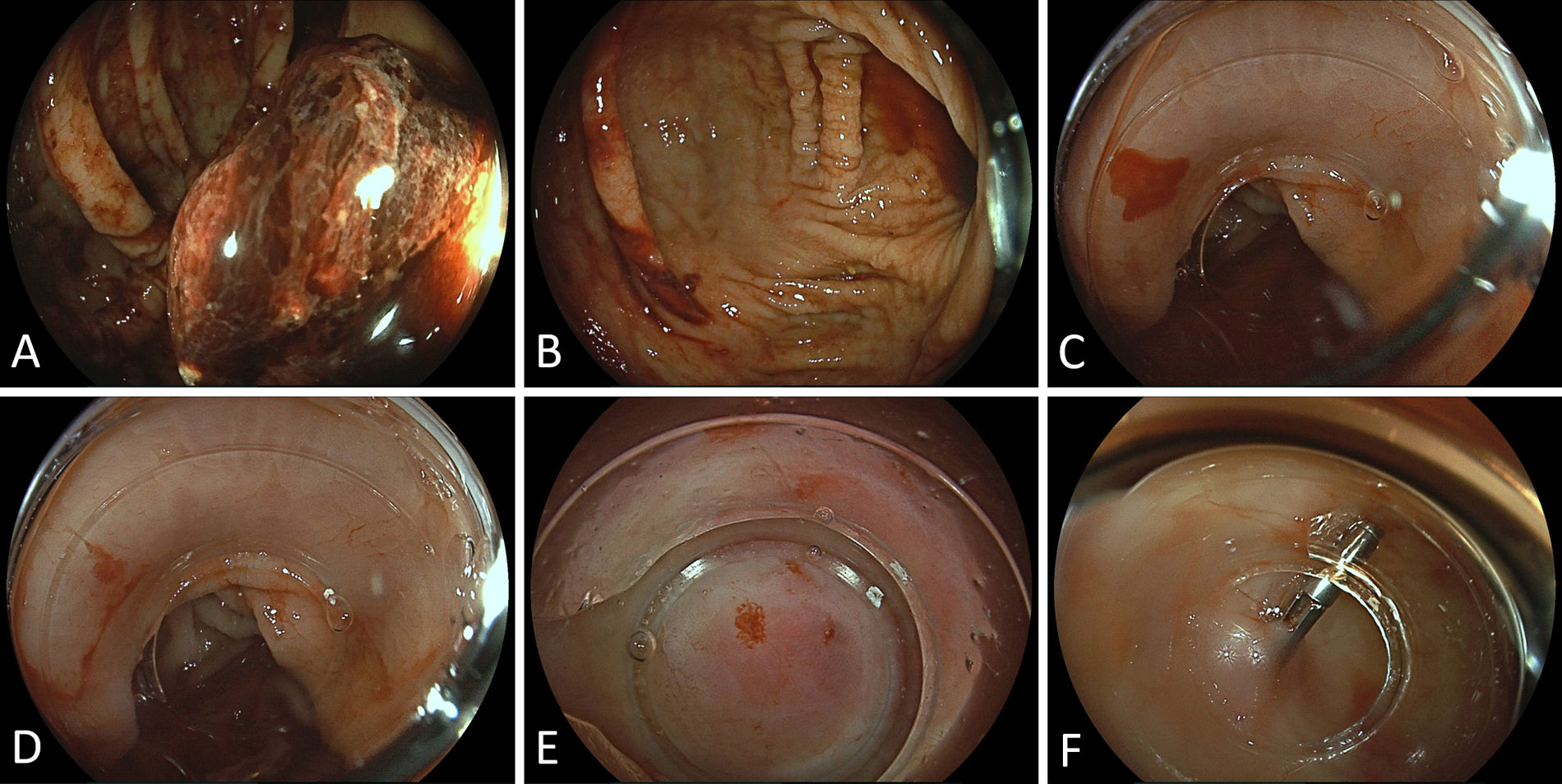
A 59-year-old male patient was referred with signs of gastrointestinal bleeding (tarry stools with admixed clots) under triple antithrombotic therapy including aspirin (100mg), clopidogrel (75mg) and warfarin (international normalised ratio at admission 3.07). Medical history included chronic atrial fibrillation and multivessel coronary artery bypass grafting (CABG) four weeks before, complicated by early graft occlusion necessitating emergent re-do surgery. With an index haemoglobin of 9.6g/dL, the hemodynamically stable patient underwent emergent esophago-gastro-duodenoscopy (EGD) demonstrating multiple erosive lesions in the antrum, however, without signs of recent haemorrhage. At the time, with a view to the patient's marked vulnerability in terms of thrombembolism, a decision was made to maintain triple antithrombotic therapy and to perform an urgent ilecolonoscopy after rapid bowel preparation. This was significant for an adherent clot opposite to the ileocecal valve (Fig. A), however, no clear-cut bleeding source could be identified in the critical area at a redundant fold (Fig. B). Therefore, we switched to a cap-fitted approach which proved instrumental in pinpointing an actively spurting lesion (Fig. C), however, the distinct nature of which could not be fully characterised even when applying variable degrees of compression (Fig. D). After moderate injection with a saline–suprarenin mixture to mark the area and provide temporary hemostasis, a tiny, though typical vascular lesion (“angiodysplasia”) came to our notion (Fig. E). Albeit argon plasma coagulation (APC) is considered the standard modality of endoscopic hemostasis, we opted for deployment of a large hemoclip in consideration of the very small lesion size and concerns for delayed bleeding risks related to potential APC-related ulceration (Fig. F). While the patient had an intercurrent drop in Hb levels to a minimum of 8.0g/dL, warranting transfusion of one unit of packed red cells, the further course was favourable with no signs of ongoing/recurrent bleeding. With regard to the achieved enduring endoscopic hemostasis, the extensive antithrombotic regime vis-à-vis very high risks of thromboembolic complications could be fully maintained throughout the GI bleeding episode, which is rarely considered in recent practice recommendations for moderate-to-severe bleeding complications.1
Conflict of interestNothing to declare.