Knowing the natural history of ulcerative colitis (UC) is essential to understand the course of the disease, assess the impact of different treatment strategies and identify poor prognostic factors. One of the most significant matters in this regard is the need for surgery.
ObjectivesTo analyse the Colectomy Incidence Rate (CIR) from diagnosis to end of follow-up (31/12/2017) and identify predictive factors for colectomy.
Material and methodsA retrospective study enrolling patients with a definitive diagnosis (DD) of UC or Unclassified Colitis (UnC) in the 2001−03 Navarra cohort.
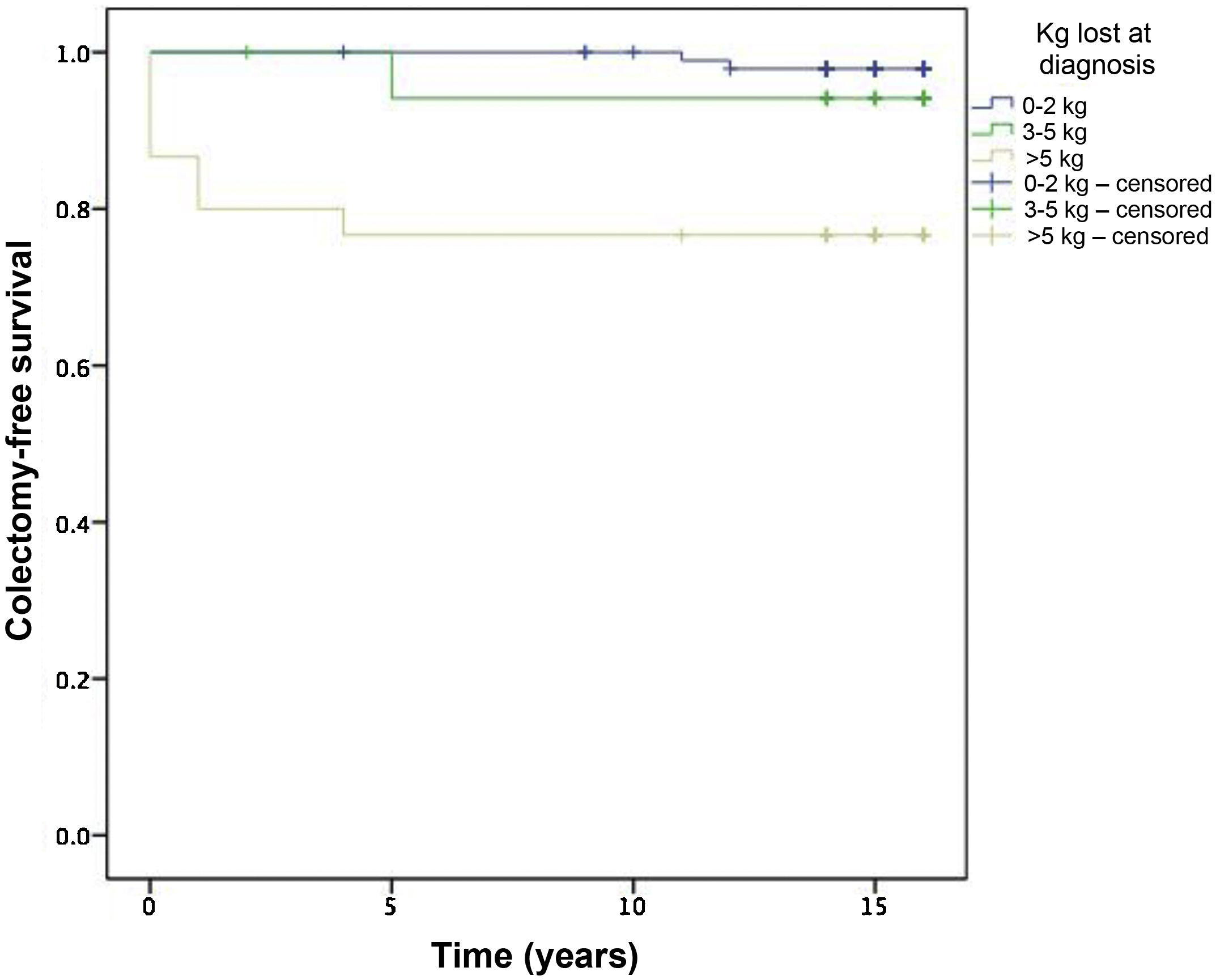
ResultsWe enrolled 174 patients with a DD of UC (E2 42.8%; E3 26.6%) and 5 patients with a DD of UnC: 44.1% women, median age 39.2 years (range 7–88) and median follow-up 15.7 years. A total of 8 patients underwent surgery (CIR 3 colectomies/103 patient-years: 3 at initial diagnosis (<1 month), 2 in the first 2 years, 2 at 5 years from diagnosis and 1 at 12 years from diagnosis. All had previously received steroids; 5 had received immunomodulators and 2 had received biologics. In 7 patients (87%), surgery was performed on an emergency basis. The indication was megacolon in 3 (37.5%), severe flare-up in 3 (37.5%) and medical treatment failure in 2 (25%). In 5 cases (62.5%), an ileoanal pouch was made, and in 3 cases, a definitive ileostomy was performed. In the univariate analysis, patients with loss of more than 5 kg at diagnosis and admission at diagnosis had a lower rate of colectomy-free survival.
ConclusionsIn our series, colectomy rates are lower than usually reported. Most colectomies were performed in the first 5 years following diagnosis and had an emergency indication.
Conocer la historia natural de la colitis ulcerosa (CU) es esencial para entender la evolución de la enfermedad, evaluar el impacto de las distintas estrategias terapéuticas e identificar factores de mal pronóstico. Uno de los aspectos más relevantes, en este sentido, es la necesidad de cirugía.
ObjetivosAnalizar la Tasa de Incidencia de Colectomía (TIC) desde el diagnóstico hasta el fin de seguimiento (31-12-2017) e identificar factores predictivos de colectomía.
Material y métodosEstudio retrospectivo que incluye los pacientes con diagnóstico definitivo (DD) de CU o Colitis Inclasificable (CI) en la cohorte Navarra 2001−03.
ResultadosIncluimos 174 pacientes con DD de CU (E2 42,8%–E3 26,6%) y 5 de CI: 44,1% mujeres, mediana edad 39,2 años (rango 7–88), mediana de seguimiento 15,7 años. Se intervienen 8 pacientes (TIC 3 colectomías/103pac/a): 3 al debut (<1 mes), 2 en los primeros 2 años, 2 a los 5 años y 1 a los 12 años de evolución. Todos habían recibido esteroides, 5 inmunomoduladores y 2 biológicos. En 7 (87%) la cirugía fue urgente y la indicación, megacolon en 3 (37,5%), brote grave en 3 (37’5%) y fallo a tratamiento médico en 2 (25%). En 5 casos (62,5%) se realizó un reservorio ileoanal y en 3 ileostomía definitiva. En el análisis univariante los pacientes con pérdida >5 kg e ingreso al debut presentaron una menor supervivencia libre de colectomía.
ConclusionesEn nuestra serie, las tasas de colectomía son más bajas que las comunicadas habitualmente, mayoritariamente se realizan en los primeros 5 años de evolución y se indican con carácter urgente.
The concept of inflammatory bowel disease (IBD) encompasses three conditions: ulcerative colitis (UC), Crohn’s disease (CD) and indeterminate colitis (IC). These pathologies, usually diagnosed in youth, have in common the presence of inflammation in the digestive tract and a chronic and recurrent course, alternating periods of marked inflammatory activity with other quiescent periods, in which the patient remains asymptomatic. The impact on quality of life and the consumption of health resources are a constant in the course of these diseases.
We are aware that knowing the natural history of any disease is essential to understand its clinical course, evaluate the impact of the different therapeutic strategies, identify poor prognostic factors, and be able to provide understandable information to patients to help them make decisions.1
In the case of UC, one of the most relevant aspects from the point of view of its natural history is precisely the need for surgery. In this sense, studies based on population cohorts, in which all the patients diagnosed in a well-defined geographical area and in a given period are included, are ideal for drawing conclusions, since they make it possible to obviate the biases of the cohorts of reference centres or of randomised studies in which individuals have to meet some, usually restrictive, inclusion-exclusion criteria.
In 2007, Arin et al. published the results of their study of the incidence of IBD in the Community of Navarra.2 This study included adult and paediatric patients, diagnosed both in public health centres (Hospital de Navarra, Hospital Virgen del Camino, Hospital Reina Sofía and Hospital García Orcoyen) and in private centres (Clínica Universidad de Navarra and Igualatorio Médico Quirúrgico). During the study period (1 January 2001 to 31 December 2003), a total of 288 cases of IBD were diagnosed (176 UC, 102 CD and 10 IC), which represented a crude incidence rate for UC, CD and IC of 10.29, 5.96 and 0.58 cases/100,000 inhabitants/year, respectively.
After more than 15 years since the diagnosis of the first patients included in the study by Arin et al., we set out to analyse the progression of UC in this cohort, in terms of the need for surgery.
Our main objective was to examine the colectomy incidence rate (CIR) in all patients with UC or IC included in this cohort, and followed up to the present day, and as a secondary objective to identify the predictive factors of colectomy.
Material and methodsThis was a retrospective cohort study that included all patients diagnosed with IBD in Navarra in the period between 1 January 2001 and 31 December 2003, whose definitive diagnosis (DD) was that of UC or IC (total cohort of 288 patients).
The initial diagnosis (ID) was considered to be that attributed to each patient in the study by Arin et al.,2 while the DD was established by the research team, based on the Lennard-Jones criteria, once the history of each person had been reviewed. Therefore, it could happen that the ID was maintained, that there was a change in the disease within the IBD itself, or that IBD was ruled out.3
First, a descriptive analysis of the study population was performed, followed by a multivariate analysis. This was carried out using logistic regression, the dependent variable being the colectomies performed throughout the course of the UC. In all cases, the multivariate analysis was adjusted for the different variables collected, always taking into account the severity at diagnosis. The data was examined with the SPSS Statistics 21.0 system.
This study was approved by the Comité Ético de Investigación Clínica de Navarra [Clinical Research Ethics Committee of Navarra] (Pyto 2016/3 of 3-2-2016).
ResultsIn three patients (1%), one diagnosed with UC and two with IC, no data were available during the course of the disease and, therefore, they were considered as lost cases. In 12 people, after analysing the medical records, the research team ruled out the diagnosis of IBD (4% overall). Of these, only in two was the ID of UC (one case) or IC (one case): in both, after reviewing the initial diagnostic tests (endoscopy and histology) and clinical progression, it was considered that the diagnosis of IBD was not consistent and they were interpreted as nonspecific colitis.
The concordance between the ID and the DD was variable depending on the disease (Table 1). In the case of UC, the ID was confirmed in 171 of the 175 initial cases (97.7% concordance), two were finally labelled as CD, one as IC, and in one the diagnosis of IBD was ruled out. In the case of IC, of the eight initial cases, only in four was the diagnosis maintained (50% concordance), three were reassigned to the UC group, and in one case IBD was ruled out.
Concordance between initial and definitive diagnosis.
| Definitive diagnosis | ||||||
|---|---|---|---|---|---|---|
| CD | UC | IC | Not IBD | Total | ||
| Initial diagnosis | CD | 92 (90.2%) | 0 | 0 | 10 (9.8%) | 102 |
| UC | 2 (1.1%) | 171 (97.7%) | 1 (0.6%) | 1 (0.6%) | 175 | |
| IC | 0 | 3 (37.5%) | 4 (50%) | 1 (12.5%) | 8 | |
| Total | 94 (33%) | 174 (61.1%) | 5 (1.8%) | 12 (4.2%) | 285 | |
CD: Crohn's disease; IBD: inflammatory bowel disease; IC: indeterminate colitis; UC: ulcerative colitis.
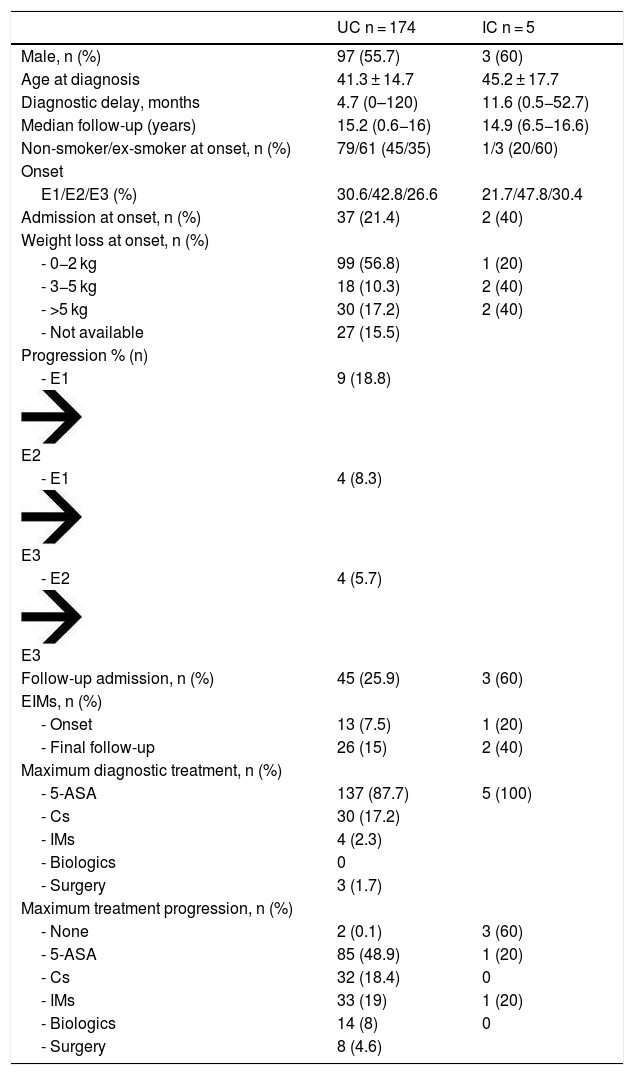
With all this, the final series was of 273 patients, of which 94 (34.4%) corresponded to CD, 174 (63.7%) to UC and five (1.8%) to IC. We analysed the individuals with UC and IC together. The characteristics of the 179 people included are shown in Table 2. The median follow-up was 15.7 years.
Patient characteristics.
| UC n = 174 | IC n = 5 | |
|---|---|---|
| Male, n (%) | 97 (55.7) | 3 (60) |
| Age at diagnosis | 41.3 ± 14.7 | 45.2 ± 17.7 |
| Diagnostic delay, months | 4.7 (0–120) | 11.6 (0.5−52.7) |
| Median follow-up (years) | 15.2 (0.6−16) | 14.9 (6.5−16.6) |
| Non-smoker/ex-smoker at onset, n (%) | 79/61 (45/35) | 1/3 (20/60) |
| Onset | ||
| E1/E2/E3 (%) | 30.6/42.8/26.6 | 21.7/47.8/30.4 |
| Admission at onset, n (%) | 37 (21.4) | 2 (40) |
| Weight loss at onset, n (%) | ||
| - 0−2 kg | 99 (56.8) | 1 (20) |
| - 3−5 kg | 18 (10.3) | 2 (40) |
| - >5 kg | 30 (17.2) | 2 (40) |
| - Not available | 27 (15.5) | |
| Progression % (n) | ||
| - E1E2 | 9 (18.8) | |
| - E1E3 | 4 (8.3) | |
| - E2E3 | 4 (5.7) | |
| Follow-up admission, n (%) | 45 (25.9) | 3 (60) |
| EIMs, n (%) | ||
| - Onset | 13 (7.5) | 1 (20) |
| - Final follow-up | 26 (15) | 2 (40) |
| Maximum diagnostic treatment, n (%) | ||
| - 5-ASA | 137 (87.7) | 5 (100) |
| - Cs | 30 (17.2) | |
| - IMs | 4 (2.3) | |
| - Biologics | 0 | |
| - Surgery | 3 (1.7) | |
| Maximum treatment progression, n (%) | ||
| - None | 2 (0.1) | 3 (60) |
| - 5-ASA | 85 (48.9) | 1 (20) |
| - Cs | 32 (18.4) | 0 |
| - IMs | 33 (19) | 1 (20) |
| - Biologics | 14 (8) | 0 |
| - Surgery | 8 (4.6) |
Cs: corticosteroids; IMs: immunomodulators; EIMs: extraintestinal manifestations; 5-ASA: 5-aminosalicylic acid.
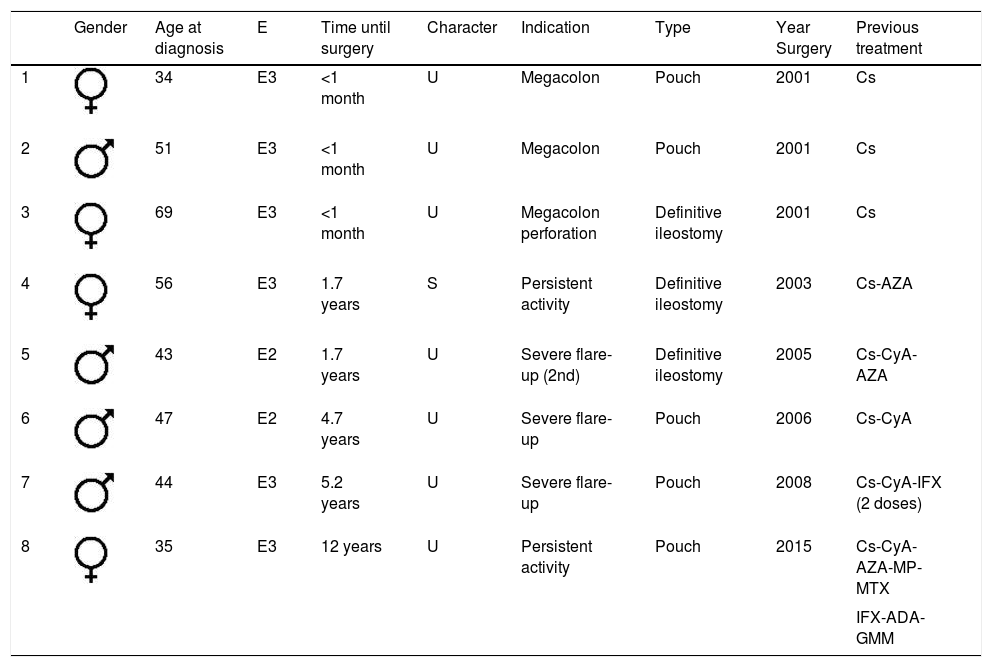
At the end of the follow-up, eight patients underwent surgery (Table 3), which represents a crude colectomy rate of 4.4% and an incidence rate of three colectomies/103patients/year (Fig. 1).
Characteristics of colectomy patients.
| Gender | Age at diagnosis | E | Time until surgery | Character | Indication | Type | Year Surgery | Previous treatment | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 34 | E3 | <1 month | U | Megacolon | Pouch | 2001 | Cs | |
| 2 | 51 | E3 | <1 month | U | Megacolon | Pouch | 2001 | Cs | |
| 3 | 69 | E3 | <1 month | U | Megacolon perforation | Definitive ileostomy | 2001 | Cs | |
| 4 | 56 | E3 | 1.7 years | S | Persistent activity | Definitive ileostomy | 2003 | Cs-AZA | |
| 5 | 43 | E2 | 1.7 years | U | Severe flare-up (2nd) | Definitive ileostomy | 2005 | Cs-CyA-AZA | |
| 6 | 47 | E2 | 4.7 years | U | Severe flare-up | Pouch | 2006 | Cs-CyA | |
| 7 | 44 | E3 | 5.2 years | U | Severe flare-up | Pouch | 2008 | Cs-CyA-IFX (2 doses) | |
| 8 | 35 | E3 | 12 years | U | Persistent activity | Pouch | 2015 | Cs-CyA-AZA-MP-MTX | |
| IFX-ADA-GMM |
ADA: adalimumab; AZA: azathioprine; Cs: corticosteroids; CyA: cyclosporin C; GMM: golimumab; IFX: infliximab; MP: mercaptopurine; MTX: methotrexate; S: scheduled; U: urgent.
Three patients underwent surgery very early, in the first month after diagnosis, two in the first two years, two at five years and one after 12 years with the disease. All had received steroids, five (62.5%) of them had also been treated with immunomodulators (IMs) (cyclosporine [CyA] in four cases) and in two (25%) biological drugs were indicated against tumor necrosis factor (anti-TNF) before surgery. In all cases, CyA was administered intravenously for a median of 9.5 days (6–12) and was prolonged orally for a further seven days in only one patient. In two people, it was ineffective and the patients underwent a colectomy, one directly and the other one month and a half later, after receiving two doses of infliximab without obtaining any response. The remaining two individuals required surgery later, one at 12 months and the other at six years: both had continued with thiopurines after the administration of CyA. Additionally, it should be noted that another three patients in our series received CyA for the same reason, with good control of the flare-up, without requiring subsequent surgery.
In seven cases (87%), the surgery was urgent and only in one case, with persistent moderate activity, was it scheduled normally. The indication was megacolon in three patients (37.5%), severe flare-up in another three (37.5%) and failure of medical treatment in the remaining two cases (25%). Ileoanal pouch surgery was performed in five people (62.5%) and a definitive ileostomy in three.
None of the patients diagnosed in paediatric age, that is, before the age of 15 (n = 5), required surgery.
In the univariate analysis, patients with weight loss >5 kg at diagnosis and admission at the onset of the disease had a lower colectomy-free survival (P = .005) (Fig. 2).
In the multivariate analysis, no predictor of colectomy was identified.
DiscussionOur series confirms what had already been verified over recent decades, which is that there has been a decrease in the rates of colectomy in patients with UC. This may be related to earlier diagnosis of the disease, the incorporation of guidelines into clinical practice that help to make quick decisions or improve surveillance strategies, and reducing the indication for colectomy due to dysplasia or colorectal cancer. But, above all, it seems to go hand in hand with the great advances in the field of medical treatment.4 Derivatives of 5-aminosalicylic acid (5-ASA), steroids,5 CyA and thiopurines6 have been progressively added over the last few decades to the therapeutic arsenal available for this pathology. But, without a doubt, the fundamental therapeutic change in the management of IBD as a whole has been the appearance of biological drugs, fully incorporated into clinical practice since the beginning of the 21st century.7 The first biologic authorised for IBD was infliximab: the European Medicines Agency (EMA) accepted its use in patients with CD in 1999, and in those with UC in 2005. The appearance of these drugs has had such an important impact on the management of IBD that it has even marked a new era: the biologic era. In the case of UC, 2005 marked the start of the biologic era1 It is suggested that the appearance of biologics has been key in explaining the decrease in the rates of surgery in UC.8
The population series published in the pre-biologic era are those that include longer follow-ups, even longer than 20 years, and higher colectomy rates.
Leijonmarck et al.9 analysed, in a population cohort from the Stockholm region, the data of 1586 patients diagnosed with UC between 1955 and 1984, and followed up for a median of 13 years. In this series, the cumulative colectomy rates at 5, 10 and 25 years were, respectively, 20% (CI 18%–22%), 28% (CI 26%–30%) and 45% (CI 41%–49%). Of the total number of surgeries, 10% were performed in the first year after diagnosis and 60% in the first five years of the disease, the only predictor of surgery being extensive disease at the time of diagnosis.
A similar study was carried out in Copenhagen,10 which included 1161 patients diagnosed with UC between 1962 and 1987. The crude colectomy rate in this study was 20%, while the cumulative rates at one, five, 10, 15, and 25 years, respectively, were 9%, 20%, 23%, 29% and 32%. Again, extensive disease at diagnosis was identified as a risk factor for colectomy.
But, undoubtedly, one of the cohorts that has contributed the most to the knowledge of the natural history of IBD is the IBSEN cohort.11–13 In this, all the cases of IBD in four regions of southeastern Norway (Oslo, Østfold, Telemark and Aust-Agder), diagnosed in the period between 1 January 1990 and 31 December 1993, were collected and prospectively followed up. The rates of colectomy at five years were 7.5% (71% in the first two years) and 9.8% at 10 years. Extensive disease, age <40 years, need for steroids or C-reactive protein >30 mg/dl, all at onset of the disease, were identified as risk factors for colectomy.
Samuel et al.14 published data on the 369 patients with UC diagnosed in the Olmsted region (Minnesota) between 1970 and 2004. The colectomy rates in this cohort were 13.1% at five years (95% CI, 9.4%–16.6%), 18.9% at 10 years (14.4%–23.2%) and 25.4% at 20 years after diagnosis (19.8%–30.8%). Male gender (HR, 2.1; 95% CI, 1.3–3.5), diagnosis in the 1990s (HR, 2.0, 1.01–4.0) and diagnosis between the years 2000–2004 (HR, 3.7; 1.7–8.2) were significantly associated with the risk of colectomy.
In a meta-analysis published in 2013,4 in which data from 30 population studies was included (26 in manuscript form and four as abstracts), a risk of surgery was established in patients with UC, one, five and 10 years after diagnosis of 4.9%, 11.6% and 15.6%, respectively.
In 2018, Fumery et al.1 reviewed the natural history of UC in 17 population cohorts, concluding that the risk of colectomy at five and 10 years, respectively, was 10%–15%. Of the patients included in their review, 20% had required IMs and up to 10% anti-TNF drugs for disease control. It should be noted that, in this review, the same authors describe very important differences between the cohorts in specific aspects such as hospitalisations or colectomies.
It is likely that this type of systematic review, in which pre-biologic and biologic population cohorts are jointly analysed, which include patients from diverse geographic areas, with years of inclusion and very different follow-up periods, are not the most appropriate for determining what is the real progression of UC at this time.
Obviously, there are fewer series that include exclusively patients diagnosed in the biologic era and these have shorter follow-up, but perhaps they are the ones that allow a more realistic picture of the current progression of UC.
Niewiadomski et al. prospectively collected 96 patients diagnosed with UC in the Barwon area (Victoria-Australia) in the periods 2007 to 2008 and 2010 to 2013.15 The mean follow-up was 18 months (12–82) and the colectomy rates, one and five years after diagnosis, were 2% and 13%, respectively. In these, 32% required IMs and 10% biologics.
The Epi-IBD study included, also prospectively, 717 patients diagnosed with UC in 22 European countries and Israel throughout 2010.16 The mean follow-up was 63 months (44–63) and the overall rate of surgery at the end of follow-up was 6% (67% of these in the first two years after diagnosis). It is noteworthy that, when data from Western hospitals were analysed, only 2% had required colectomy after two years. In this series, 30% received IMs and 12% biologics.
The EpiCom cohort, in 2011, included 380 patients with UC and 71 with IC.17 At the end of the first year of follow-up, one patient with UC (0.3%) and two with IC (3%) had required surgery, while 5% received biological drugs.
Jeuring et al. analysed the colectomy rate among patients with UC diagnosed in the Limburg area (Netherlands) in three different cohorts (cohort A: 1991–1997, cohort B: 1998–2005, and cohort C: 2006–2010).18 In the first year, the cumulative colectomy rate was 4.1%, 0.9% and 1%, respectively, in each of the cohorts, and at five years it was 7.5%, 5.7% and 4.1%. The percentage of patients, for each of the cohorts, who required IMs was 12, 26% and 22%, and for biological drugs it was 0%, 4.4% and 10.6%.
More recently, Barnes et al. published a retrospective study carried out in the USA on the IQVIA Legacy PharMetrics Adjudocated Claims Database (IQVIA).19 This database includes 93,930 patients with UC (18–65 years): in 2007 the colectomy rate was 7.8 cases/103 patients/year (95% CI, 7.4–8.2) and in 2016 it was 4.2 cases/103 patients/year (95% CI, 3.2–5.1). As in the rest of the studies, the decrease in colectomy rates was accompanied by an increase in the use of biologics.
It seems clear that, since the advent of biological drugs, colectomy rates in patients with UC have been progressively decreasing. If we limit ourselves to series that include patients diagnosed closer to the biologic era, ours is one of those that provides a longer follow-up (15.7 years) and a lower colectomy rate (crude colectomy rate 4.4%; cumulative incidence rate of colectomy of three colectomies/103 patients/year). It is true that, from the point of view of UC, ours should perhaps be considered a “transition” series between the pre-biologic and biologic eras since, until 2005, we did not have the possibility of using infliximab in people with UC. In fact, 50% of our patients underwent surgery when the drug for this pathology was not yet authorised, which is a limitation of our study.
As in other series, most of the patients operated on (75%) had extensive colitis (Montreal E3) and 75% had surgery in the first five years after diagnosis.
In the univariate analysis, weight loss (reported by the patient) greater than 5 kg at diagnosis, and the fact of being admitted at the time of onset of the disease, turned out to be the only predictive factors of colectomy, while in the multivariate analysis none was identified. Male gender, active smoking, the extent of the disease or the need for corticosteroids, identified as risk factors for colectomy in other series, were not statistically significant in ours.20 This analysis is probably influenced by the small number of colectomy patients.
Obviously, all this occurs at the expense of an increase in the use of immunosuppressive drugs, both IMs and biologics. In our series, at the end of the follow-up, 19.6% of the patients received IMs and 8.3% biologics, both percentages lower than those described in the most recent series, and this may perhaps reflect the greater experience we have acquired in the management of these drugs that, today, we are probably indicating earlier in the course of the disease.
In our series, the colectomy rate was very low and we will just have to wait and see if this data is confirmed in subsequent studies. Series such as the Spanish one that is collecting incident cases diagnosed in the year 201721 or the Norwegian IBSEN III,22 which will include all the cases diagnosed in the IBSEN territory between 2017 and 2019, are likely to provide part of the answers. And then, when we really check what is changing in the progression of UC, we will be able to have reliable and updated information to share with managers and patients, which will allow us to adapt the system to the real needs of the disease and help both professionals and patients in making decisions.
FundingThe authors declare that they received no funding to conduct this study.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodríguez C, Elosua A, Prieto C, Pérez E, Irisarri R, Campillo A, et al. Tasas de colectomía en colitis ulcerosa 15 años después del diagnóstico. Datos de la cohorte Navarra 2001–2003. Gastroenterol Hepatol. 2022;45:1–8.