Cytomegalovirus (CMV) is a very common viral pathogen with significant morbidity and mortality in immunosuppressed patients.
We present the case of a 72-year-old woman, with a history of polymyalgia rheumatica undergoing chronic treatment with methotrexate (20mg/week) and methylprednisolone 5mg. She presented a one-month history of epigastric pain and postprandial fullness and a five-month history of constitutional symptoms. She reported no drug exposure. The gastroscopy revealed focal antral gastritis and a fibrin-coated ulcer in the lesser curvature, without identifying Helicobacter pylori. The gastroscopy revealed focal antral gastritis and a fibrin-coated ulcer in the lesser curvature measuring 10–12mm, with regular and oedematous folds. The pathology study revealed an ulcer with chronic gastritis with an interstitial inflammatory component and adjacent foveolar hyperplasia, without identifying Helicobacter pylori.
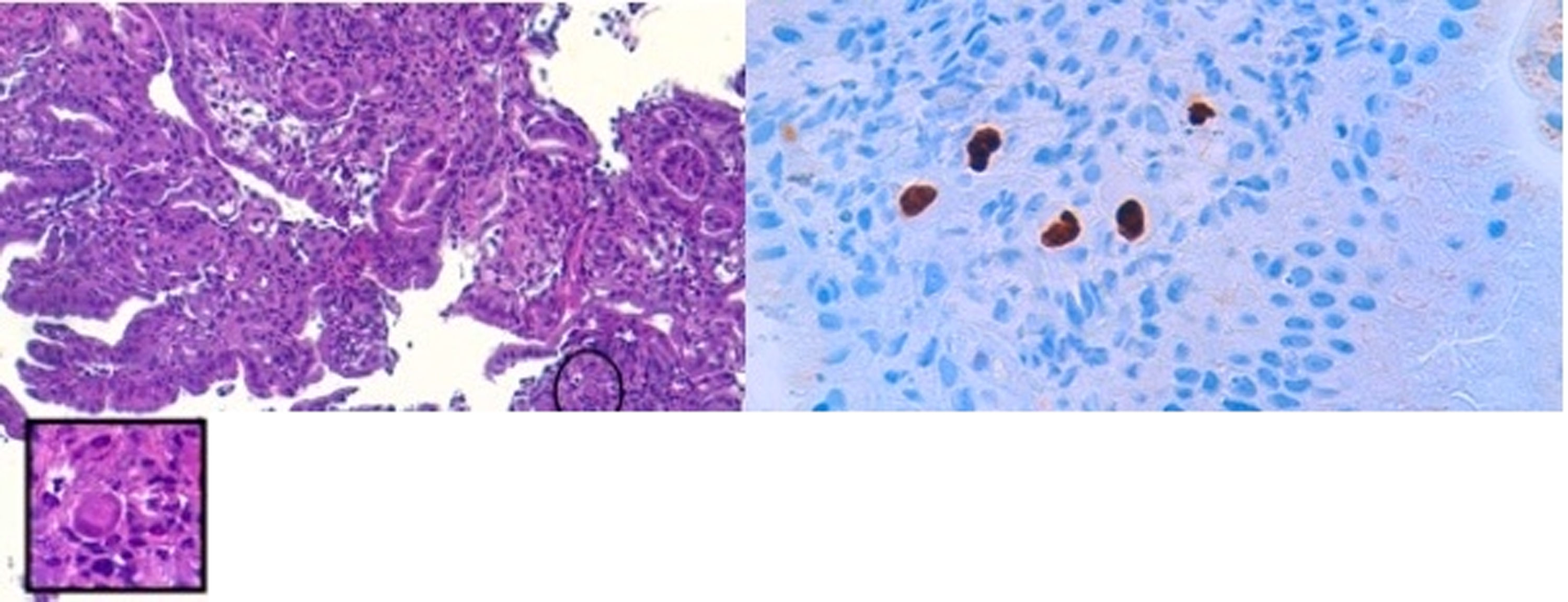
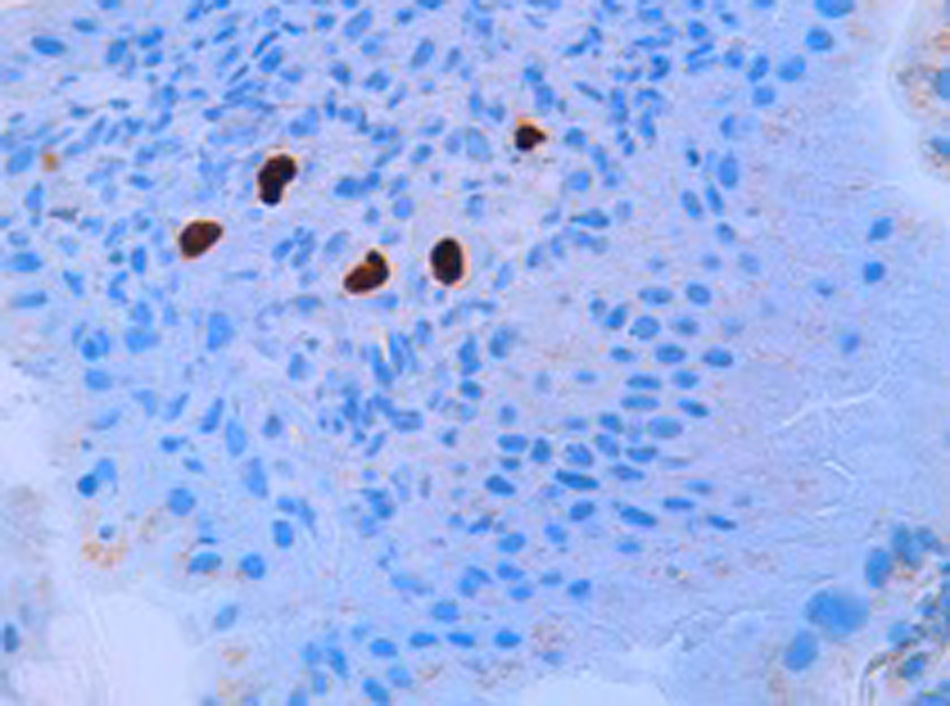
Treatment was started with esomeprazole 40mg/12h for six weeks resulting in clinical improvement, with food intolerance due to vomiting, anorexia, polymyalgia and severe asthenia. The blood tests identified hypoproteinaemia (4.8g/dl), hypoalbuminaemia (2.53g/dl) and macrocytic anaemia (haemoglobin 98g/l). The second gastroscopy revealed three fibrin-coated ulcers measuring 1cm in diameter, with geographic borders and with perilesional oedema. The pathology study showed CMV-associated gastritis with ulceration and the immunohistochemical study was positive (Figs. 1 and 2).
(A and B) Associated changes at the border of the ulcer, with marked foveolar hyperplasia, reactive epithelial abnormalities and chronic and acute non-specific inflammation. Focally, large stromal or endothelial cells with nuclear and cytoplasmic inclusions characteristic of CMV infection can be seen.
Methotrexate was suspended and intravenous ganciclovir administered (5mg/kg/day) for four weeks followed by oral valganciclovir. Follow-up gastroscopies were performed, revealing progressive improvement. However, the patient suffered a flare-up of her rheumatic disease and treatment was started with leflunomide and methylprednisolone 5mg/day. At this time it was decided to maintain permanent secondary prophylaxis with oral valganciclovir (450mg/day).
CMV is a highly seroprevalent herpes virus in the adult population. However, not all infected patients develop clinical symptoms. In immunosuppressed patients, its severity is directly related to the degree of immunosuppression. Its manifestations range from fever to organ involvement.1 Very few cases of rheumatology patients receiving immunomodulators or biological medicinal products have been published in the literature. Infectious oesophagitis is probably the most common symptom, followed by colitis. A meta-analysis published in the Revista Clínica de Reumatología [Clinical Journal of Rheumatology] in 2013 found that stomach ulcers are extremely rare and are characterised by a wide variety of symptoms. In contrast, another review of case studies published in the same journal found ulcers of the upper gastrointestinal tract to be to most common symptom, with multiple ulcers found in 55% of patients, typically in the gastric antrum. Although a lack of mortality in this group of patients is a noteworthy finding, serious life-limiting manifestations secondary to the onset of hypovolaemic shock can occur. The risk of contracting the disease seems to be associated with significant weight loss and combinations with corticosteroids or immunosuppressants like cyclophosphamide and methotrexate. In these patients, the onset of CMV-associated disease may occur several months or even years after starting immunosuppressive therapy.2
Macroscopically, CMV-induced gastric ulcers may look extremely similar to those caused by Helicobacter pylori or by NSAIDs. Deep biopsies must be taken as CMV can sometimes be found in the submucosal tissue. Diagnosis is confirmed by identifying intranuclear inclusion bodies in the haematoxylin and eosin stain. However, the sensitivity of this test is low, which is why immunohistochemistry is recommended if CMV is suspected.3 It may be useful to administer a PPI to promote healing in immunocompetent hosts. However, immunosuppressed patients require the concomitant administration of an antiviral agent like ganciclovir. According to the literature, the most widely-used regimen is intravenous ganciclovir administered for three or four weeks, while foscarnet is an effective alternative. We only found one case of relapse in the form of a gastric ulcer in the published literature, which occurred 20 days after initiating the treatment. Some authors recommend a shorter intravenous therapy regimen followed by oral treatment with valganciclovir.4
There are no published data concerning primary prophylaxis in patients receiving immunomodulators or biological medicinal products. They should probably be considered low risk practically for life. Nevertheless, given the low estimated incidence, indefinite monitoring could be a questionable strategy. In the event of the onset of disease, it is recommended to adjust the immunosuppressive therapy if possible and maintain prophylaxis with oral valganciclovir over the long term, probably indefinitely, depending on the degree of immunosuppression, as disease relapse is common. It would be interesting to know the potential effects of changing immunosuppressive therapy to leflunomide in rheumatology patients given that this drug is active against CMV if administered orally and is inexpensive.2 The successful use of leflunomide as an alternative in transplant patients (kidney and lung) resistant to ganciclovir and in secondary prophylaxis has been reported, primarily in cases of low viral load and without severe disease. However, cases of leflunomide failure in haematopoietic cell transplantation have also been published, meaning that the results found in the literature are open to debate.
Please cite this article as: Martínez Huguet C, Arguedas Lázaro Y, del Valle Sánchez E, Omiste Sanvicente T, Bernal Monterde V, Montoro Huguet M. Citomegalovirus asociado a úlcera gástrica: caso clínico y revisión de la literatura. Gastroenterol Hepatol. 2019;42:256–258.