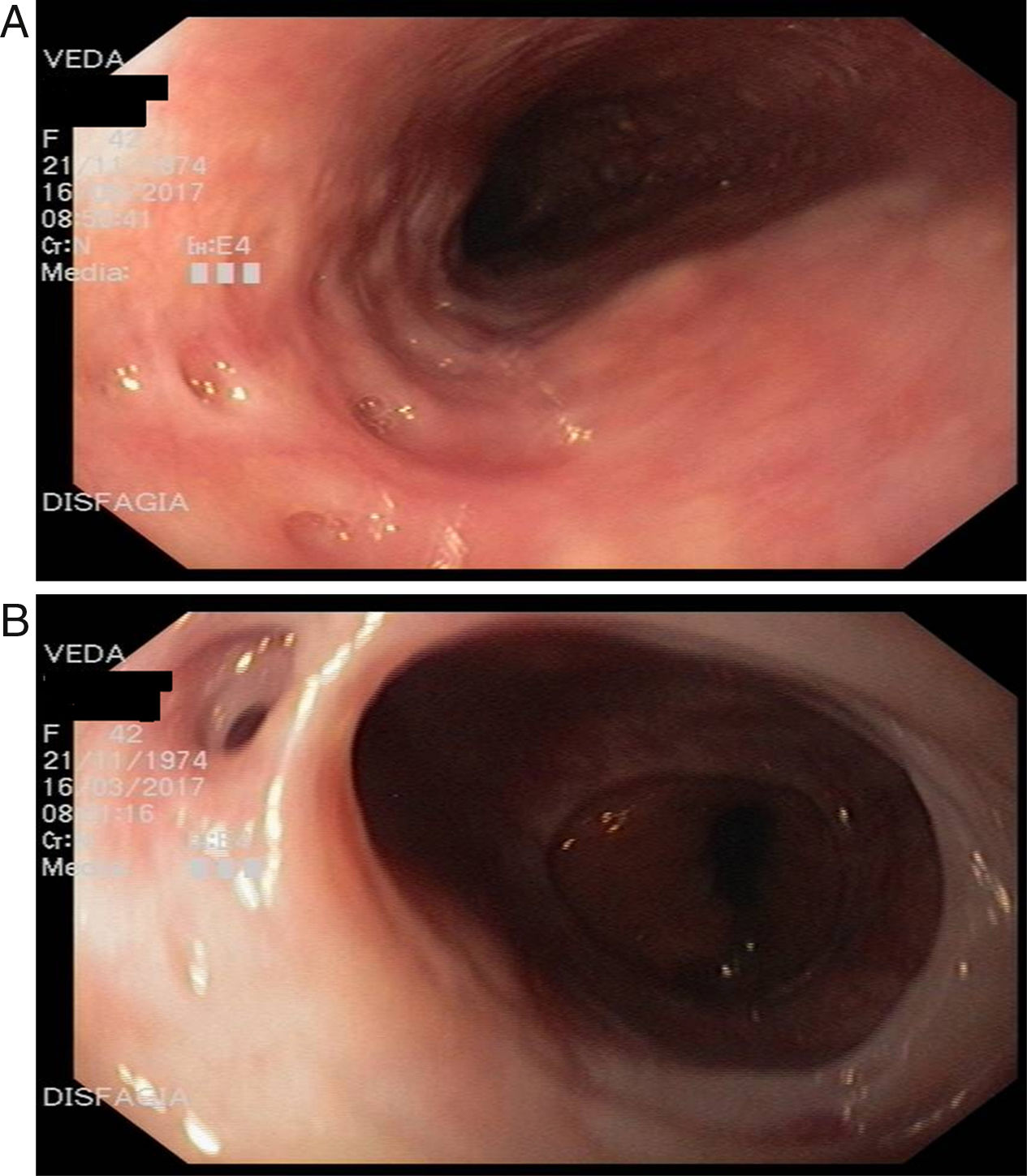
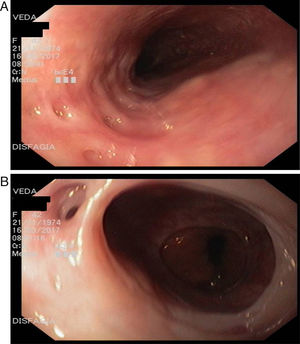
We present the case of a 42-year-old female patient, who was referred to our department with a five-year history of progressively worsening oesophageal solid-food dysphagia. She reported repeated episodes of food impaction, which passed spontaneously without the need for extraction by endoscopy. Her previous medical history included HIV for 10 years, for which she partially adhered to treatment, an episode of oesophageal candidiasis three years prior to the consultation for which she received antifungal treatment which partially improved the symptoms, alcohol consumption of 200g/day for 10 years and smoking. An upper GI video-endoscopy was performed which showed sectors with dilated lumen and other narrow sectors, with no food content. Multiple small holes were found, 2–4mm in diameter, of different depths, with signs that the mucosa was indurated (Fig. 1). Multiple biopsies were taken with nonspecific results, but eosinophilic oesophagitis was ruled out. Treatment was started with proton pump inhibitors with improvement in the dysphagia at 24h. The patient was discharged from hospital and followed up by infectious diseases and gastroenterology.
Oesophageal intramural pseudodiverticulosis is a rare benign disease, initially described by Mendel in 1960.1 In retrospective radiological studies, the condition was found in 0.15% of the oesophageal images.2 There are just over 250 published cases, with a slight predominance in males over the age of 50. It consists of small sac-like invaginations in the oesophageal wall with segmental (predominantly proximal) or diffuse involvement.3 The pathogenesis is unknown, but it is thought to be the result of obstruction of lumen due to inflammation of the submucosal glands or fibrosis of the oesophageal wall. The condition has been associated with reflux disease, diabetes, oesophageal candidiasis, achalasia, Mallory Weiss tears, alcohol consumption and smoking.4 The predominant symptom, found in up to 80% of patients, is oesophageal dysphagia, and food impaction can sometimes occur. However, it can also be asymptomatic. Oesophageal barium swallow is a more sensitive diagnostic method, in which narrow orifices and small invaginations can be detected in the oesophageal wall continuous with the lumen. These lesions are only detected by gastroscopy in 20% of cases.5,6 Computed tomography images show a diffuse thickening of the oesophageal wall which can simulate intramural gas, and irregularities in the lumen of the organ. In most cases, histological diagnosis is only possible from surgical specimens, in which dilation of the excretory ducts of the submucosal glands can be detected. The histology report from endoscopic biopsies usually lists nonspecific oesophagitis. As in our patient, Candida infection is recognised in a high percentage of cases, but whether it plays an aetiological role or is incidental is unknown and, if diagnosed, it should be treated, as it improves the symptoms.7 The main complication is stenosis, which is reported in up to 80–90% of cases, but dysphagia occurs regardless of this finding. Some authors have described a higher prevalence of oesophageal cancer in this disease. However, there is no evidence in the literature to support it being a premalignant condition. Other complications such as oesophageal fistula or perforation are rare. Treatment consists of measures to control reflux disease, abstaining from alcohol and antibiotic therapy for associated infections. In patients with stenosis, endoscopic dilation has been reported to improve symptoms, but surgery is occasionally necessary.8 In the long-term, despite clinical improvement and adequate treatment, there is no regression of the pseudodiverticulosis.
Please cite this article as: Biagioni M, Olmos JI, Antelo P, Waldbaum C, Wonaga A, Sordá J. Disfagia por seudodiverticulosis esofágica intramural: inusual hallazgo endoscópico. Gastroenterol Hepatol. 2018;41:506–507.