Ingestion of foreign bodies (FB) is a common reason for urgent gastrointestinal endoscopy. More than 80% of the FB that reach the stomach will pass through the gastrointestinal tract until they are expelled. Large FB, however, can remain lodged in the gastric cavity. Nonetheless, less than 1% will cause serious complications, such as perforation of the gastric wall, or reach adjacent organs such as the pancreas.1 We present a case of resolution of this serious complication by gastrointestinal endoscopy.
Our patient was a 60-year-old male with a history of coronary heart disease and hypertension who came into the emergency department on two separate occasions with epigastric and retrosternal pain. In the second assessment, a week after the initial onset, the pain had progressively increased in intensity, with associated pyrexia of 38°C during the previous two days. On physical examination, the patient had diffuse pain in the upper abdomen without signs of peritoneal irritation. Blood tests only showed leucocytes 11.9×103/mm3 (75.1% PMN) and raised CRP (94.23mg/l) with complete blood count and liver profiles, amylase and lipase, within the normal laboratory range.
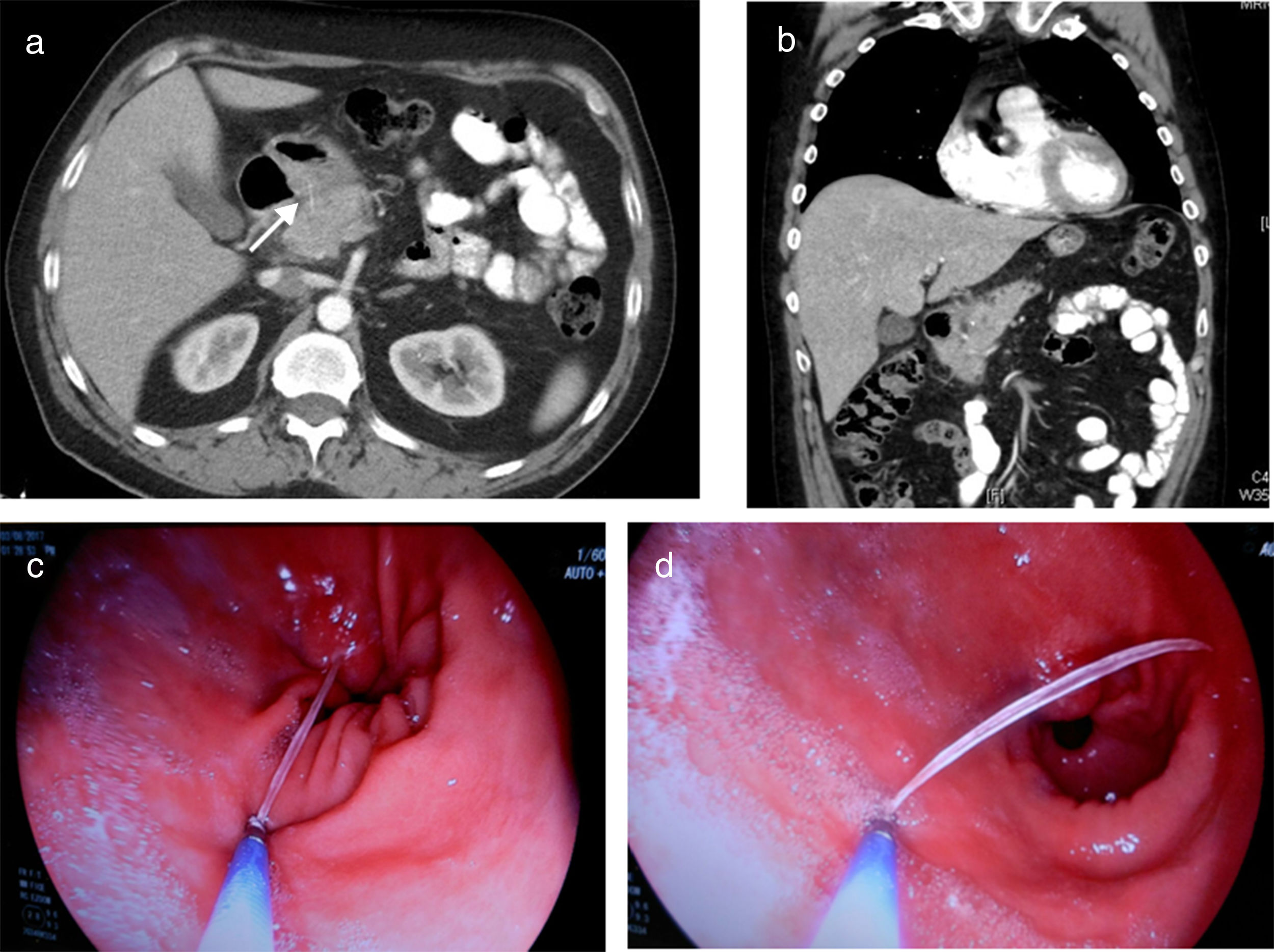
Computed tomography (CT) scan of thorax/abdomen showed inflammatory changes in the peripancreatic fat, and in the adjacent gastric antrum, pylorus and duodenal bulb. A linear image of at least 3cm was observed which, from the lumen of the antrum, was pointing towards the head of pancreas, with thickening of both structures (Fig. 1a and b). Performing gastroscopy we found an area of oedematous mucosa with fibrin at the roof of the pyloric antrum. Washing of the area revealed the tip of a trapped fish bone, which we were able to extract with forceps without incident (Fig. 1c and d).
(a and b) Images from the thorax/abdomen CT scan showing frayed edges and increased peripancreatic fat density, and of the adjacent gastric antrum, pyloric region and duodenal bulb, with linear image (arrow) of at least 3cm from the lumen of the antrum to the head of pancreas, with thickening of both structures; (c and d) gastroscopy images of the extraction of the fish bone with forceps.
After extraction of the FB, the patient made good clinical progress, initially nil by mouth with IV antibiotic therapy, later tolerating oral diet, and was discharged from hospital after five days. At his outpatient follow-up two weeks later, the patient was asymptomatic. At four weeks, repeat CT and gastroscopy showed complete recovery.
Sharp or pointed FB can penetrate the wall of the gastrointestinal tract and even migrate to adjacent organs. The most common are toothpicks and fish and chicken bones. They are very often ingested accidentally, without the affected person even being aware, as in our case. The most likely areas for an FB to become impacted or cause perforation are where there is physiological narrowing of the gastrointestinal tract, such as the pyloric region, duodenal curves, the angle of Treitz or ileocaecal valve.2 The associated complications range from complete lodging in the gastric wall, which could be mimicking subepithelial tumours or pseudo-pancreatic tumours with or without biliary obstruction, to liver abscesses.3–5
Initial diagnosis is mainly made by imaging techniques. However, there needs to be a high diagnostic suspicion, given that the signs may be hidden and it may not always present with symptoms of persistent and progressive abdominal pain, even presenting with fever. The test of choice is CT, thanks to the different reconstructions that can be performed in different planes. In a large proportion of cases, CT can assess the complication and detect the FB as a radiopaque image in the area showing radiological signs of inflammation or complication.5
Treatment has classically been surgery, but an increasing number of cases are being published of endoscopic management, with this being simple, fast and without complications in the majority of cases.2 For FB which have penetrated deeply and are not visible from the gastrointestinal lumen, there are reports of using endoscopic ultrasound techniques to help detect them and then extracting them by submucosal dissection.3,4 In our case, the FB was embedded in the gastric wall, although ulceration was still visible proximal to where it had penetrated and we were able to grab it by its proximal tip and extract it with biopsy forceps. The patient's rapid clinical improvement after the FB was extracted was impressive, in line with other reports in the literature.4,5
In conclusion, when a sharp or pointed FB penetrating or perforating the gastrointestinal system is diagnosed, in view of its less aggressive nature and high likelihood of resolution, we should opt for gastrointestinal endoscopy before resorting to surgery.
Please cite this article as: Núñez Martínez Ó, Sanz García C, Pérez Enciso I, Holguera Ortiz L, Alberdi Alonso JM. Resolución endoscópica de perforación gástrica con penetración a páncreas por espina de pescado. Gastroenterol Hepatol. 2018;41:567–568.