Until the introduction of penicillin in the mid-twentieth century syphilis, caused by the bacterium Treponema pallidum, was one of the most common sexually transmitted infections. The incidence of syphilis decreased significantly following the discovery and subsequent introduction of penicillin, but has begun to increase over the last decade, mainly in the context of HIV. In Chile, in the first quarter of 2016, 846 cases were reported to the Ministry of Health, with an incidence rate of 4.6 per 100,000 population.1
T. pallidum has a similar pathogenesis to Mycobacterium tuberculosis, the pathogen responsible for tuberculosis. Both agents have in common a slow replication time, often asymptomatic primary infection, and silent dissemination which can lead to multi-organ failure.
Syphilis is classically described as having three phases: (a) primary phase in which local multiplication occurs; (b) secondary phase with lymphatic and haematogenous dissemination and skin, eye, central nervous system (up to 40% of cases) involvement observed in the patient, and (c) tertiary phase, mediated by hypersensitivity, which can manifest up to 30 years after infection, and among other problems, can involve bones and central nervous and cardiovascular systems.2
We present the case of a 68-year-old male patient with a history of hypertension who consulted for a week-long history of colic-type abdominal pain in the epigastrium radiating to both hypochondria.
On physical examination, the patient was alert and orientated, haemodynamically stable, afebrile and eupnoeic. Examination of the patient's skin revealed confluent macular exanthema, predominantly on the trunk. Cardiopulmonary examination was normal. His abdomen was soft and depressible, but sensitive to palpation in the epigastrium. There were no signs of peritoneal irritation.
Laboratory tests showed haemoglobin 17.7g/dl, leucocytes 13,470, 316,000 platelets/μl, ESR 13mm/h, CRP 15mg/l, lipase 42U/l, creatinine 0.9mg/dl and normal liver profile, and abdominal ultrasound was normal.
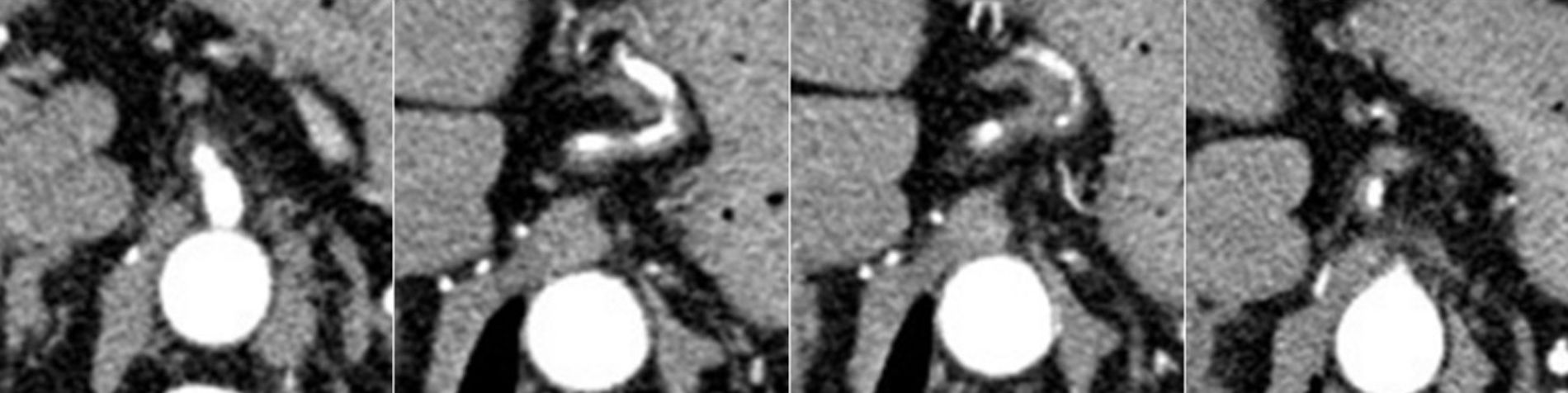
As the abdominal pain continued to persist, even with high doses of opioids, a computed tomography (CT) angiography study was performed. The CT showed diffuse wall thickening of the left gastric artery with an area of multi-segmental stenosis, with no abnormalities in renal and coeliac arteries (Fig. 1).
An increase in macular lesions and palmoplantar involvement were also detected, as a result of which a Venereal Disease Research Laboratory (VDRL) test was requested, showing titres of 1:16. Other results included: HIV negative; FTA-ABS positive 1:32; study with ANA, ANCA, ENA autoantibodies negative; serology for HBV and HCV negative; cytology study in cerebrospinal fluid detected presence of 8–10 predominant mononuclear and physicochemical cells showing proteins of 95mg/dl and normal glucose, with VDRL 1:8.
Magnetic resonance imaging (MRI) of the brain detected leptomeningeal meningovascular involvement compatible with neurosyphilis. Although the skin and laboratory findings pointed to secondary syphilis, the typical characteristics of tertiary syphilis with neurological and vascular involvement predominated and aggravated the condition. The patient was started on treatment with intravenous sodium penicillin for 14 days, with which the skin lesions cleared up and the abdominal pain gradually decreased and went away. Repeat CT-angiogram of the abdomen and pelvis showed regression of the vascular involvement.
Although there was clinical improvement in symptoms over the course of the patient's stay in hospital, he developed areflexic paraparesis of the lower extremities, symptoms compatible with tabes dorsalis. MRI of the medulla oblongata showed a dorsal medullary lesion without contrast enhancement, compatible with vascular damage secondary to neurosyphilis. Motor rehabilitation was initiated and, after significant improvement in the neurological deficit, the patient was discharged.
In a patient with abdominal pain and positive treponemal tests, the following alternative diagnoses should be considered: syphilitic hypertrophic gastritis,2 of similar presentation according to the systematic review by Mylona3; also, painful intra-abdominal lymph nodes, sensitive hepatosplenomegaly, proctitis, pyloric obstruction and secondary vasculitis.4,5 In our patient, the abdominal pain was attributable to T. pallidum infection-mediated vascular involvement.
In syphilis-related vascular involvement, early invasion of the endothelium by spirochetes has been described, particularly in the vasa vasorum, through a mucopolysaccharidase which causes endarteritis obliterans.
The weakened arterial wall can develop mycotic aneurysms with a higher risk of rupture, although nowadays this is a rare complication. Vascular involvement commonly occurs in the aortic arch, but in 10%–20% of cases can affect the abdominal descending aorta and its branches.6,7 There are no pathognomonic images and investigation is based essentially around treponemal serology and positron emission tomography findings which, added to the clinical suspicion and after reasonably ruling out other causes of secondary vasculitis, lead us to the diagnosis.
If vascular involvement alone is being investigated, segmental arterial mediolysis (SAM)7 and vasculitis secondary to other infections, mainly mycobacteria, should be considered as possible diagnoses.
SAM, which has been reported in adults, pregnant women in particular, is a non-arteriosclerotic or inflammatory alteration of unknown cause. The pathogenesis is ischaemia resulting from arterial spasm, affecting the visceral and coronary arteries. Radiologically it can be confused with polyarteritis nodosa, as the angiographic characteristics are similar, with microaneurysms appearing to be strung like the beads of a rosary.
Finally, syphilis is a disease that has increased in incidence over recent years and which should be suspected in the presence of difficult-to-manage abdominal pain and vascular involvement demonstrated by imaging techniques.
Please cite this article as: Navea C, von Mühlenbrock C, Cabello N, Echeverría M, Jiménez A, Poniachik J. Sífilis, causa poco habitual de dolor abdominal. Gastroenterol Hepatol. 2018;41:565–566.