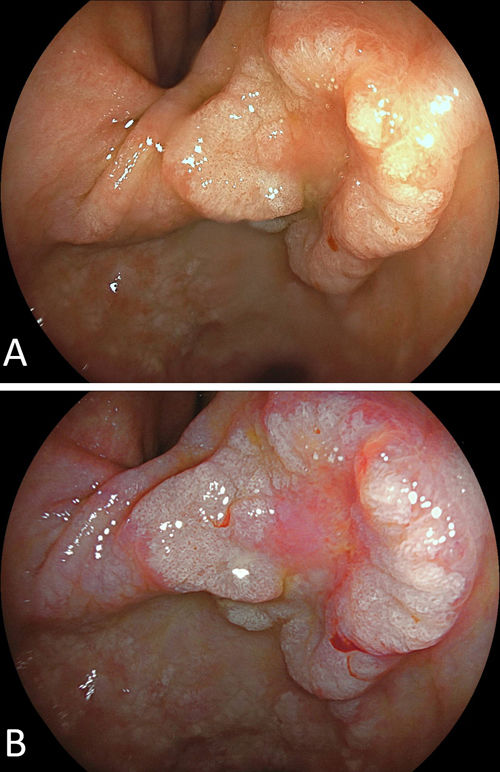
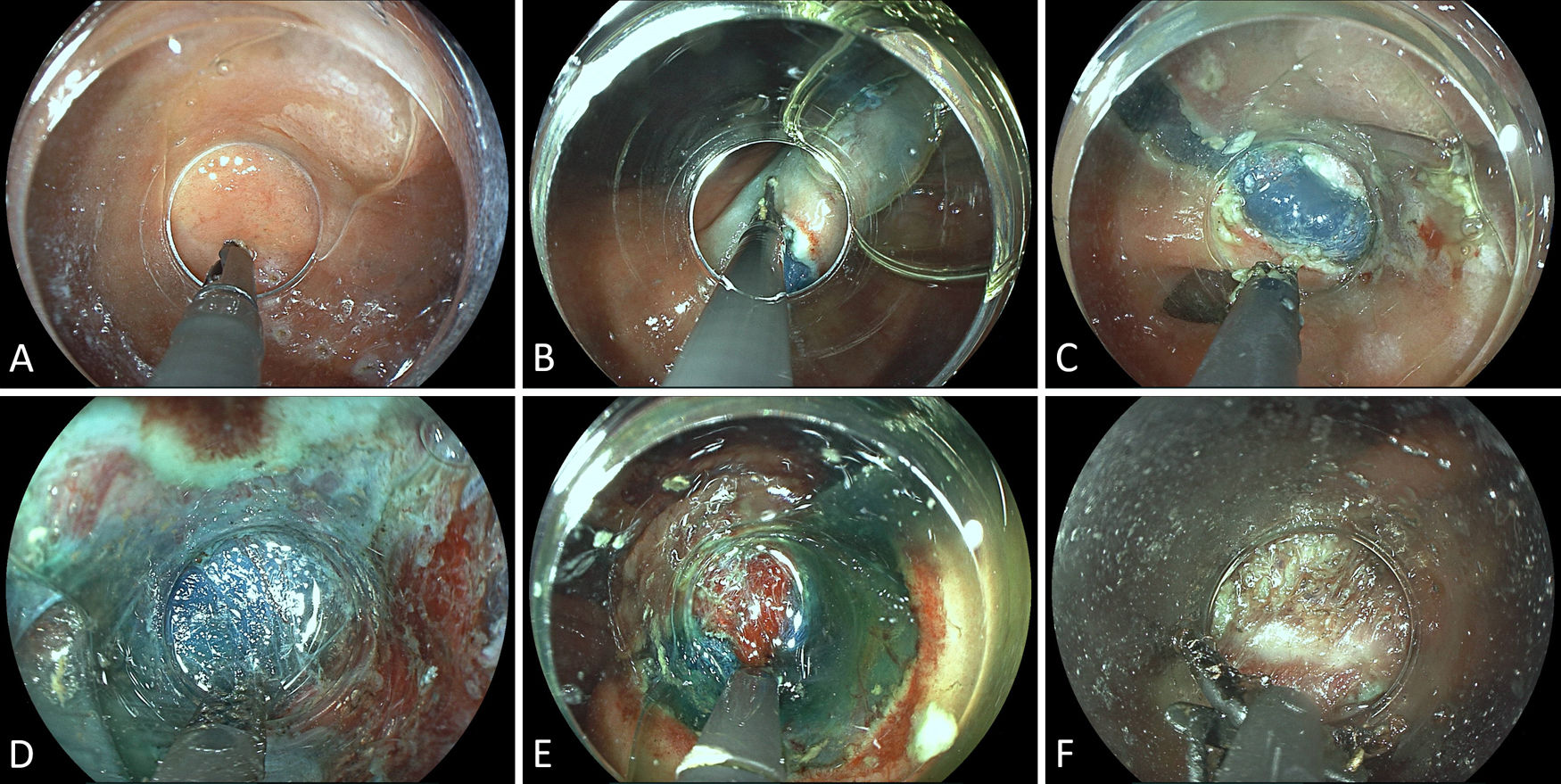
An 84-year-old male patient presented with upper abdominal pain and underwent EGD suggesting early gastric cancer (ECG) at the anterior incisura. White light endoscopy indicated an estimated 30mm Paris 0-IIa+IIc lesion with central redness and depression along with circumferential, peripheral protuberance. The lesion's redness was highlighted by linked colour imaging, and the a priori probability for submucosal invasion was considered high (Fig. 1A+B). Limited biopsies to avoid fibrosis induction and/or complicating final pathology assessment as to ulcer status revealed high-grade dysplasia. With negative imaging studies for potential lymph node/distal metastatic involvement including endoscopic ultrasound (EUS) and CT studies, the patient underwent diagnostic, potentially therapeutic endoscopic submucosal dissection (ESD). With a view to poor endoscopic operability and thinner gastric wall at this specific location, we chose an all-in-one scissor-type ESD knife (Clutch Cutter, Fujinon, Düsseldorf, Germany) as a rotable, serrated grasping forceps with insulated outer blades. More specifically, due to anticipated challenges dissecting over the thinner-walled incisura and underneath the lesion's center with high probability of advanced fibrosis, a decision was made to use a short-blade, 3.5-mm scissor-type knife more established for colorectal applications. With a procedure time of 85min and an individual experience of >50 ESDs, the resection was completed en bloc without major difficulties (Fig. 2A–F). Final pathology of the 50×25-mm specimen indicated a well-differentiated, intestinal-type ECG: pT1b (SM1<100μM), L0, V0, UL+, LM−, VM− with a maximum diameter of 25mm. Due to ulcerative findings and submucosal invasion, outside criteria for endoscopic curability (eCuraC2) were given. In consideration of advanced age and frailty (clinical frailty score 6–7), the patient opted for close surveillance after being adequately informed.1,2
(A) An estimated 30-mm Paris 0-IIa+IIc lesion at the anterior gastric angle with an elevated circumferential protruberance. (B) Linked colour imaging (LCI) highlights the irregular central redness (or rather pinkness) and well-preserved demarcation to the surrounding mucosa. Nonetheless, the probability of submucosal infiltration and high-grade fibrosis was considered high.
(A) Marking the lesion with the tip of the 3.5-mm scissor-type knife (ERBE VIO200D: forced coagulation, effect 3, 30W). (B) Circumferential incision in the so-called “paper-cutting technique” (PCT; Endocut Q, effect 2, duration 3, interval 1). (C) Extension of mucosal incision with the submucosal space already beginning to open up due to cap-related traction, thereby obviating the need for dedicated traction rescue techniques, such as the “clip-with-line” approach. (D) Submucosal space entry and submucosal dissection in retroflexed position facilitated by a small-caliber cap (same electrosurgical settings as for mucosal incision). (E) Preventive coagulation of a large submucosal vessel using the same ESD knife (soft coagulation, effect 5, 100W). (F) Marked central fibrosis correlating to the reddened area cautiously cut through little by little as the final step during the ESD procedure.
Endoscopic submucosal dissection (ESD) continues to disseminate into dedicated Western endoscopy centers. While the utility of scissor-type ESD knives with grasping properties has been reported from many Asian groups, the adoption of these newer devices lags behind. Potential benefits may include, among others, more stability/safety in locations with poor endoscopic operability, all-in-one features without need to switch devices, and potentially increased tip control during step-by-step dissection in fibrotic areas.3
Conflict of interestNothing to declare.