In relation to the case recently published by Dr. Masiques Mass et al.,1 we want to put forward three new cases with different clinical manifestations that have been diagnosed in the last ten years at our centre, wanting to emphasize the importance of clinical suspicion in order to reach their diagnosis.
The first case concerns a 38-year-old woman from Colombia with a history of intermittent abdominal pain and vomiting in her country. She was admitted to the Internal Medicine Department from the Emergency Department due to epigastralgia and vomiting lasting one week and no other associated symptoms. On examination she was afebrile with a soft, depressible, but painful abdomen and induration in the epigastrium. On admission, her blood tests revealed hypertransaminasaemia (GOT 77U/l, GPT 118U/l) and 12,500/mm3 leukocytosis (24% eosinophilia), with no other alterations. Infectious, autoimmune and Mantoux studies were negative. The gastroscopy showed thickened gastric folds, while the chest, abdomen and pelvis CT scan showed perihepatic, perisplenic and pelvic ascites, along with parietal peritoneum and antrum and small intestine thickening. Moreover, a cystic tumour dependent on the right ovary was evidenced.
In light of the radiological findings, we decided to carry out a programmed diagnostic laparoscopy. However, while in hospital, the patient presented a clinical deterioration with a progressive increase of peripheral eosinophilia (up to 51%). Given the suspicion of eosinophilic gastroenteritis, we decided initiate empiric corticoid treatment and an improvement was seen in 24h. In the subsequent surgical intervention, specimens of omentum (no findings), right ovary (benign) and gastric wall were taken, with the presence of mucosal and muscular eosinophils confirming the diagnosis of eosinophilic gastroenteritis.
Discharged with progressively decreasing corticoid treatment, the patient presented a new outbreak requiring admission four months post-diagnosis. Immunosuppressive treatment with azathioprine was initiated due to her corticodependence. At present, eight years post-diagnosis, the patient remains in follow-up, attending Internal Medicine consultations. She occasionally requires low-dose corticoid treatment (alternating 2.5/5mg daily) but has not needed any further admissions, with the immunosuppressive therapy being withdrawn 15 months after its introduction.
The second case concerns a 67-year-old woman with mild bronchial asthma monitored by Pulmonology, and cholecystectomy with recurrent biliary colic. The patient was examined at Allergology consultations for rhinoconjunctivitis, with negative studies for medicines and foods. She was admitted for three weeks of epigastralgia, heartburn and vomiting that was becoming more frequent. She also presented with hyporexia and unquantified weight loss. On examination she was afebrile and had a distended, tympanic and painful abdomen on generalized palpation, with no signs of peritoneal irritation.
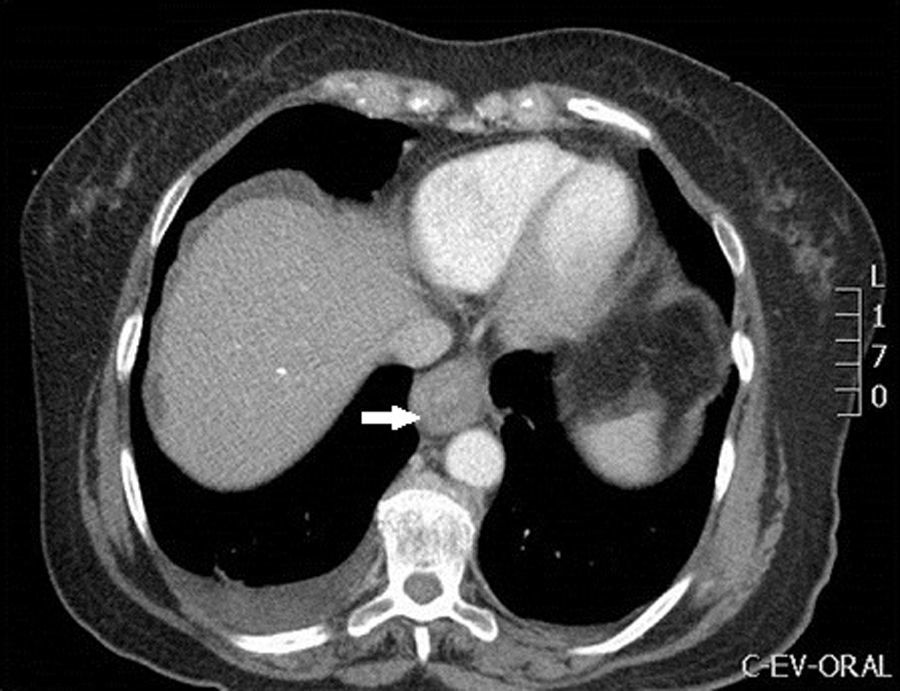
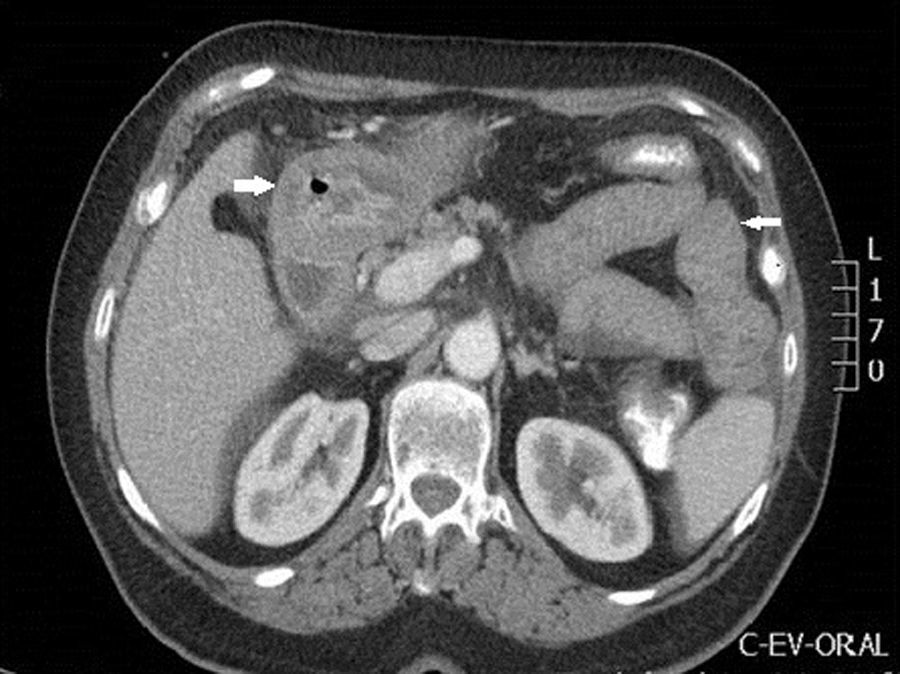
In the blood tests performed on admission, noteworthy findings included leukocytosis of 9600/mm3 with 49% eosinophils (the remaining CBC, liver profile, antitransglutaminase and CRP results were normal). Also performed were an infectious stool study (negative) and an abdominal ultrasound (gastric wall thickening conditioning secondary gastric dilation and minimal amount of ascites in the Douglas and Morrison space, normal bile duct). The study was completed with a chest, abdomen and pelvis CT scan (Figs. 1 and 2), showing a thickening of the middle and distal oesophageal third with oedematization of the submucosal and muscular layers, thickening of the gastric wall and small intestine loops at the duodenum, jejunum and ileum levels.
In light of these findings, a gastroscopy was requested, objectifying chronic gastritis and oedema of the second part of the duodenum, with biopsies taken at all levels. Given the doubtful efficiency of gastric biopsies, the study was completed with an echo-endoscopy with FNA of the gastric wall and ascitic fluid. Treatment with intravenous methylprednisolone 40mg/day was then initiated and a clinical improvement was seen after 48h, with a progressive oral diet being initiated.
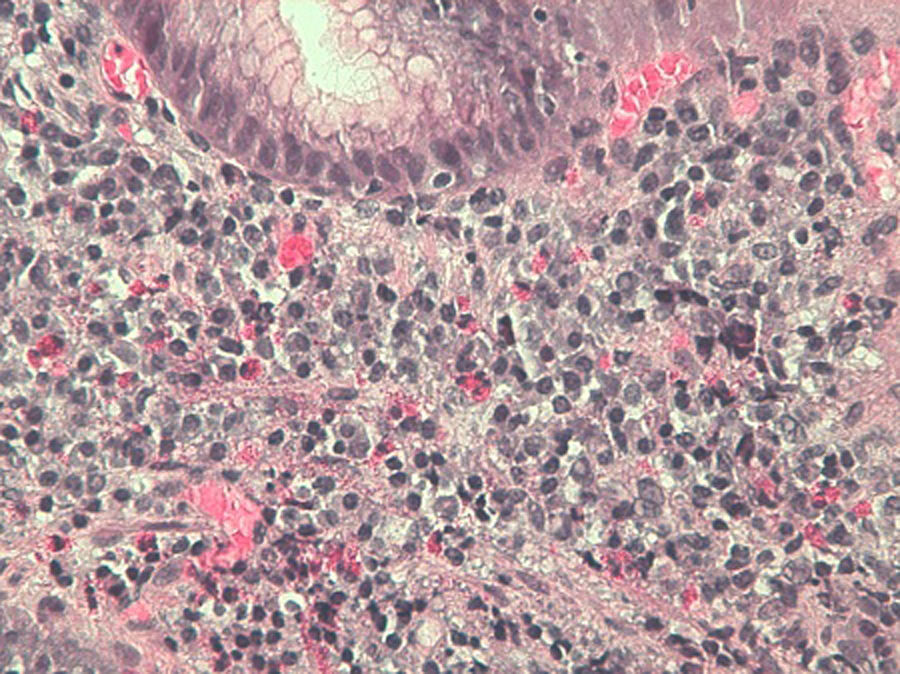
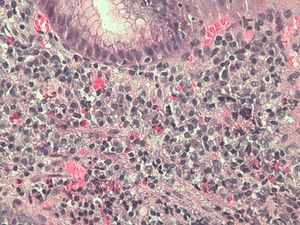
The anatomopathological results confirmed the clinical suspicion, revealing 15–20, 15–20 and >30 eosinophils/field in the biopsies of the oesophagus, stomach and duodenum, respectively (Fig. 3). In the ascitic fluid obtained by means of echo-endoscopy, 97% eosinophils were obtained, with the remaining biochemical parameters returning normal results.
On discharge, the abdominal ultrasound was repeated, seeking the disappearance of the ascitic fluid and an analytical improvement after one week of treatment with 13,800 leukocytes and 1% eosinophils.
The last case is a 56-year-old man with no known allergies, who was examined 11 years prior to the current episode due to gastric dilatation of unidentified aetiology. The gastroscopy showed signs of chronic antral gastritis, with the rest of the examination being normal.
The patient was re-examined due to epigastric pain and weight loss. A CBC (no alterations) and stool study (negative) were requested, and the gastroscopy was repeated, which on this occasion showed a thickening of the rigid antral mucosa without peristaltic movements, thus suggesting gastric neoplasia (ap: HP-negative mild chronic gastritis). The study was completed with a CT scan, which confirmed the circular thickening of the gastric antrum wall and the appearance of regional lymphadenopathies together with ascitic fluid in the wall, suggesting the high probability of advanced gastric neoplasia with peritoneal carcinomatosis. An echo-endoscopy was also added, showing a stenotic antral mucosa with the appearance of neoplastic infiltration, along with food retention in the fundus and an antral thickness of 1cm. Multiple biopsies were taken which were repeatedly negative. As such, due to the high suspicion of neoplasia, we decided to perform a diagnostic laparoscopy. The findings of the surgery were an inflammation of the parietal and visceral peritoneum with adhesions to the gastric wall and a 4cm induration of the gastric antrum with a serous inflammatory appearance. The samples obtained were negative for malignancy, with an abundant eosinophil infiltration appearing in both the peritoneal biopsy and the muscular biopsy of the gastric wall. In light of the findings obtained, treatment with prednisone 40mg/day with clinical improvement was initiated, being progressively lowered until withdrawal.
Given the lack of specificity of the symptomatology, it is necessary to consider this entity in the differential diagnosis. Endoscopy with gastrointestinal biopsy is the technique of choice to determine the diagnosis, demonstrating >20eosinophils/field. Peripheral eosinophilia is not one of the diagnostic criteria, and may not appear in up to 20% of patients. However, when it is present it may be useful in monitoring the treatment response.
Some cases present as cases of intestinal and acute abdomen obstruction requiring urgent surgical intervention. However, surgery should be avoided whenever possible as it is not curative and patients normally respond to medical treatment.
The treatment of choice is corticosteroid therapy with oral prednisone 40mg/day for 7–14 days, followed by a progressive reduction. In some cases, maintenance treatment with low doses of prednisone (5–10mg/day) is necessary, and budesonide treatment may be useful in these cases, given the lower rate of adverse effects.2 In refractory cases, the use of immunosuppressants such as azathioprine may be considered.3
To conclude, note that the rarity of this entity makes clinical suspicion necessary to reach the diagnosis. Besides cases requiring emergency surgery due to an intestinal obstruction, in general it has a good prognosis with a good response to medical treatment, and maintenance treatment is not generally necessary.
Please cite this article as: Campos Ruiz A, Ganchegui Aguirre I, Urtasun Arlegui L, Fernández Laso AB, Spicakova K, Salvador Pérez M, et al. Gastroenteritis eosinofílica: aportación de tres casos clínicos con presentaciones diferentes. Gastroenterol Hepatol. 2017;40:327–329.