Hepatolithiasis is characterised by the presence of gallstones in the hepatic bile ducts, causing repeated symptoms of cholangitis with progressive destruction and dilation of the bile ducts, which leads to the formation of liver abscesses, cirrhosis, atrophy and even cholangiocarcinoma.1 Its treatment has evolved and currently a conservative approach is being attempted, increasing the use of endoscopic techniques and decreasing the number of hepatectomies carried out due to this disease.2 We will describe a case using an assisted technique by way of a flexible cystoscopy with the use of a holmium laser to destroy the lithiasis, reviewing the available literature on the topic.
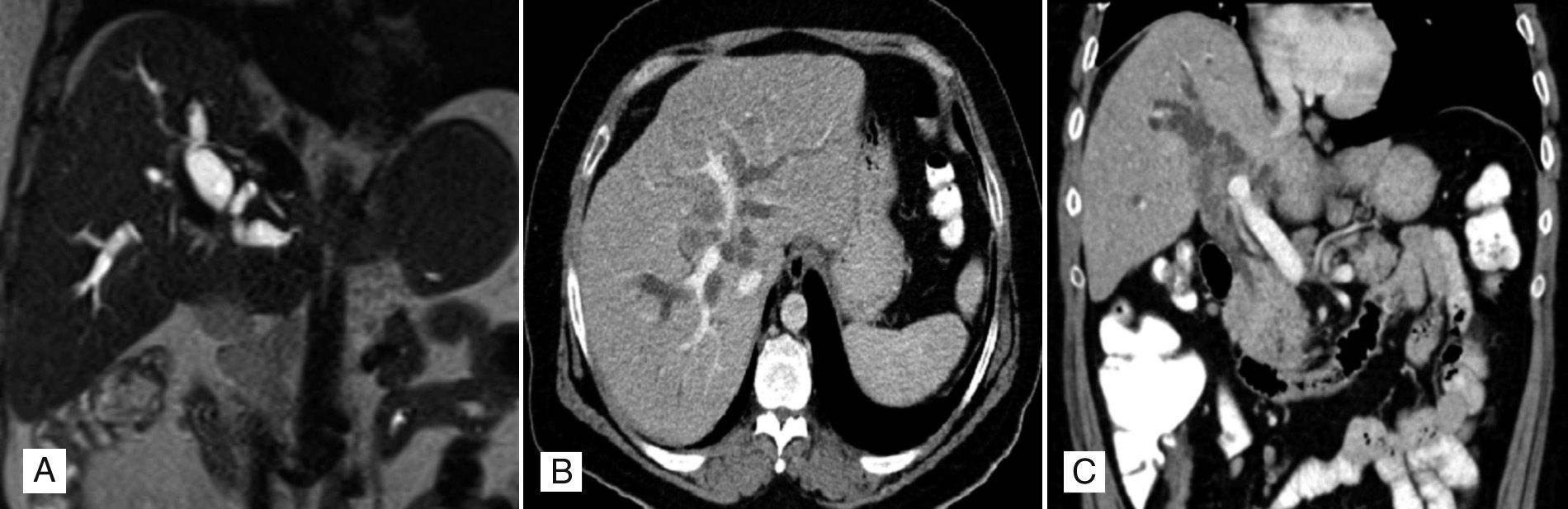
A 55-year-old male patient with a history of multiple sclerosis, clinically asymptomatic, but with elevated transaminase figures. The ultrasound found hepatic steatosis with intrahepatic bile duct dilation, observing multiple hyperechogenic images in its interior. An ERCP was performed that ruled out choledocolithiasis and the CAT scan confirmed a marked dilation of the intrahepatic bile duct, predominantly the right. Images of lithiasis are observed in the tracts of both lobes and in the proximal segment of the common hepatic duct, associated with periportal lymphadenopathies. The MRCP confirms these findings and also highlights obstruction of the common hepatic duct (Fig. 1). A liver biopsy was performed finding periportal fibrosis, acute and chronic periductal inflammation, mild ductular proliferation secondary to chronic obstruction and moderate steatosis. The findings are compatible with chronic stage 2 steatohepatitis and surgery was decided.
Magnetic Resonance Cholangiopancreatography in T2 sequence (A), marked dilation of the intrahepatic bile duct is observed, with images of lithiasis in the tracts of both lobes and in the proximal segment of the common hepatic duct. Contrast-enhanced computerised axial tomography. Transversal slice (B), marked dilation of the bilateral intrahepatic bile duct, images of lithiasis in the tracts of both lobes. Coronal slice (C) dilation of the right bile duct, with images of lithiasis in the proximal segment of the common hepatic duct, associated with periportal adenopathies.
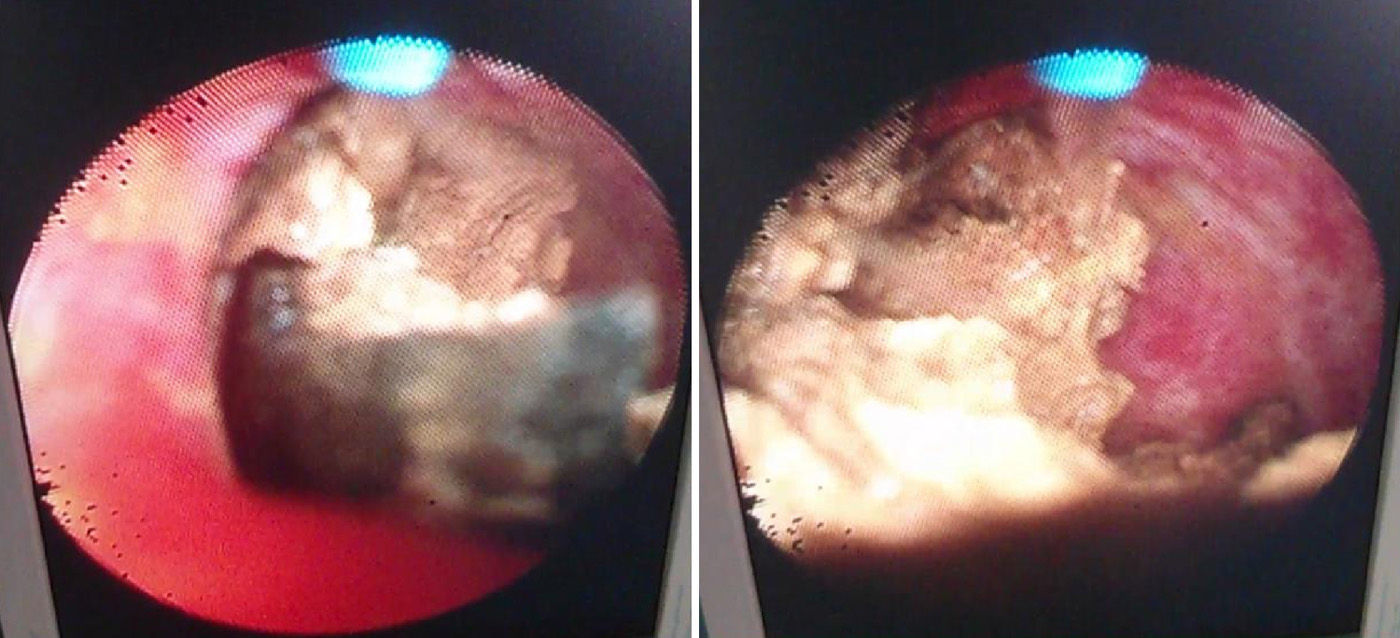
In the same biopsy, agenesis of the gallbladder was observed with hepatic-duodenal fistula, hepatic steatosis, and multiple gallstones in the common bile duct, as well as in all of the intrahepatic biliary tree, mainly in the LLL. Gallstones were endoscopically extracted from both bile ducts and, using flexible cystoscopy, gallstones in the peripheral biliary tracts were extracted by the holmium laser, fragmenting some of them (Fig. 2). Subsequently, the bile duct was resected along with the hepatic-duodenal fistula, finishing with a hepaticojejunal bypass. The definitive pathology analysis for the piece extracted observed the bile duct wall, with fibrosis, non-specific chronic inflammation and areas of bleeding. No evidence of malignancy. The patient progressed favourably with no postoperative complications and currently, 8 months after surgery, is asymptomatic. No pathological findings on the follow-up ultrasound and the blood tests had values within the normal range, bilirubin 0.44mg/dl (normal range: 0–1.00mg/dl), ALT 34.5U/L (normal range: 0–45.0U/L), AST 23.7U/L (normal range: 5–37.0U/L), gamma GT 106.0U/L (normal range: 0–45.00U/L) and alkaline phosphatase 106.0U/L (normal range: 30–120.0U/L). There were no causes that justified the hepatolithiasis in this patient (parasitism or stenosis of the bile duct). It was associated with the congenital changes observed, making it a unique case.
The endoscopic treatment with laser, initially used and developed for urological diseases,3,4 could be the option of choice for bilateral intrahepatic lithiasis, particularly when it occurs in patients in poor general conditions and they are not associated with physical changes like stenosis of the bile duct or hepatic atrophy, thus preventing liver resection.5 In this case we observe the presence of bilateral lithiasis of different sizes in the common and peripheral branches of the biliary tree, and so hepatectomy should be avoided by extracting the biggest and most accessible gallstones manually and leaving the smaller and more peripheral ones to be destroyed via the holmium laser. In this way, a satisfactory surgical result can be obtained.
The holmium laser is a current benchmark system for endoscopic lithiasis fragmentation, as it is less technically complex and has a higher fragmentation rate than its predecessors (pulsed dye-laser, FREDDY, etc.).5,6 It produces and releases pulsed energy, managing to minimalise thermal injuries in neighbouring structures. Its wavelength is very close to the water absorption peak, which grants it a great lithiasis fragmentation capacity and the relative weakness of its shock wave decreases lithiasis movement, preventing it from migrating.3,6
Recently used with a percutaneous approach,7 some series show that its use lessens the surgery time, the postoperative stay, complication rate, and the presence of residual lithiasis. However, it maintains similar relapse rates to those of other treatments, and even higher than hepatectomy in unilateral hepatolithiasis.5,8 Although it is effective, it requires a prolonged biliary access and often multiple procedures in order to ensure the gallstones are fully cleared.9 The ideal route of access for its use would be percutaneous using interventional radiology techniques,7 using the laparoscopic or open surgery approach for cases where tracing of the gallstones is difficult or they are large in size.5,6 Although the indications are still varied, most authors use this technique when there are multiple, unique, bilateral gallstones which are bigger than 2cm, impacted or difficult to trace. They would previously using endoscopic extraction, such as ERCP, where successful.5–9
The use of this technique whether or not in combination with hepatectomy shows us a new perspective that will require new studies in order to confirm its long-term benefits, meaning it would become the technique of choice in the future for the treatment of hepatic lithiasis.
Conflicts of interestThe authors of this paper declare that they have no conflicts of interest.
Please cite this article as: Tejera Hernández AA, Cabrera García ME, Navarro Medina P, García Plaza G, Larrea Olea FJ, Hernández Hernández JR. Hepatolitiasis. Abordaje quirúrgico endoscópico utilizando láser de holmio para su tratamiento. Gastroenterol Hepatol. 2017;40:16–18.