The presence of ectopic pancreatic tissue is a relatively rare entity. Just a few retrospective case series are available in the literature. It is usually an incidental finding without clinical consequences. Between those patients who develop symptoms, bleeding has been described as a rare complication of this condition. We describe a case report of gastrointestinal bleeding and hyperamylasemia secondary to jejunal pancreatic tissue successfully managed with surgery.
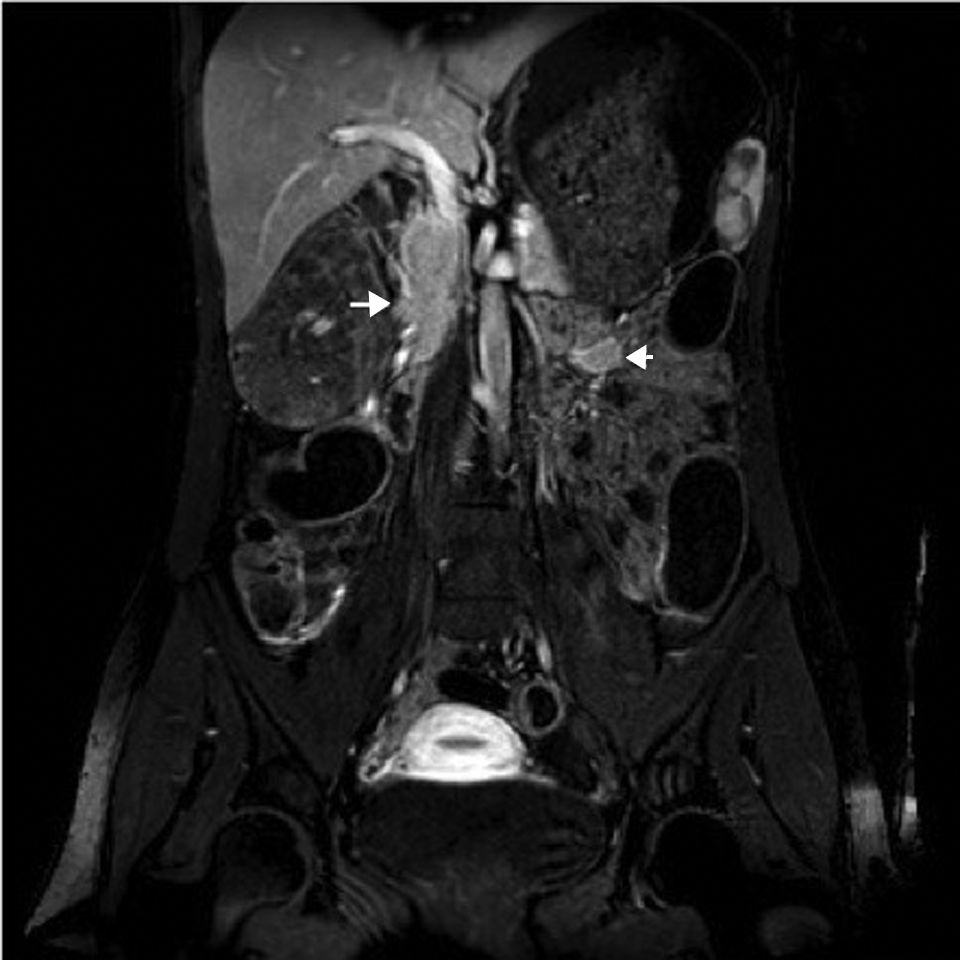
A 31 year-old woman was admitted to our hospital because of gastrointestinal bleeding. She had no relevant past personal or family medical history. She was only taking folic acid because she was planning to become pregnant. She had been also taking nonsteroidal anti-inflammatory drugs during the last month. In the previous week before admission she had observed daily melenic stools. She also complained of mild to moderate colicky abdominal pain. Physical examination was unremarkable. Blood analysis revealed iron deficiency anemia (hemoglobin 7.3g/dL, ferritin <3ng/ml, transferrin saturation 3.1%) and mild hyperamylasemia (pancreatic amylase 128U/L, normal range 13–53). An urgent upper endoscopy showed no signs of gastrointestinal bleeding. A computed tomography was performed and showed a mass in proximal jejunum of 22mm. This lesion showed a morphology and tissue enhancement similar to those in the pancreas, so an ectopic pancreatic tissue was suspected. Capsule endoscopy revealed a submucosal mass located in the jejunum, without active bleeding. This finding was further confirmed by magnetic resonance enterography (Fig. 1). A laparoscopic segmental resection was performed during the admission. The final histological diagnosis revealed a jejunal ectopic pancreatic tissue of 27mm with superficial ulceration (Fig. 2).
An ectopic pancreas is defined as pancreatic tissues lacking vascular or anatomic communication with the normal body of the pancreas, yet possessing histological features of pancreatic acinar formation, duct development and islets of Langerhans with independent blood supply and ductal system.1–3 It is supposed to arise due to the persistence of a duodenal evagination involved in the normal development of the pancreas. Another hypothesis suggests the presence of pancreatic metaplasia of the endodermal tissue in the gastric mucosa.4 It has been described in multiple locations along the gastrointestinal tract, being the stomach the most common (25–38%).4 There are also cases in the duodenum (9–36%) and jejunum (0.5–27%), as well as other extraintestinal locations. It often arises in within the submucosa (75%) but sporadically also in the muscularis propria and serosa.5 Heinrich described four types of pancreatic heterotopia initially in 1909. In 1973 Gaspar–Fuentes included some modifications to this classification.6 This classification is based upon the structures observed in the ectopic tissue (pancreatic ducts, acinar tissue and islet cells).
In previous case series only 73 out of 212 patients with ectopic pancreatic tissue were symptomatic. Bleeding from an ectopic pancreas was observed only in 3 of them.7 Another retrospective study reported 3 cases of ectopic pancreas causing bleeding in the small bowel among 76 cases of obscure gastrointestinal bleeding.8 These data reflect the low incidence of symptoms in this relative rare entity. Nevertheless this type of lesions should be suspected when evaluating an obscure gastrointestinal bleeding, although it requires a high index of suspicion. Hyperamylasemia has been described in complicated ectopic pancreas but neither of them in a case of bleeding. This is the first report describing this relationship. Probably if diagnostic techniques continue to improve we can expect an increase in the incidence of these disorders.