Tuberculosis (TB) is an infectious disease, the prevalence and incidence of which are increasing in our area as a result of immigration and the use of immunosuppressants. Although TB usually affects the lungs, it is a systemic disease and can occur in other parts of the body; extrapulmonary TB is common in less developed countries.1
Although gastrointestinal involvement is unusual, it is something we must be aware of, since TB has the ability to mimic other disorders common in our area, such as Crohn's disease (CD).2 Numerous studies have attempted to create diagnostic algorithms to facilitate the differential diagnosis between these conditions.3–9 According to several recent publications,5–9 the final diagnosis of gastrointestinal TB should include epidemiological, clinical, radiological, endoscopic and histological findings.
We present a case of Mycobacterium tuberculosis with ileocolic and pulmonary involvement to illustrate the importance of the differential diagnosis of this disease, as the characteristics do not differ greatly from CD, but the prognosis depends to a large extent on the early introduction of a suitable treatment.
With this case report, we also highlight the main characteristics of intestinal TB, both clinical and radiological, endoscopic and histological, underlining the importance of the epidemiological context, which plays a crucial role in the diagnostic process.
Case reportIn November 2015, a 31-year-old male from Romania and resident in Spain for five years was admitted to our hospital with a two-month history of abdominal pain located in the right iliac fossa and umbilical region, radiating to his back. He also had associated weight loss of 10kg, fever and night sweating, asthenia and nausea without vomiting. The patient smoked about 20 cigarettes a day and had no relevant medical/surgical history. He had apparently not had any contact with any patients with active TB.
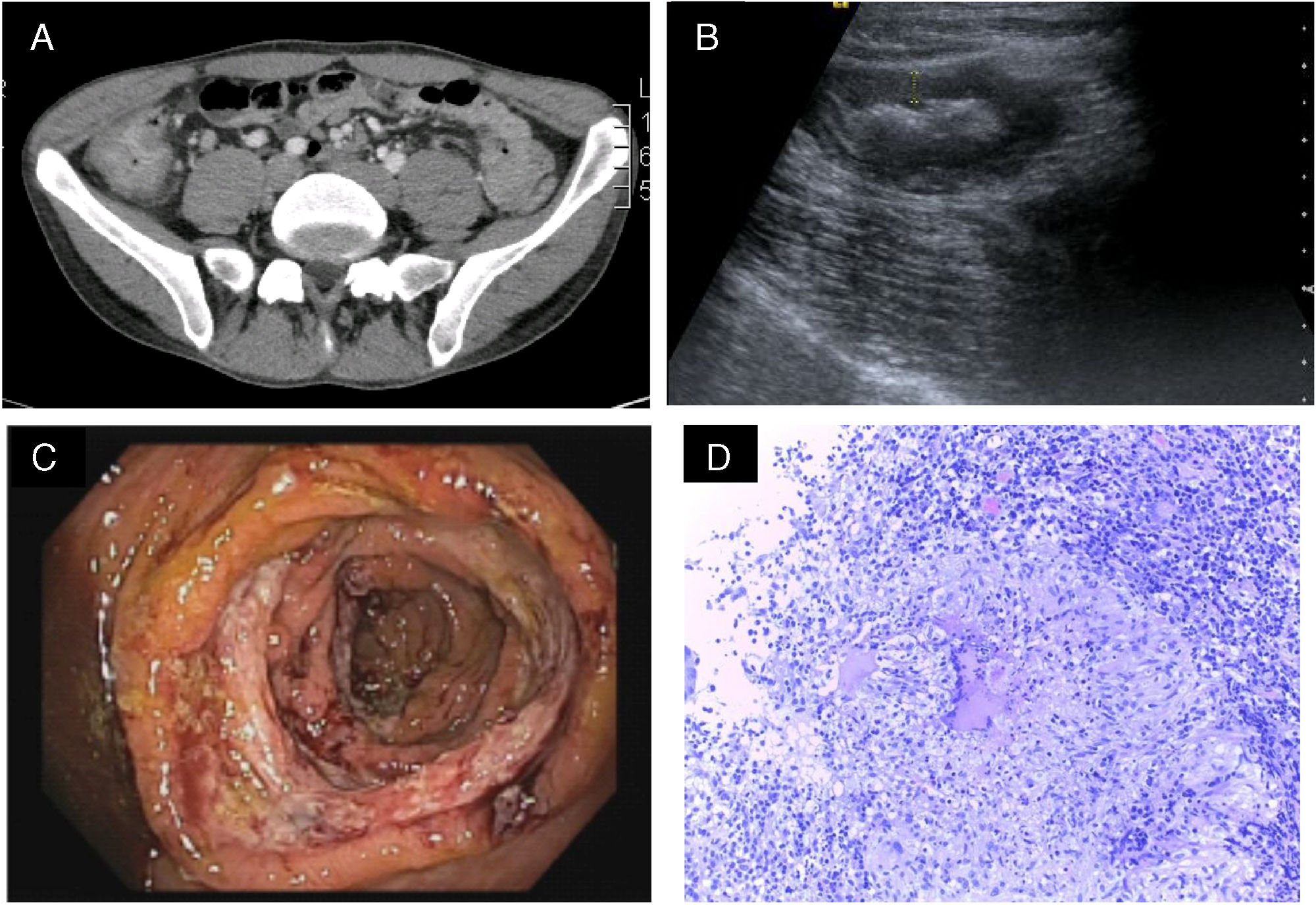
Analytically, tests showed elevated C-reactive protein (58.9mm/l) as an acute phase reactant, with a normal cell count. Abdominal ultrasound and computed tomography (CT) of abdomen and pelvis showed extensive ileocolitis from the terminal ileum to the ascending colon, with wall thickening, peri-caecal fat involvement and multiple mesenteric lymphadenopathy, all of which as a first possibility could correspond with CD (Fig. 1). The chest X-ray showed a large cavitary nodule in the right upper lobe.
The colonoscopy found oedematous mucosa, friable to rubbing by the endoscope, and numerous circumferential ulcers in the terminal ileum, caecum and ascending colon. The ileocaecal valve was stenosed and deformed, but it was patent. Multiple biopsies were taken, and the histology showed chronic-looking granulomatous ileocolitis, abundant inflammatory infiltrate and numerous caseating granulomas (Fig. 1). With these findings, the QuantiFERON test, a bronchoalveolar lavage and Lowenstein culture were performed, all of which were positive, confirming the diagnosis of active pulmonary TB with intestinal involvement.
Anti-tuberculosis treatment was started according to the guidelines accepted at that time with good tolerance and clinical improvement. Within just a few days the patient's abdominal pain and fever and sweating had subsided.
DiscussionThe case we have presented here underlines the importance of the clinical and epidemiological context of each patient, which must be taken into account in the diagnostic process. We also highlight the role of a good differential diagnosis, supported by radiological, endoscopic and histological findings, of two similar disorders like intestinal TB and CD, with completely different treatments.1,5,7,8
Intestinal TB is an unusual manifestation of extrapulmonary TB.1 The area most commonly affected is the ileum, followed by the colon. It is known as “the great imitator”, as its main manifestations are very nonspecific, and diagnosis therefore has to be based on a set of clinical characteristics and complementary test results. It tends to have a more acute onset than CD. However, it can also manifest itself as a subacute or chronic disease. The symptoms most commonly reported are fever, night sweats and weight loss.5 Perianal disease is an uncommon finding in TB, supporting the diagnosis of CD.1
Imaging tests, particularly CT enterography, can help guide us. Single or isolated ileal focal lesions and necrosis or calcifications in the mesenteric lymph nodes are typical findings of intestinal TB, while proximal and segmental involvement of the small intestine or the presence of fistulas should steer us towards CD.6
Endoscopically, in both diseases we may find circumferential ulcers or scars in the mucosa of the colon or terminal ileum. Taking biopsies of diseased tissue for histological and microbiological diagnosis help with the definitive diagnosis (PCR, Lowenstein medium culture, Ziehl-Neelsen staining). Colonoscopy is also useful in the follow-up and assessment of the treatment response in these patients.5
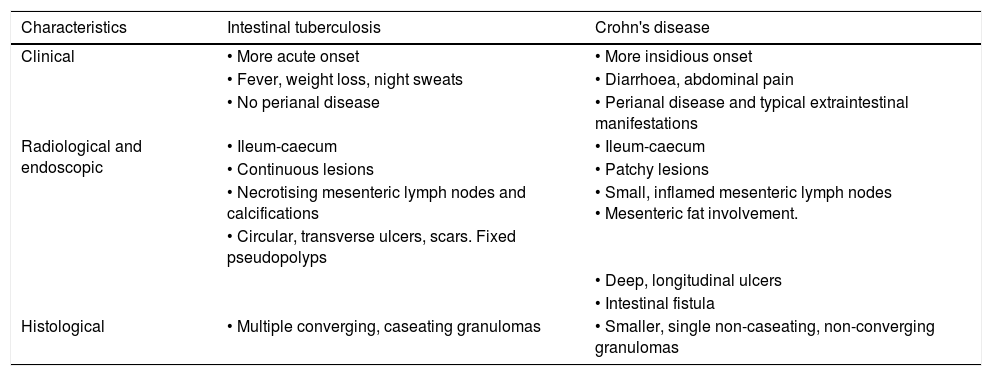
Although not very sensitive, the identification of caseating granulomas is a very specific finding of intestinal TB.1 Given the similarity of the lesions with those in CD, it is important that the samples be examined by an expert pathologist with a high level of clinical suspicion. The main characteristics of CD and intestinal TB are summarised in Table 1.
Differential diagnosis between Crohn's disease and intestinal tuberculosis.
| Characteristics | Intestinal tuberculosis | Crohn's disease |
|---|---|---|
| Clinical | • More acute onset | • More insidious onset |
| • Fever, weight loss, night sweats | • Diarrhoea, abdominal pain | |
| • No perianal disease | • Perianal disease and typical extraintestinal manifestations | |
| Radiological and endoscopic | • Ileum-caecum | • Ileum-caecum |
| • Continuous lesions | • Patchy lesions | |
| • Necrotising mesenteric lymph nodes and calcifications | • Small, inflamed mesenteric lymph nodes • Mesenteric fat involvement. | |
| • Circular, transverse ulcers, scars. Fixed pseudopolyps | ||
| • Deep, longitudinal ulcers | ||
| • Intestinal fistula | ||
| Histological | • Multiple converging, caseating granulomas | • Smaller, single non-caseating, non-converging granulomas |
Medical treatment with anti-tuberculosis drugs is the first step when intestinal TB is suspected, and can be used empirically for a short time until the diagnosis is confirmed.8 Surgery is generally reserved for complications such as obstruction or stricturing, but there have been reports of endoscopic management in a few isolated cases, with good outcomes.10
Two recent studies developed diagnostic algorithms, combining epidemiological, clinical, radiological, endoscopic and histological characteristics. However, they require wider use to verify their effectiveness in routine clinical practice.5,6 TB is a real worldwide public health problem. A high index of suspicion and a methodical multidisciplinary diagnostic process are essential for early diagnosis and early treatment of these patients.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Morales N, García-Campos M, Cordón G, Iborra M. Tuberculosis intestinal, simulador de la enfermedad de Crohn: diagnóstico diferencial. Gastroenterol Hepatol. 2019;42:29–32.