The symptomatic onset of intestinal malrotation in adulthood is uncommon and usually presents with acute processes of intestinal occlusion, intussusception or volvulation that require urgent surgical treatment.1 On the other hand, when they present with nonspecific and chronic digestive symptoms, there is controversy as to the treatment of choice, the most widely applied being surgery using the Ladd procedure to avert the future appearance of these potentially surgical complications.1–3
Despite this, there are some published cases of patients with mild or moderate symptoms in whom conservative treatment is chosen, with one noteworthy article published in this journal by Núñez-Gómez et al.4 The article describes an adult patient with chronic symptoms of abdominal pain coursing over 14 years, managed conservatively with light meals and the usual analgesics, with symptomatic control and without the patient presenting relevant complications during follow-up.
We present a case with a similar clinical course and characteristics, albeit with the peculiarity that the patient only presented significant clinical improvement after being diagnosed and treated for a small intestinal bacterial overgrowth (SIBO).
The patient was a 60-year-old man diagnosed 12 years previously with intestinal malrotation by CT scan due to nonspecific digestive symptoms with onset 4–5 years prior to diagnosis. The predominant symptoms were meteorism and dysmotility-type dyspepsia, and particularly diffuse abdominal distension and discomfort, daily and almost continuous, which did not interfere in his daily activities or night rest. There was no abdominal pain, vomiting, or weight loss. At diagnosis, a complete study of the small and large intestine was carried out by means of blood tests, radiology and endoscopy, including endoscopic capsule, in which potentially surgical complications were ruled out, as were other diseases such as Helicobacter pylori infection, inflammatory bowel disease, coeliac disease or diverticula.
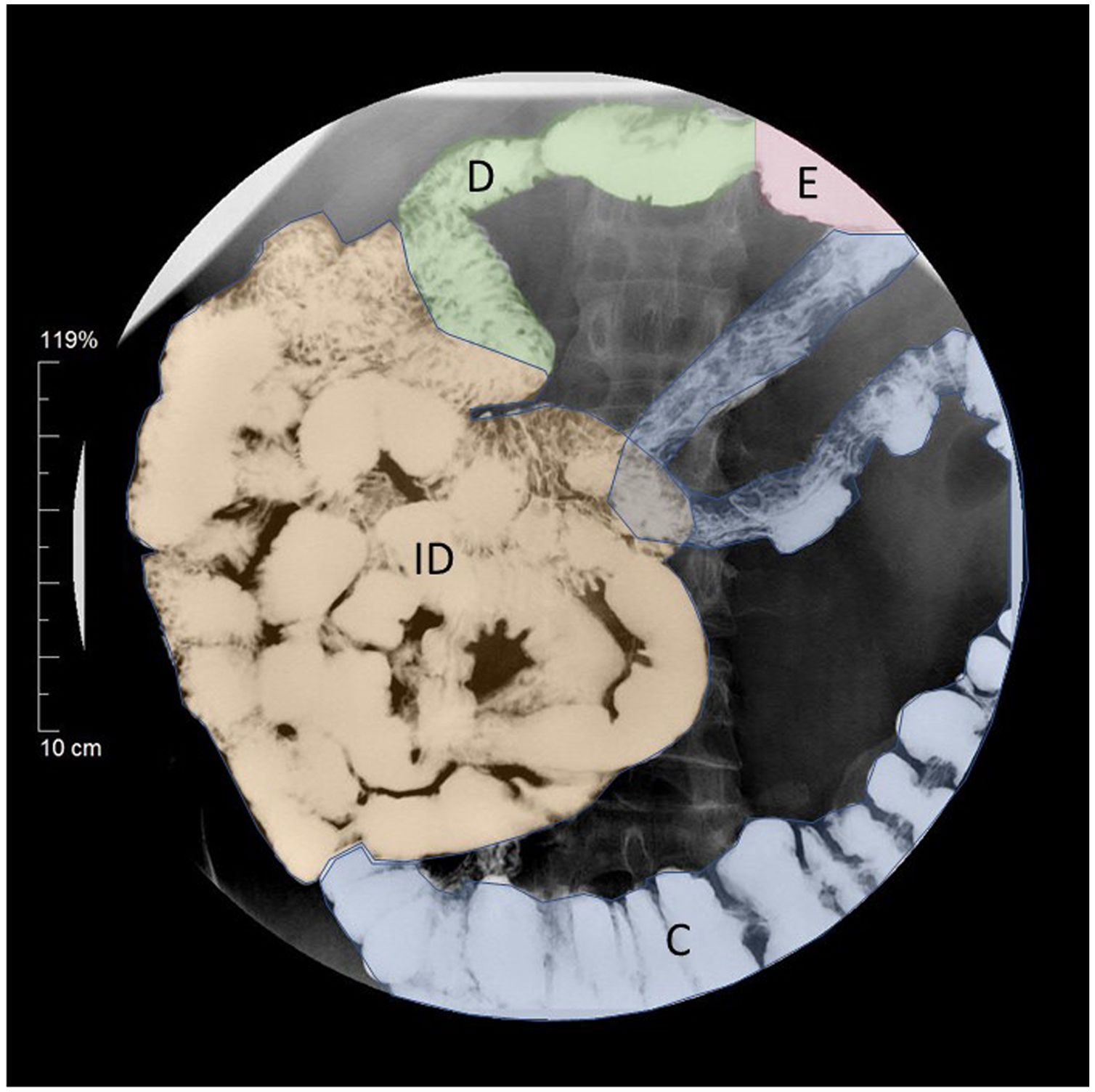
Symptom intensity was variable, including periods in which the patient was practically asymptomatic, without requiring urgent medical care or presenting relevant complications at any point. Annual follow-up was performed with a CT scan or barium contrast (Fig. 1). Pharmacological treatment with antispasmodic, analgesic, propulsive, probiotic and prokinetic agents, as well as the use of light, fat-free meals and lactose- and FODMAP-free diets only provided partial symptom control. However, two years ago, SIBO was detected by aspirated air with an oral lactulose overload test, and after chronic treatment with oral rifaximin 400mg every 12h for one week every month was prescribed the symptoms improved substantially and have been controlled until the present day.
As in the article by Núñez-Gómez et al.,4 in our case we observed that conservative management of patients with mild or moderate symptoms is possible and is not necessarily associated with the appearance of urgent surgical complications. Our patient's significant clinical improvement after starting treatment for SIBO was very striking. Moreover, this improvement has been maintained over time and was not achieved with any of the other treatments used.
Despite the limitations on the study of the intestinal microbiota, SIBO is an easily diagnosed condition thanks to aspirated hydrogen detection tests following oral glucose or lactulose solution overload. Its pathogenesis is multifactorial, with slow transit and disruption of the intestinal anatomical barriers as triggering mechanisms being particularly prominent. It is therefore related to conditions such as small-bowel diverticulosis, stenosis, inflammatory disease, irritable bowel syndrome or surgical resections.5 However, its association with intestinal malrotation has not been investigated, although taking the aetiopathogenic analogies of intestinal malrotation with some of the diseases that are associated with SIBO into account, we believe that this relationship between the two conditions may exist.
In our opinion, intestinal malrotation should be taken into account in the study of nonspecific digestive symptoms and we believe it is useful to look for SIBO when symptoms are consistent or there is no improvement with other treatments. However, specific studies will be required to confirm the association of these two pathologies.
Conflicts of interestThe authors declare that they have no conflicts of interest.
To Dr Abel Gregorio Hernández and Ana Serrano Prats.
Please cite this article as: Alventosa Mateu C, Núñez Martínez PC, Castillo López GA, Pascual Romero A. ¿Está asociada la malrotación intestinal sintomática en el paciente adulto con el sobrecrecimiento bacteriano de intestino delgado? Gastroenterol Hepatol. 2020. https://doi.org/10.1016/j.gastrohep.2020.04.008