Gastroesophageal reflux disease (GORD) is a condition with high prevalence in Spain which significantly alters patients’ quality of life. Treatment of GORD is essentially medical as most patients respond adequately to conservative treatment, based on general and diet-related measures. These are often accompanied by pharmacological treatment with antacids, histamine H2 receptor blockers, proton pump inhibitors and prokinetic drugs.1
Nevertheless, surgery plays an important role in the treatment of GORD. In general, the indications for surgery can be summarised as a desire to stop taking medication, lack of adherence, presence of adverse effects, oesophagitis that is refractory to medical treatment or the existence of complications (oesophageal ulcer, stenosis and Barrett's oesophagus). The techniques used are many and varied, with laparoscopic fundoplication being the most common today. In the case of complicated gastroesophageal reflux in which the anatomy of the gastro oesophageal junction (GOJ) may be altered due to previous surgeries or the presence of complications of oesophagitis, such as peptic stenosis or short oesophagus, dilatations associated with conventional antireflux surgery, Collis gastroplasty—alone or in combination with Nissen fundoplication—oesophageal resections with total or partial replacement with stomach, jejunum or colon, and total duodenal diversion (TDD) have all been described. The last technique, described in 1961, is recommended by various groups as the ideal technique for the treatment of surgical recurrence and certain complications of GORD.
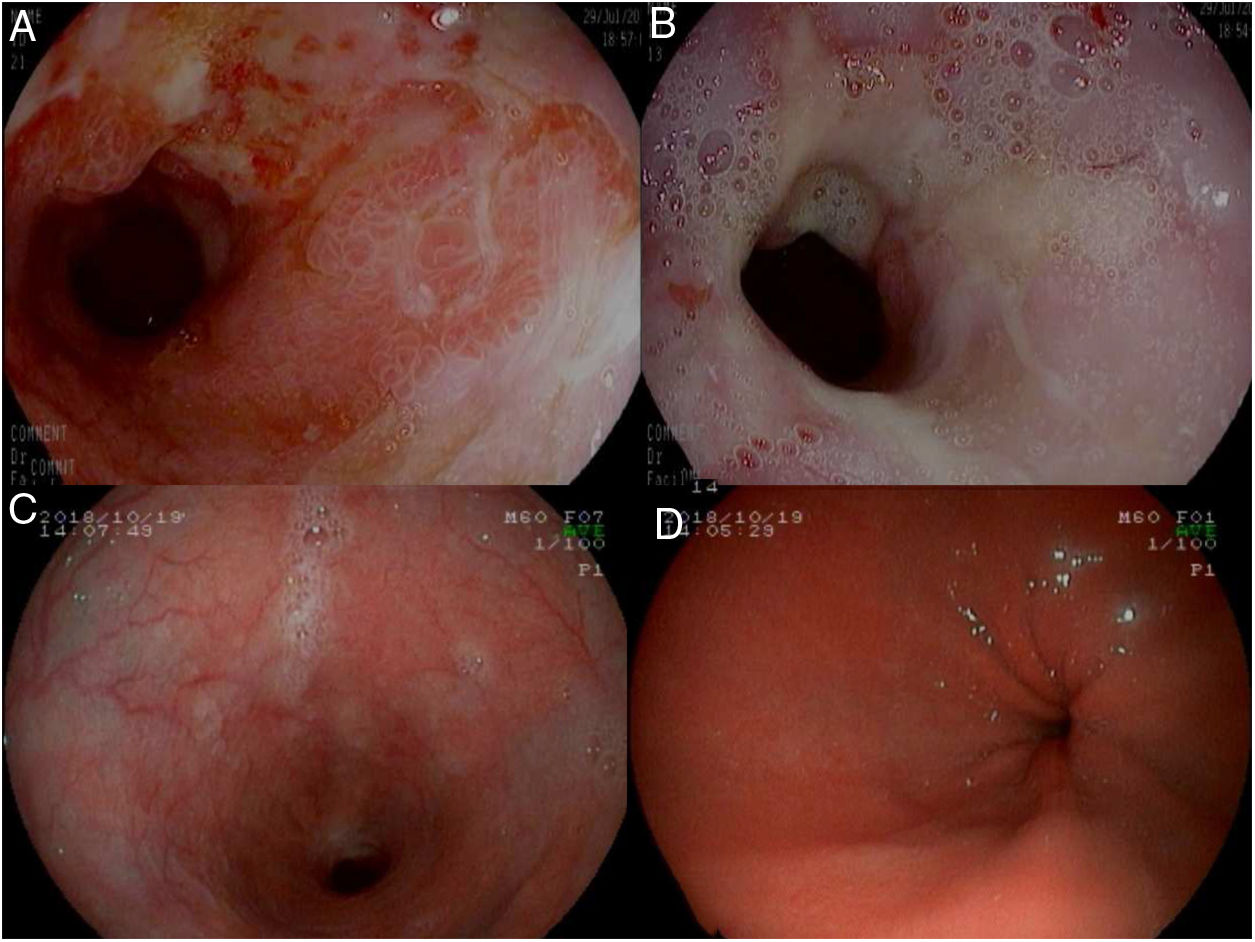
We present the case of a 72-year-old male patient with a personal history of cholecystectomy and a history of allergic reactions to proton pump inhibitors (PPIs), H2 blockers and domperidone, who attended a consultation for pyrosis which had been ongoing for years, associated with dysphagia in recent months. The gastroscopy revealed a stenosis of 3–4cm in length 32cm from the alveolar arch, easily passed with the endoscope, with the presence of fibrinous ulcers around the whole circumference, with two areas of raised mucosa and adenomatous appearance on the stenosis, biopsy of which revealed non-specific ulceration (Fig. 1A and B). A functional study was performed, confirming the existence of reflux with oesophageal hypomotility. Given that neither PPIs nor H2 blockers could be used, treatment was started with Ziverel® (hyaluronic acid and chondroitin sulphate). In the review at two months, the patient reported that the symptoms persisted and the control gastroscopy showed the same findings, so the decision was made to use surgical treatment. Given the existence of stenosis, the associated motor disorder and the difficulty of management in the event of a recurrence due to drug allergies, the decision was made to perform a total duodenal diversion via laparoscopy.
(A and B) Initial gastroscopy. Stenosis of 3–4cm in length that is easily passed with the endoscope, with the presence of fibrinous ulcers around the whole circumference (A) and two areas of raised mucosa and adenomatous appearance (B). (C and D) Control gastroscopy at 12 months from the surgery, with no evidence of lesions.
The patient's postoperative evolution was satisfactory and he was discharged six days later. Currently, 18 months from the surgery, the patient is asymptomatic, with the control gastroscopy showing no evidence of lesions (Fig. 1C and D).
The total duodenal diversion (TDD) described by Holt and Large consists of performing a bilateral truncal vagotomy, antrectomy and reconstruction of the tract using a gastrojejunal anastomosis, in which the Roux-en-Y limb measures 70cm in length, with the aim of ensuring that the content of the stomach is neither acidic nor alkaline due to the length of the Roux-en-Y limb which avoids any risk of bile reflux to the gastric pouch.
TDD has been used in patients with recurrent symptoms after a classic anti-reflux operation,2,3 in GORD associated with severe oesophageal motor disorder or scleroderma, and has even been proposed as a first-line operation for Barrett's oesophagus complicated by ulcer or stenosis.
In 1996, Fekete et al.4 published a series of 107 surgically treated patients with regression of oesophagitis at three months in 89% and postprandial pH-metry with reflux control in 92% of cases. Most of the more recent comparative prospective studies with objective clinical assessment with endoscopy and histology have been performed in patients with Barrett's oesophagus, demonstrating success in 95% after TDD and in 65% after Nissen fundoplication (p<0.01).2,3
This technique involves gastric resection and Roux-en-Y gastrojejunal anastomosis, so its complications are associated with the known postgastrectomy syndromes (early and late Dumping syndrome, diarrhoea, cholelithiasis and Roux limb syndrome). Nevertheless, their frequency is low and the same is true of mortality (0–1.8%). Moreover, the precision of the surgical technique offered by laparoscopic dissection could further reduce these complications.5
To conclude, TDD is not the standard surgical treatment for patients with GORD. However, in select cases, it is preferable to procedures that include oesophageal resection due to its good outcomes and low morbidity and mortality. Laparoscopic execution of the technique in turn offers the benefits of a minimally invasive approach, especially as regards local and general symptoms, possible repeat operations and quality of life.
Please cite this article as: Romera Barba E, Navarro García MI, González-Costea Martínez R, Torregrosa Pérez NM, García Marcilla JA. Diversión duodenal total laparoscópica en el tratamiento de la enfermedad por reflujo gastroesofágico complicada. Gastroenterol Hepatol. 2019;42:492–493.