Obesity is a chronic and incurable disease that has become a major public health concern worldwide. Treatment of overweight patients is challenging and less invasive alternatives to the surgical procedures are sought for the treatment. In this context, a placement of an intragastric balloon (IGB) by endoscopic route is an efficient, safe and minimal invasive procedure for the treatment of obesity.1 Although it is a safe procedure, some severe complications may occur.2,3
Fungal colonization of IGBs is a rare adverse, generally the patients are asymptomatic, and no treatment is required. Fungal colonization may lead to degradation of the balloon's silicone and facilitate the balloon extraction, but paradoxically it also may lead to serious complications during IGB removal. The authors report the case of a difficult explant of an IGB with severe fungal colonization.
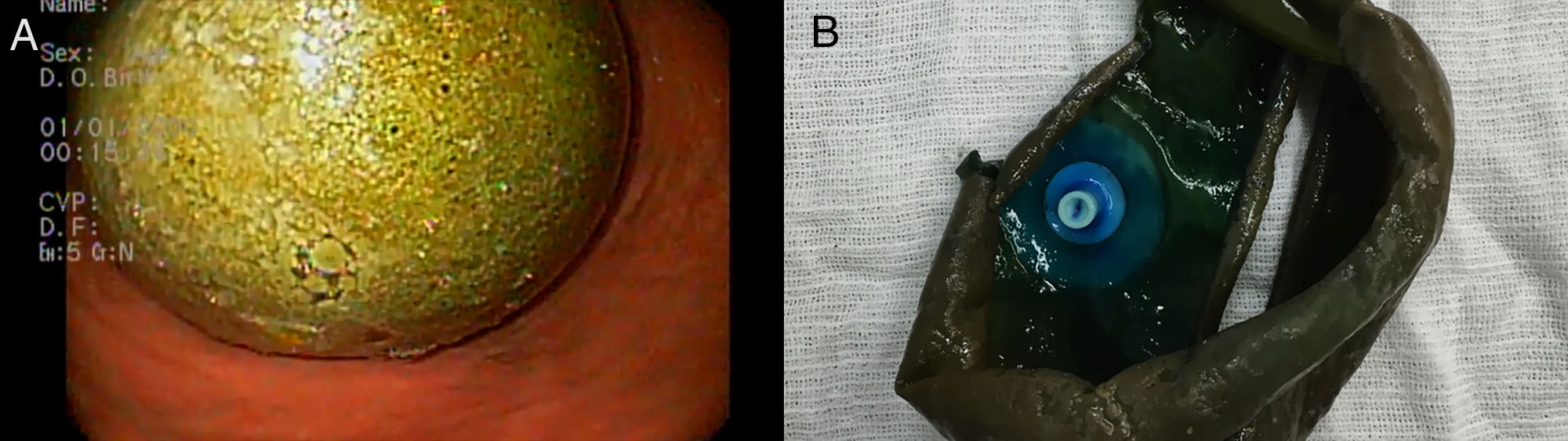
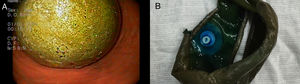
A 43-year-old female patient with a body mass index of 30.7kg/m2, but without comorbidities, who was submtitted to IGB placement (Orbera, Apollo Endosurgery, Austin, TX) to treat obesity. In the six months following the procedure, the patient was treated with proton pump inhibitors (PPI; pantoprazole magnesium 40mg id) and she lost about 18kg. Near the date scheduled to remove the IGB, the patient began with persistent fever and myalgia. The complete blood count showed leukopenia (2.0×109/L) and thrombocytopenia (48×109/L) and her serology (IgM) was positive for Dengue fever. Conservative treatment was instituted with rest and hydration and the patient had a good evolution. The removal of the IGB was postponed until normalization of the platelet count and resolution of the infection. Thus, explant was performed seven months after the IGB placement. Upper endoscopy, performed under general anesthesia and orotracheal intubation, identified intense colonization of the balloon by fungus (Fig. 1A). The IGB was emptied according to the conventional technique using a balloon removal needle (GFE Brasil Ltda.) with the contents being aspirated completely. However, removal of the IGB using Raptor tweezers (US Endoscopy) was unsuccessful; it was impossible for the IGB to pass through the cardia as it was rigid with rough walls due to the fungal colonization and because of its friability. It was then decided to cut the balloon in the middle using bariatric scissors (Europa Medical, Recife, Brazil) to reduce its thickness and facilitate its extraction (video). Finally, the Raptor tweezers were again introduced and the IGB was successfully removed without further complications (Fig. 1B).
Balloon contamination by fungus is one frequently overlooked complication of these devices.4 Visible fungal infection occurs in up to 5.8% of the IGB and may even be more frequent in air-filled balloons (up to 14.9%).4 Currently there is no consensus about the triggering factors of contamination. One possible explanation, could be the contact of the balloon with the gastric mucosa, causing it to remain constantly moist and together with the food debris on the balloon's surface, could promote an environment suitable for microbial proliferation. This explanation has already been reported in an attempt to explain the fungal contamination of gastrostomy tubes.5 Also, the gastric emptying delay provoked by the balloon, the patient's habits, such as smoking, the chronic use of PPIs, and the IGB balloon after 6 months, may also play a role, favoring the contamination.
In most cases of IGB contamination, the colonization is identified at the time of the balloon removal and the patients are asymptomatic. The routine prophylactic use of antifungal drugs to avoid fungal infection is not recommended.4
In the recent published Brazilian IGB Consensus,5 in the presence of diagnosis of fungal colonization of the balloon, 36.4% of the participants agreed that nothing should be done, 27.3% recommended interruption of PPI therapy, 18.2% recommended PPI interruption and antifungal drug administration, and 18.2% recommend antifungal drugs alone. Also, there was no recommendation for balloon removal owing to this adverse event.4 Currently there is also no consensus on any recommendation to avoid fungal colonization.
IGB extraction is a safe procedure, with few severe complications, that are generally treated endoscopically.6 The difficulty of removing the IGB may be related to several factors, including those related to the patient (presence of severe esophagitis, stenosis, etc.), the extraction technique, the degree of sedation of the patient and, in some cases, the deterioration of the IGB material in cases of late withdrawal.6 Therapy with PPI associated with low immunity due to Dengue infection and removal of the balloon more than six months after its placement, could have predisposed to fungal colonization in the case reported. Colonization can make the structural components of the IGB more rigid and friable making the explant difficult. The technique described herein may be used as a salvage therapy for extraction of difficult IGB's cases and to reduce the risk of complications, as this is a safe option for rigid balloons removal.
Conflicts of interestNone declared.