Inflammatory bowel disease (IBD) is a clinical entity with multisystemic involvement. The incidence of extraintestinal manifestations of IBD oscillates between 21 and 41%, being more common in Crohn's disease (CD) than in ulcerative colitis (UC).1 Respiratory manifestations are the least common, and when they appear they are often associated more with UC than with CD.2 Respiratory alterations in IBD vary from subclinical manifestations to alterations of the upper and lower airways and parenchymal diseases, that in some cases can lead to severe conditions. The clinical characteristics of IBD as regards its phenotype and degree of activity have not been related to pulmonary dysfunction. However, there are studies that suggest that the disease's duration and chronicity may be a respiratory protective factor.3
We present the case of a 31-year-old male patient, smoking 10 cigarettes/day, with no personal history of interest. He attended a consultation due to a clinical picture of dysmotility-type dyspepsia which had been ongoing for one year. The physical examination was unremarkable. The blood test was notable for: ESR 29mm/h, fibrinogen 736mg/dl, CRP 129mg/l, leukocytes 13,000/mm3, 78% neutrophils and TSI 9%. The gastroscopy revealed a stenosis of inflammatory/cicatricial appearance with ulceration at its base in the second part of the duodenum. The biopsies were compatible with CD.
One month later, in a review, he reported diarrhoea consisting of 3–4 soft stools/day without blood and febrile peaks together with erratic abdominal discomfort. Likewise, in the last two weeks he had started to have a dry cough and non-specific thoracic discomfort. Given the clinical deterioration, it was decided to admit him for the following additional tests:
A chest x-ray on which an alveolar opacity was observed in the upper right lobe compatible with infectious inflammatory involvement.
HCV, HBV and HIV serologies negative. ANA negative. Blood cultures negative. Sputum bacteriology negative. Mantoux test negative.
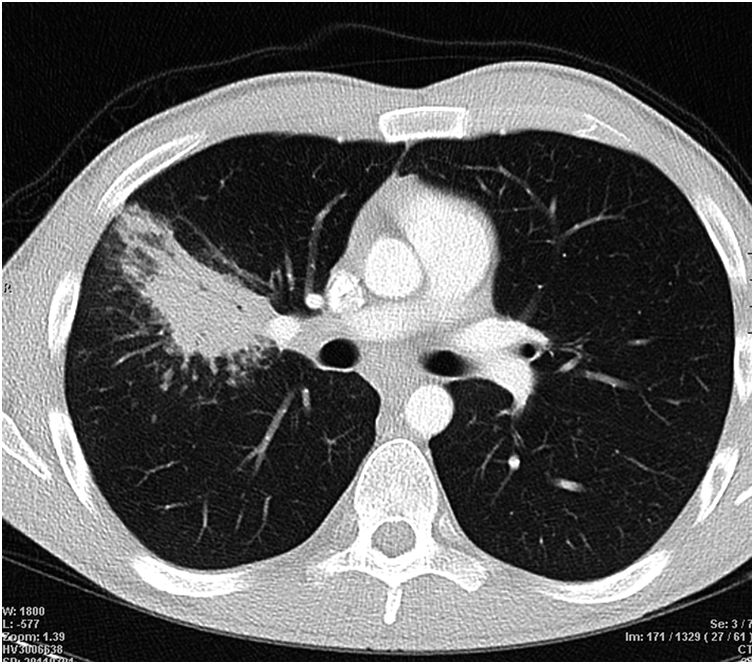
Computed axial tomography (CAT) of the chest and abdomen, which described multiple foci of pulmonary consolidation that could be of an infectious or inflammatory nature (Fig. 1) and a slight thickening of the wall of the terminal ileum with prestenotic dilatation.
Bronchoscopy with bronchoalveolar lavage (BAL) and transbronchial lung biopsy (TBLB), with no endoluminal lesions found. BAL microbiology: normal flora of the upper airways with negative cultures for Legionella, Gram, AFB and fungi. Transbronchial lung biopsy: thickening of the alveolar septum due to chronic inflammation and fibrosis. Alveoli thin-walled, without fibrosis or inflammation. The pneumocytes presented non-specific reactive changes. No granulomas or signs of malignancy were observed.
Colonoscopy, which revealed an ileocaecal valve with signs of inflammation and partial stenosis, exploring the last 3–4cm of the ileum where several ulcers with fibrin could be seen. Biopsies of the ileum were taken, finding non-specific inflammatory lesions.
All of the above was compatible with CD with involvement of the small intestine and upper digestive tract associated with a respiratory process compatible with bronchiolitis obliterans organizing pneumonia (BOOP).
Treatment was started with prednisone at a dose of 1mg/kg/day, in combination with azathioprine at a dose of 150mg/day with clinical, analytical and radiological improvement. As we were treating a young patient with gastric and small intestine involvement, three months later we decided to add treatment with adalimumab. From a respiratory point of view, the evolution was favourable, and a repeat chest x-ray at three months from starting corticosteroid treatment was normal.
The most common respiratory manifestations in IBD are those induced by the drugs used to control the disease (5-ASA, infliximab and methotrexate), so they often improve after suspending the medication.4
One of the diseases described within the pattern of parenchymal involvement is BOOP. There are few cases of this disease reported in the literature, it being more common in UC than in CD.2 It often manifests with fever, dyspnoea, general malaise and a cough. It is a non-specific inflammatory process that affects the lumen of the small airways and distal air spaces, with the presence in them of granulation connective tissue pseudopolyps.
The typical radiological findings are pulmonary consolidations and the ground-glass opacity pattern.5 Bronchoscopy is often normal in the majority of patients, and it is sometimes the transbronchial lung biopsy that enables us to reach a diagnosis.
The vast majority of patients with BOOP respond to treatment with corticosteroids, as occurred in our patient. The recommended regimen is 1–1.5mg/kg/day of oral prednisone for three months then gradual reduction of the dose over the following three months.
To conclude, it is important to keep all pulmonary manifestations in mind, both those induced by pharmacological treatments and those associated with the disease itself, in order to enable early diagnosis and treatment. To reach a diagnosis of BOOP, a bronchoscopy and a transbronchial lung biopsy must be performed. Most patients with BOOP have a good response to treatment with corticosteroids.
Please cite this article as: Cebrián García A, Ruiz-Clavijo D, Irisarri Garde R, González de la Higuera Carnicer B, García de Galdiano Fernández A, Fraile González M. Bronquiolitis obliterante con neumonía organizada en enfermedad de Crohn. Gastroenterol Hepatol. 2019;42:496–497.