Lymphocytic esophagitis (LyE) is a novel clinicopathological condition, first described in 2006 by Rubio et al. in Sweden,1 in a series of 20 patients as a histological subset of chronic esophagitis characterized by >20 intraepithelial lymphocytes (IELs) per high-power field (HPF) with no more than rare granulocytes. Since then, a number of case reports from all over the world have confirmed the identity of this new condition.2
We report two recent patients from our center meeting clinical and histopathologic criteria compatible with LyE.
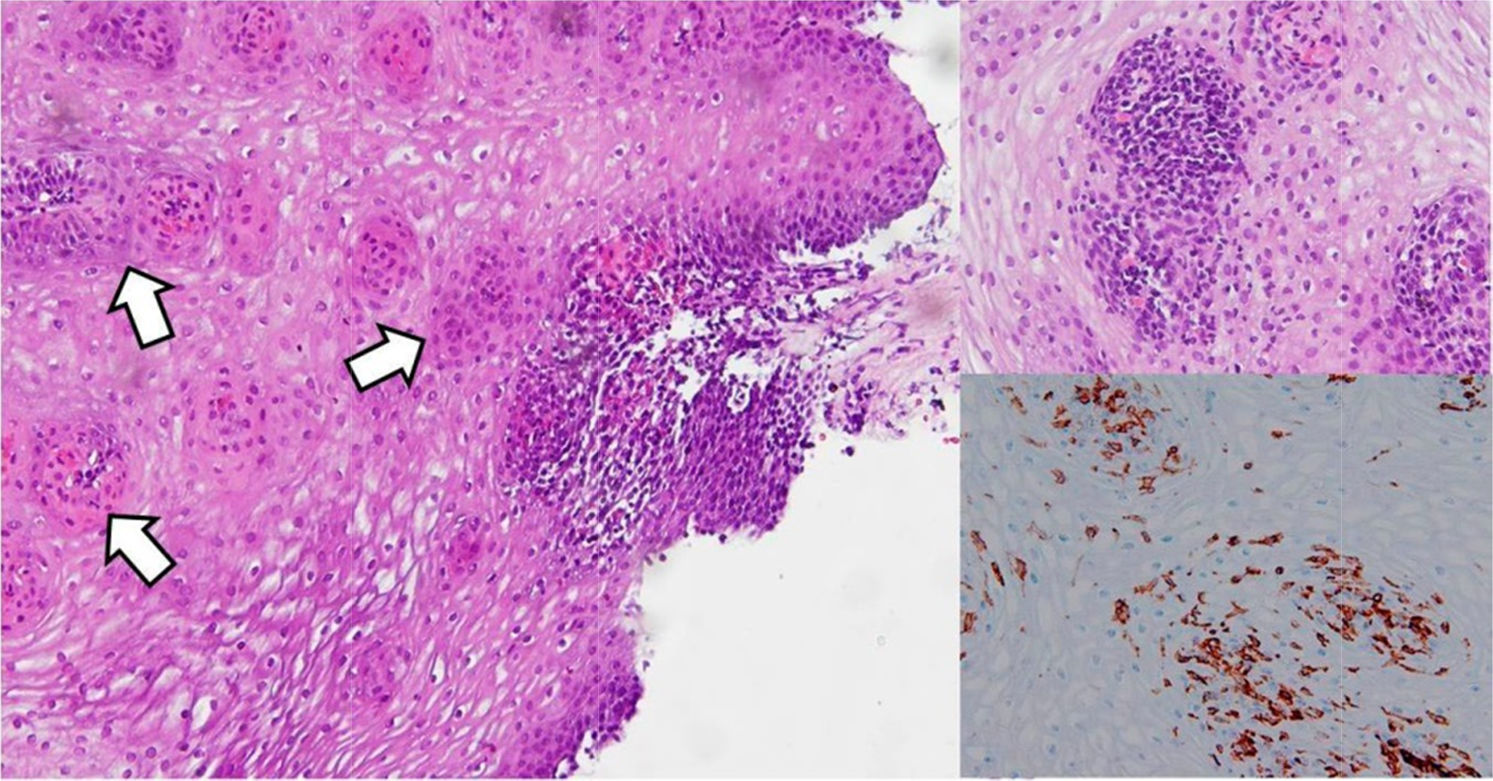
Case #1: A 52 yr-old male with smoking habit and a history of kidney stones presented with heartburn and non-progressive dysphagia over the past year. Upper endoscopy revealed no caliber or mucosal abnormalities and esophageal biopsies were taken to rule out eosinophilic esophagitis (EoE). Histopathologic analysis exhibited increased IELs increased (≥25/HPF) with marked basal–parabasal cell hyperplasia and intercellular edema (spongiosis). No eosinophils or neutrophils were detected (Fig. 1).
Left panel. Esophageal biopsy revealing heavy lymphocytic infiltration with papillar and peripapillar localization (white arrows) and intercellular edema (spongiosis), in the absence of either neutrophils or eosinophils. Right panel. A more detailed picture of lymphocytic infiltration, showing >25 CD4+ intraepithelial lymphocytes per 100 epithelial cells.
Case #2: A 63-year-old male with a history of hypertension, type 2 diabetes mellitus, ischemic cardiopathy and dyslipemia presented with recurrent esophageal food impaction requiring three emergency endoscopies. The patient denied previous heartburn and/or regurgitation. Esophageal endoscopic appearance was normal and esophageal biopsies revealed no eosinophilic but dense intraepithelial lymphocytosis (≥40/HPF) with papillar and peripapillar localization, and intercellular edema.
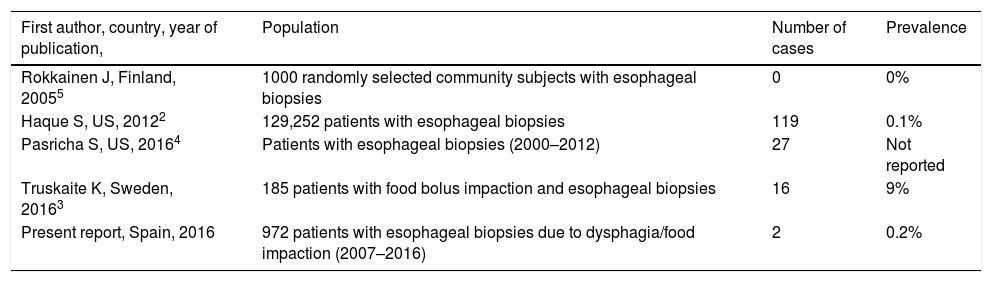
To the best of our knowledge, these LyE cases are the first reported in Spain. The prevalence of LyE has been reported to be 0.1% in patients with oesophageal biopsies,2 albeit a recent study from Sweden has reported that LyE might be present in up to 9% of patients with food impaction3 (Table 1). In our experience as a referral center for EoE over the past decade, we have only found two cases in 967 patients (0.2%) evaluated with esophageal biopsies due to dysphagia or food impaction (Table 1).
Updated prevalence rates of LyE in literature, including the present report.
| First author, country, year of publication, | Population | Number of cases | Prevalence |
|---|---|---|---|
| Rokkainen J, Finland, 20055 | 1000 randomly selected community subjects with esophageal biopsies | 0 | 0% |
| Haque S, US, 20122 | 129,252 patients with esophageal biopsies | 119 | 0.1% |
| Pasricha S, US, 20164 | Patients with esophageal biopsies (2000–2012) | 27 | Not reported |
| Truskaite K, Sweden, 20163 | 185 patients with food bolus impaction and esophageal biopsies | 16 | 9% |
| Present report, Spain, 2016 | 972 patients with esophageal biopsies due to dysphagia/food impaction (2007–2016) | 2 | 0.2% |
LyE is more common in older women without atopic conditions referring dysphagia, food impaction or gastro-esophageal reflux disease (GERD) symptoms.3,4 Association with Crohn's disease in children has shown discrepant results,6,7 whereas in adults it has been consistently associated with (GERD) and non-achalasia primary motility abnormalities.3,4,8 LyE has been proposed as an inflammatory non-specific response to different sources of esophageal injury, including radiofrequency ablation for Barrett's esophagus.9 Undoubtedly, LyE currently remains a histologic pattern in search of a disease.10 In our experience, consistent with most previous reports,2,5 it is still a rare finding (0.2%) in patients evaluated because of dysphagia or food impaction. Although this condition clinically and endoscopically may resemble EoE, the underlying etiology, its clinical significance and course, and best treatment remain to be ascertained in further studies.