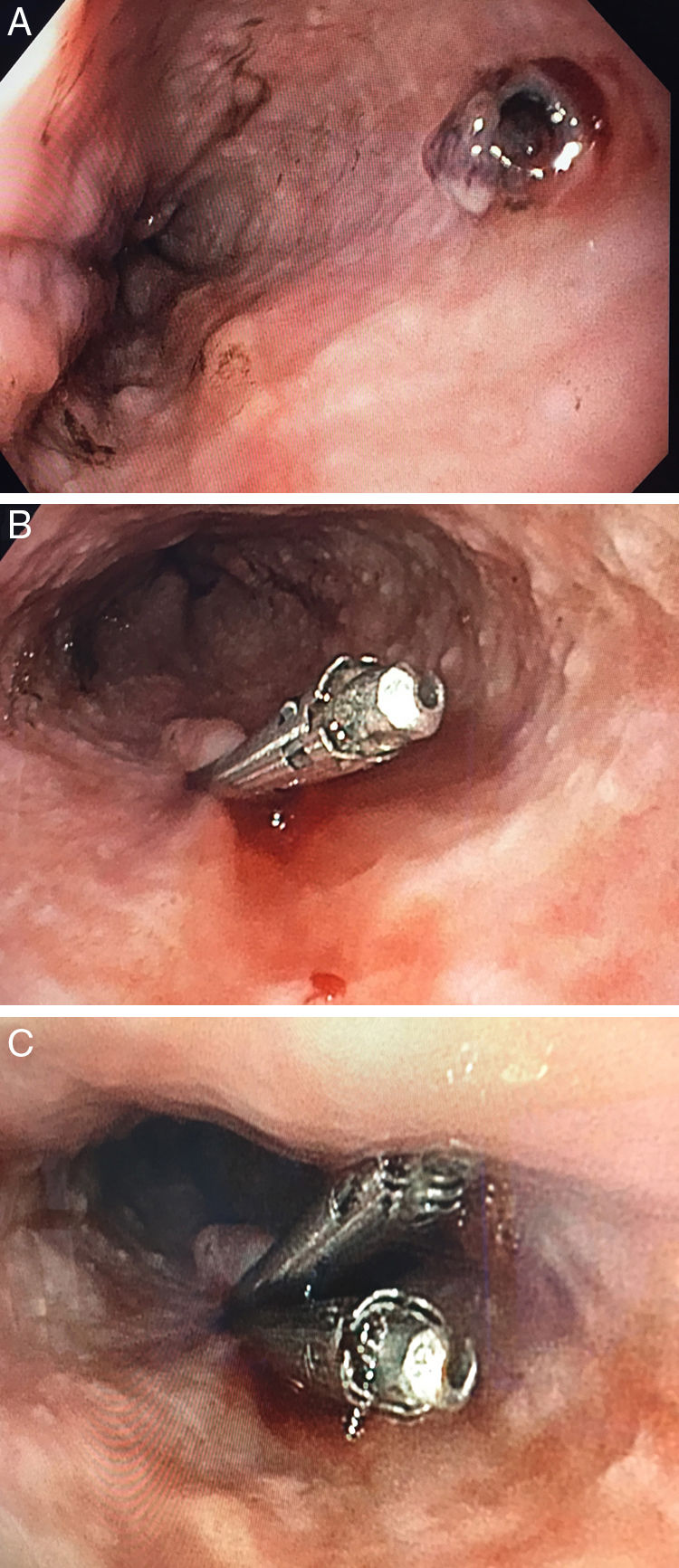
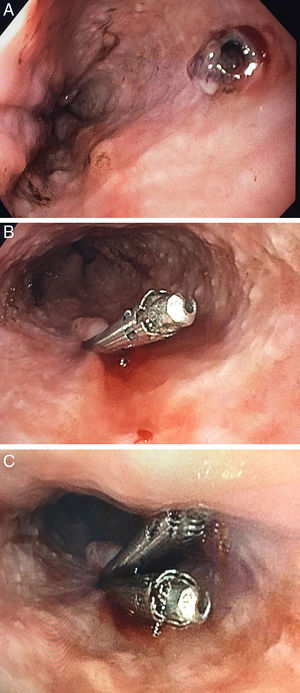
We present the case of a 63-year-old man with hypertension on drug treatment admitted for Fournier's gangrene. During the immediate postoperative period, the patient suffered massive haematemesis with hypotension. He developed severe anaemia, with haemoglobin levels down to 5.6g/dl, and had to be transferred to the intensive care unit. Emergency upper gastrointestinal endoscopy was performed, showing a large fresh clot occupying the lower half of the oesophagus and the gastric fundus. After thorough lavage and postural changes, pulsatile bleeding, probably arterial, was identified at the mid level of the oesophagus. The underlying mucosal lesion was not visualised. The injection of 6°cc of adrenaline at 1:10,000 stopped the bleeding, but it was not possible to accurately locate the culprit lesion because of the large amount of blood debris. The patient developed melaena with hypotension again 24h later and had to be started on vasoactive drugs. A further emergency upper gastrointestinal endoscopy was performed, with prior administration of prokinetics, and a visible vessel was detected in the mid oesophagus (Fig. 1A), with no abnormalities in the surrounding mucosa and no active bleeding compatible with Dieulafoy's lesion. Haemostasis was achieved by placing two Hemoclips® (Fig. 1B and C), with the effectiveness of the haemostasis being confirmed at the end of the procedure.
Dieulafoy's lesion is an uncommon finding, but extremely important clinically because it can cause massive gastrointestinal bleeding, destabilising the patient haemodynamically. It consists of an arterial vessel in the submucosa abnormally large for its location which protrudes into the mucosa through minimal weaknesses in continuity. It is important to stress that the surrounding mucosa is histologically normal and therefore differs from the vascular structures present in ulcerative niches. The pathophysiology remains unclear and the mechanisms by which these arterial vessels have not been subject to the decrease in physiological lumen to become blood capillaries or why they protrude through the mucosa are not fully understood. Histologically, neither aneurysmal dilations nor vasculitis have been found in the vessels responsible for the lesion. The lesion is most often located in the proximal stomach and diagnosis is a challenge because of the difficulty of visualisation, even more so with unusual locations like the oesophagus; 75–80% of the lesions are located in the stomach, with the majority concentrated in the 6cm distal to the oesophagogastric junction. The second most common location is the duodenum (up to 15%), half of them in the duodenal bulb. The remaining 5% are found in the colon or rectum. Other locations such as the ileum or oesophagus are considered incidental and only isolated cases or very small case series have been reported.1–4 In the oesophagus, we should further highlight the difficulty with diagnosis because of its particular anatomical features; it being a narrow space in which blood accumulates rapidly, hindering optimal examination of the entire surface of the mucosa. It is therefore sometimes necessary to perform repeated endoscopies before a definitive diagnosis can be made.
Its incidence is estimated at 0.1–1.5% of all gastrointestinal haemorrhages, and, only counting non-variceal upper gastrointestinal haemorrhages, Dieulafoy's lesion is responsible for 0.1–6%. In terms of demographic characteristics, the mean age is around 60, but cases of all ages have been reported. It predominantly affects males (69% vs. 31%) and there tends to be at least one associated comorbidity from the following list: structural heart disease, hypertension, chronic kidney disease and/or diabetes.5
Clinically, it usually manifests as painless, massive upper gastrointestinal bleeding, with up to 87% going into hypovolaemic shock. Diagnosing Dieulafoy's lesion is not an easy task. If the endoscopy is performed early, it may be possible to see the lesion actively bleeding. However, if the lesion is not bleeding at the time of endoscopy, as the surrounding mucosa is normal, it will probably not be found; in 20% of cases, a second endoscopy is required. Some measures, such as changing the patient's position or administering prokinetics prior to endoscopy, can facilitate visualisation. Angiography or a computed tomography angiogram can be used for diagnosis and even treatment when this is not possible endoscopically or when the patient is so unstable that endoscopy cannot be performed.6 The utility of endoscopic ultrasound has been suggested in selected cases, as it provides both diagnosis, identifying blood flow by applying the Doppler effect on the oesophageal mucosa, and the opportunity to apply targeted therapy.7
The main therapeutic approach is endoscopic, although debate persists about the best method for haemostasis. Because of the low prevalence of Dieulafoy lesions, there are no large randomised studies to provide evidence for a solid recommendation. Sclerotherapy and thermal methods of haemostasis used in monotherapy have been shown to be effective in achieving initial haemostasis, but with a high rate of rebleeding (33%) and potentially serious side effects such as perforation. There is now solid evidence showing that mechanical methods of haemostasis (Hemoclip® and rubber band ligation) are superior to sclerotherapy and thermal methods for the treatment of gastric Dieulafoy lesions, particularly in rebleeding situations. No differences have been found in haemostasis efficacy when comparing the two mechanical methods. However, rubber band ligation seems to achieve better control of rebleeding and can reduce the endoscopic procedure time.8,9 It is important to remember that management of oesophageal Dieulafoy lesions is complex because of the difficulty in manoeuvring the endoscope in the oesophagus, with the consequent increased risk of iatrogenic perforation.
In conclusion, Dieulafoy's lesion is a vascular disorder which can manifest as severe gastrointestinal bleeding. Although usually located in the stomach, there are other less common locations that must not be overlooked and which make it vital to carefully examine the entire surface of the mucosa during endoscopy. Making an accurate diagnosis is important because of the potential severity and high recurrence rate. Although there is no firm scientific evidence on the endoscopic method of choice, treatment with mechanical haemostasis methods (Hemoclip® and/or rubber band ligation) seems to be superior to the use of sclerotherapy or thermal methods.
Please cite this article as: Guerrero García A, Nuñez Gómez L, Crespo Pérez L, Mateos Muñoz B, de Teresa López ML, Albillos Martínez A. Dieulafoy esofágico: una causa infrecuente de hemorragia digestiva alta. Gastroenterol Hepatol. 2018;41:643–644.