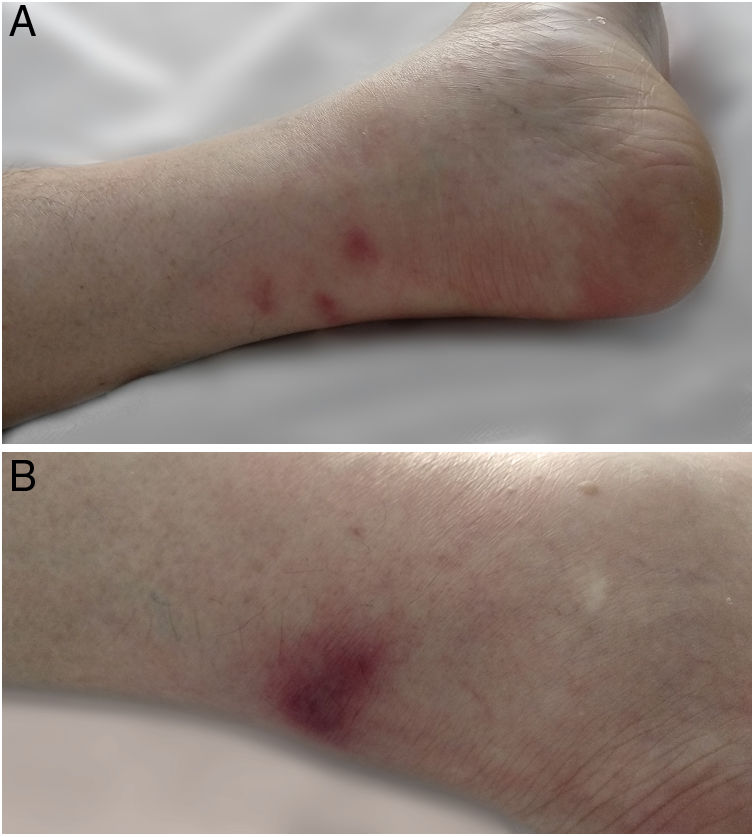
We present the case of an 82-year-old man admitted for abdominal pain. He had a 24h history of erythematous nodular lesions, painful to the touch, on the posterior-distal area of both legs (Fig. 1A and B). Histological study showed mixed panniculitis with lobular predominance and anucleated adipose cells; pancreatic panniculitis was diagnosed (Fig. 2A and B). After the patient's admission to hospital, imaging tests showed locally advanced pancreatic cancer infiltrating vascular structures. However, investigations were not completed due to the death of the patient.
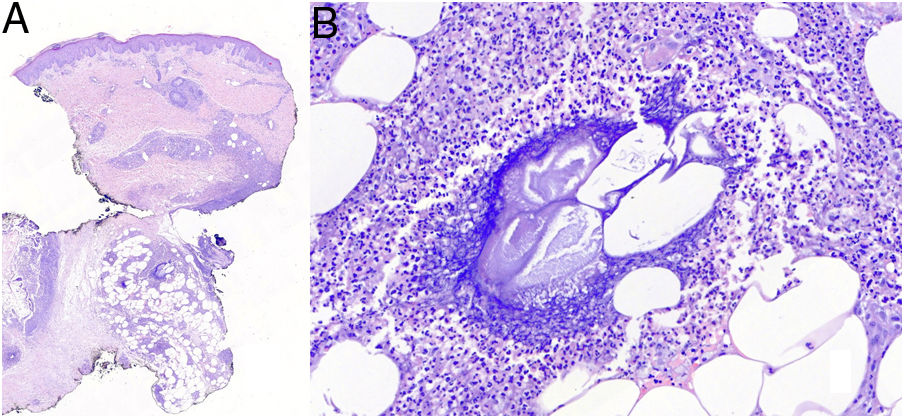
(A) Histopathological study of the lesion on the posterior aspect of the right leg. The image shows predominant involvement of the panniculus adiposus, with predominantly lobular panniculitis (H&E 1.9×). (B) Histopathological study of the lesion on the posterior aspect of the right leg at higher magnification. The image shows the presence of “ghost areas” with anucleated adipose cells intermingled with amorphous granular tissue with intense basophilia (H&E 24.5×).
Pancreatic panniculitis is an uncommon complication associated with disease of the pancreas (2–3%).1 Clinically, it appears as erythematous, oedematous nodules, painful on palpation, which can ulcerate and are often located on the posterior aspect of the leg (usually perimalleolar).2 Diagnosis is established by skin biopsy; mixed panniculitis with lobular predominance is observed, where the adipocytes lose their nuclei, becoming so-called ghost cells, and these cells then become surrounded by granular basophilic material.1 Panniculitis is the first sign of pancreatic disease in 30–40% of cases, increasing to 68% if associated with pancreatic carcinoma.3 We therefore consider that clinically recognising this finding may be essential for the early detection of occult pancreatic carcinoma.
Please cite this article as: de la Torre Gomar FJ, Heras González S, Pérez Rodríguez Á, Sáenz Aguirre A, Martínez de Lagrán Álvarez de Arcaya Z. Paniculitis pancreática como forma de presentación de neoplasia localmente avanzada. Gastroenterol Hepatol. 2020;43:325–326.