Oesophageal pH-monitoring allows the quantification of gastric reflux episodes in patients with gastroesophageal reflux disease (GERD). The accuracy of the test depends on correct positioning of the pH sensor 5cm above the lower oesophageal sphincter (LES). The most precise manner to locate the LES is through prior determination by oesophageal manometry. However, because this technique is uncomfortable, mathematical formulas tend to be used in children.
ObjectivesTo evaluate the applicability of paediatric formulas to estimate oesophageal length in adults and their effect on diagnostic accuracy.
Material and methodsA prospective study was carried out in adult patients, in whom the distance between the nasal orifice and the LES was determined by manometry and was compared with the estimated height-related distance calculated by four paediatric formulas (numbered 1–4). We also evaluated the relationship between the position of the probe and the percentage of reflux detected in our series of impedance measurements.
ResultsFormula 1 (9.31+height in cm×0.197) was the most accurate (comparison of means −0.38 with 95% CI −0.70/−0.06, p=0.019). With this formula, none of the patients had estimation errors of ±6cm. With formulas 2, 3 and 4, the percentage of error was 4.4%, 1.5% and 32.0%, respectively.
ConclusionOesophageal length estimation in adults by using formula 1 is acceptable and can be used in adult patients who refuse to undergo prior manometry.
La pHmetría esofágica permite cuantificar los episodios de reflujo ácido en pacientes con enfermedad por reflujo gastroesofágico (ERGE). El posicionamiento adecuado del electrodo de pH a 5cm por encima del esfínter esofágico inferior (EEI), determina la precisión de la prueba. La manera más exacta para localizar el EEI es mediante su determinación previa por manometría esofágica, pero es una técnica molesta, por lo que en niños tendemos a utilizar fórmulas matemáticas.
ObjetivosValorar la aplicabilidad de las fórmulas pediátricas de estimación de longitud esofágica en pacientes adultos y su repercusión en la precisión diagnóstica.
Material y métodosEstudio prospectivo en pacientes adultos en el que la distancia desde el borde de la narina hasta el EEI determinada por manometría se ha comparado con la distancia estimada en relación a la talla calculada por 4 fórmulas pediátricas (numeradas del 1 al 4). También hemos valorado la relación entre posición de la sonda y porcentaje de reflujos detectados en nuestra serie de impedanciometría.
ResultadosLa fórmula 1 (9,31+talla cm×0,197) fue la más precisa (comparación de medias −0,38 con IC95% −0,70 a −0,06, p=0,019). Con dicha fórmula, ningún paciente presentó errores de estimación de±6cm. Con las fórmulas 2, 3 y 4 el porcentaje de error fue del 4,4, del 1,5 y del 32,0%, respectivamente.
ConclusiónLa estimación de la longitud del esófago en adultos mediante la fórmula 1 es aceptable y puede usarse en casos en los que el paciente rechace la realización de una manometría previa.
Oesophageal pH monitoring is the method of choice for quantifying episodes of gastric reflux in patients with gastro-oesophageal reflux disease (GERD). Probe placement is important and determines the sensitivity of the test, because the number of reflux episodes detected decreases the further away the probe is from the lower oesophageal sphincter (LES).1 The pH electrode of the probe is generally placed 5cm above the LES to prevent it from entering the stomach during the test due to patient movements, while at the same time detecting all episodes of acid reflux. Oesophageal manometry is used in adults for accurate localisation of the LES prior to placement of the pH catheter.2,3 Manometry is an uncomfortable test that requires patient collaboration, and as such tends to be avoided in children, in whom the distance is calculated using arithmetic formulae that correlate height with oesophageal length.4–6 These formulae can be calculated rapidly and do not require additional resources or patient collaboration, but they are subject to errors that can invalidate the pH or impedance test.6–8
Oesophageal intraluminal impedance testing, meanwhile, provides a study of reflux episodes at different levels of the oesophagus,8 thus providing an exact idea of the percentage of episodes that are not detected as a result of a poorly positioned probe.
Our aim was to assess the accuracy of formulae used to calculate naso-oesophageal catheter placement, as well as the loss of information that a placement error could entail.
Materials and methodsA prospective, descriptive study was conducted in a group of adult patients with suspected GERD who first underwent 4-channel perfusion oesophageal manometry followed by pH testing using the Synectics Medical (Medtronic, MN, USA) and Ohmega systems (Medical Measurement Systems [MMS], NH, USA), respectively. The pH catheter used was the S21-*, also from MMS.
The length from the nares to the upper border of the LES determined by manometry was compared with the length estimated using paediatric formulae that related this distance with the height. Formula 1 (9.31+height in cm×0.197) has been used per protocol in our hospital for the last 15 years. It is the result of our own modification of formula 2 to achieve greater accuracy (unpublished data).
Formula 2 (9.31+height in cm×0.179) is the formula used in Hospital Infantil Vall d’Hebron in Barcelona (Spain), and is based on studies conducted in the hospital in the 1970s and 1980s.
Formulas 3 (6.7+height in cm×0.226) and 4 (5+height in cm×0.252) are those reported by Strobel, taking as the origin the mouth or nares, respectively.4
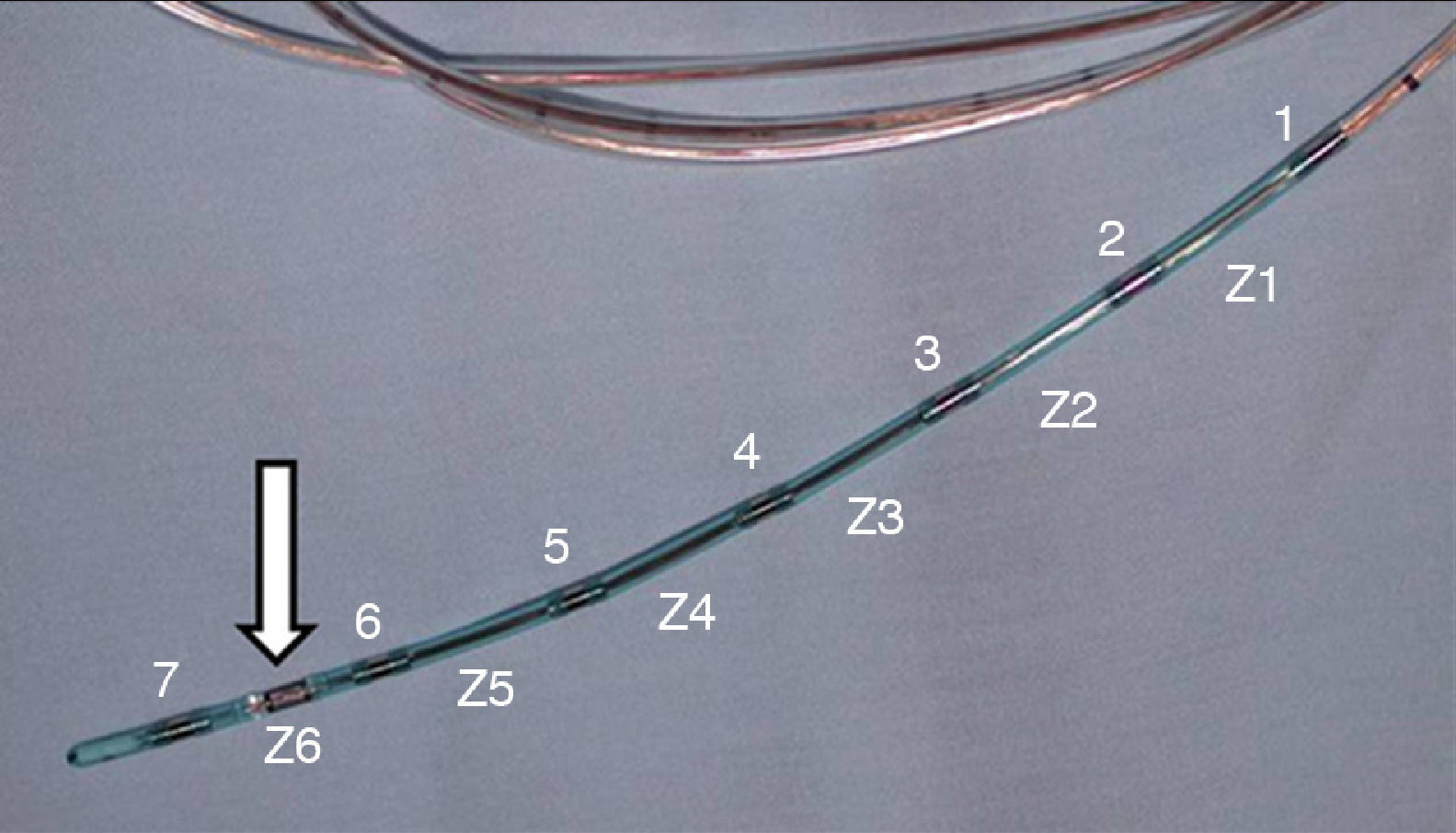
In order to assess the percentage of reflux episodes that might be lost the further away the probe is placed from the optimal position, we analysed the results of our paediatric impedance-pH monitoring series. The impedance catheter used was the K6011-EI-0636 (MMS), with 1 pH electrode and 6 impedance channels. The characteristics of the gastro-oesophageal episodes (acidic, non-acidic or weakly acidic) were not assessed, nor were results between children and adults compared.
The information was noted in each patient's medical record following the hospital's restricted access protocols and was processed using SPSS statistical software. The qualitative variables are described with categorical frequency distribution, and the quantitative variables with mean and standard deviation. A formula for calculating the length from the nares to the superior border of the LES was obtained from data from the sample using simple linear regression, where the dependent variable is the distance determined by manometry and the independent variable is the height. The correlation of the measurements calculated using the paediatric formulae with the length determined by manometry was studied using Pearson or Spearman correlation coefficients, depending on whether or not the variables followed a normal distribution. The level of statistical significance was accepted as 5% (p<0.05).
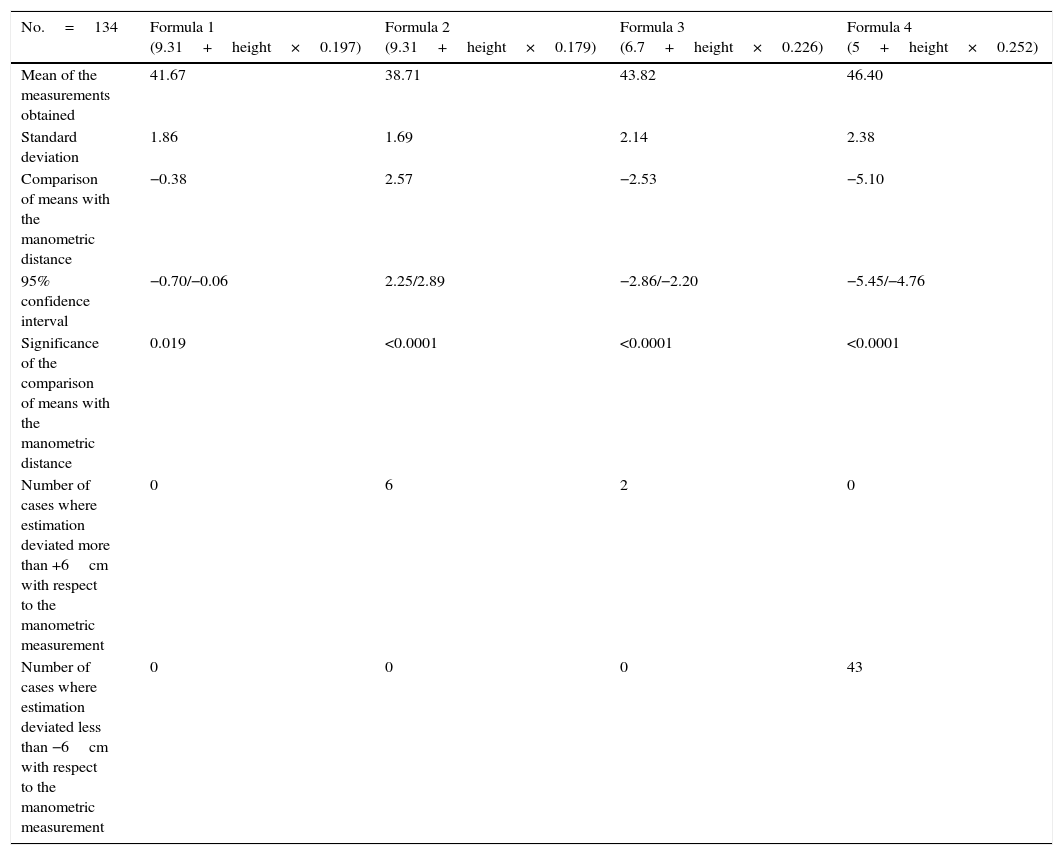
ResultsA total of 134 patients (48 men and 86 women) with heights between 162.00 and 196.00cm (χ¯: 174.03, Me: 173.50 and S: 6.30) and between 147.00 and 173.00cm (χ¯: 158.84, Me: 159.00 and S: 5.90), respectively, were studied. The distance from the nares to the LES determined by manometry ranged from 39.00 to 47.00cm in men (χ¯: 43.11, Me: 43.00 and S: 1.90) and from 35 to 45cm in women (χ¯: 40.27, Me: 40.00 and S: 2.07). Overall, heights ranged from 147 to 196cm (χ¯: 164.28, Me: 156.5 and S: 9.47) and the distances from the nares to the LES determined by manometry from 35 to 47cm (χ¯: 41.29, Me: 40 and S: 2.43). Table 1 shows the data obtained after applying the paediatric formulae analysed, with height as variable (sex was not considered as a conditioning variable in the study).
Distances from the nares to the lower oesophageal sphincter using the height-related paediatric formulae analysed.
| No.=134 | Formula 1 (9.31+height×0.197) | Formula 2 (9.31+height×0.179) | Formula 3 (6.7+height×0.226) | Formula 4 (5+height×0.252) |
|---|---|---|---|---|
| Mean of the measurements obtained | 41.67 | 38.71 | 43.82 | 46.40 |
| Standard deviation | 1.86 | 1.69 | 2.14 | 2.38 |
| Comparison of means with the manometric distance | −0.38 | 2.57 | −2.53 | −5.10 |
| 95% confidence interval | −0.70/−0.06 | 2.25/2.89 | −2.86/−2.20 | −5.45/−4.76 |
| Significance of the comparison of means with the manometric distance | 0.019 | <0.0001 | <0.0001 | <0.0001 |
| Number of cases where estimation deviated more than +6cm with respect to the manometric measurement | 0 | 6 | 2 | 0 |
| Number of cases where estimation deviated less than −6cm with respect to the manometric measurement | 0 | 0 | 0 | 43 |
The following formula was constructed based on our measurements of the distance from the nares to the LES by manometry in our adult group: distance from nares to LES=14.059+height in cm×0.166 (correlation 0.551 and p<0.001).
On analysing the data from the paediatric impedance series, it was noted that if the distal channel of the impedance catheter (Z6) detects 100% of the reflux episodes, the second channel (Z5) detects a mean of 99.5% and the third (Z4) detects a mean of 90.68% of reflux episodes.
DiscussionThe medical literature contains numerous mathematical formulae that estimate the length of the oesophagus by correlating it with the height of the individual.4–6,9 The ultimate aim of all these studies is to find a formula that can reliably predict the length of the oesophagus based on the height of the individual, thereby avoiding oesophageal manometry in order to correctly position the pH electrode.
The Strobel4 and Staiano5 formulae are widely known and commonly used, but numerous authors have resorted to personal patient series to establish their own formulae.6 Other variables, such as weight and age have even been added to improve the precision of the calculation.9
Some authors prefer to check the position radiologically, ensuring that the probe electrode is at the level of the second vertebra above the diaphragm.10,11
We have used formula 1, described above, for the last 15years in our hospital. It is very similar to formula 2, but in our opinion is more accurate. The third and fourth formulae studied are those of Strobel,4 which are probably the most widely accepted in the paediatric field.
Our results vary slightly from those described by other authors,5 in the sense that, as the height increases–even though there is a significant correlation between this and the oesophageal length (p<0.0001)–the margin of error is significant in a considerable percentage of cases (Table 1).
Notably, distances obtained from the formula used in our hospital (formula 1) are closest to the results obtained by manometry. None of the patients presented oesophageal length estimation errors greater than ±6cm.
The extent to which poor positioning of the pH probe affected the accuracy of the test is unclear, and we cannot be certain how many reflux episodes were not detected when the probe was poorly placed. We believe that impedance testing (regardless of the patient's age) can provide valuable data that correlate the positioning error with the accuracy of the test.
For this reason, we used our paediatric impedance series. The catheter used has 7 impedance sensors (which determine study channels called Z1 to Z6 from the most proximal to the most distal) and 1 pH sensor. In the catheter chosen, the sensors are situated at 2cm intervals from the distal end, so that the number of reflux episodes (acidic, weakly acidic and non-acidic) detected in each can be determined (Fig. 1).
At 4cm above the tip of the catheter (between the penultimate and third last sensor, which define the Z5 channel), 99.5% of reflux episodes were detected with respect to those detected in Z6, and at 6cm from the tip (channel Z4), 90.68% of episodes were detected. The greater the distance from the distal oesophagus, the more the proximal extent of the reflux gradually decreased. Logically, this finding should be interpreted with caution, since most patients undergoing impedance monitoring are diagnosed with GERD. As such, they are not healthy individuals and are more likely to present abnormalities in oesophageal length (hiatus hernias) and motility that contribute to the proximal extent of the reflux and increase the percentage of episodes detected in the proximal sensors. Even the oesophageal length appears to vary depending on the predominant symptoms of the GERD.12
Our paediatric impedance series includes a wide age range, from one-month premature babies with a body length of 35cm to adolescents with a height of 195cm. This comprises a huge range of distances to the LES, and therefore tests the mathematical formulae more thoroughly than a series of adults with a far more homogeneous height range would do. This is why we consider the loss of information regarding the distance from the LES measured by manometry evidenced by impedance findings to be so important, and why we consider the contribution of impedance to this study, albeit not essential, to be so significant.
ConclusionsIn order to determine the placement of a pH probe in adults, the paediatric formula employed in our hospital can be used, and can replace oesophageal manometry in cases where it cannot be tolerated.
Conflict of interestsThe authors declare that they have no conflict of interests.
Please cite this article as: Molina Caballero AY, Villar Varela ME, Pérez Martínez A, Ayuso González L, Hernández Martín S, Goñi Orayen C. Colocación de sondas de pHmetría mediante fórmula relacionada con la talla. ¿Es un método aplicable a los adultos? Gastroenterol Hepatol. 2016;39:261–264.