Haemangioma is the most common benign liver tumour, with a prevalence of 20% in the population. They behave as solitary nodules, usually asymptomatic and smaller than 5cm in size, although rarely they can be larger, become associated with consumptive coagulopathy (Kasabach–Merritt syndrome) or be diffuse, affecting the whole liver.
We report the case of a patient with multiple hepatic haemangiomas (hepatic haemangiomatosis) (HH) with replacement of the liver parenchyma causing portal hypertension and its associated complications.
This was a 46-year-old man with no relevant history who came to the emergency department with abdominal distension, with giant rock-hard hepatomegaly and abdominal collateral circulation found on examination. Blood tests showed abnormal liver function, predominantly cholestatic, with normal bilirubin, albumin and platelets, and mild coagulation abnormalities. Alpha-foetoprotein levels were within normal range. Liver function tests (virus serology, autoimmunity and metabolic disorders) showed no abnormalities, and there was no evidence of previous ingestion of drugs or toxic substances.
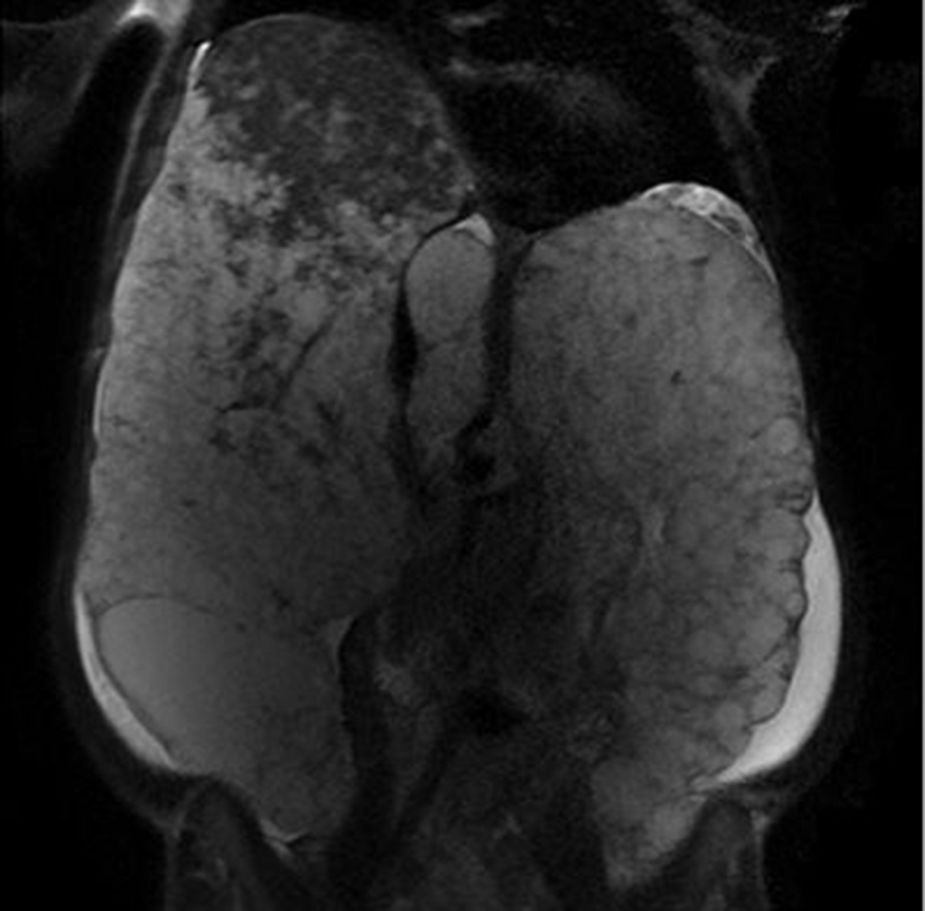
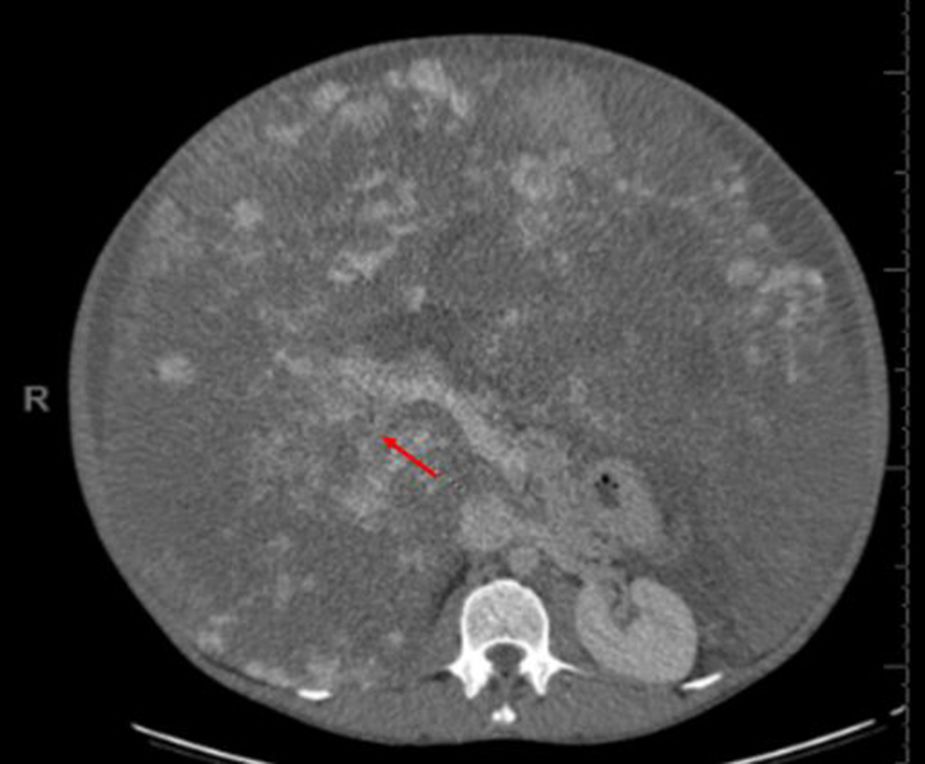
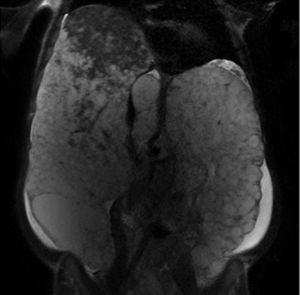
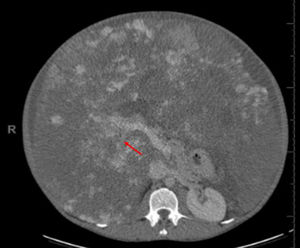
The initial abdominal ultrasound revealed giant hepatomegaly taking up almost the entire abdomen, with a very heterogeneous structure and countless space-occupying lesions suggestive of angiomatosis, which were confirmed by contrast ultrasound, magnetic resonance imaging and abdominal CT. The CT scan also showed vascular compression of the portal branches, intrahepatic cava and left suprahepatic, although they remained patent, with venous bypass through the azygos system, and a normal spleen. The diagnostic process was completed with Tc-99m red blood cell and colloid scintigraphy, which showed de-structured parenchyma and a pattern of uptake highly specific to HH lesions. Paracentesis was performed and ascitic fluid was found to have a serum-to-ascites albumin gradient of 1.1. Gastroscopy showed portal hypertensive gastropathy with no oesophageal varices. Given the highly specific radiological findings of HH occupying virtually all of the liver parenchyma, no liver biopsy was performed because of the complexity of the technique and the risk of causing further damage.
The patient's clinical progress was slow; the ascites was difficult to control and he developed spontaneous bacterial peritonitis. He is currently being assessed for liver transplantation, with diagnoses of HH with replacement of liver tissue and development of PH, and Child–Turcotte–Pugh grade B7 and Model for End Stage Liver Disease (MELD) 10 liver failure (Figs. 1 and 2).
Hepatic haemangiomas are the most common benign tumours of the liver, with very low likelihood of malignancy. They usually occur in young women, in the form of single small lesions. If larger than 5cm or if the involvement is diffuse, they can be accompanied by symptoms such as pain in the upper abdomen, nausea and early satiety; or cause complications such as rupture of the haemangioma and compression or thrombosis of adjacent structures.1–3
PH is a seldom reported consequence of haemangiomas and has generally been related to the physical compression of the portal vein in giant lesions, with portal vein thrombosis also a risk.4 In our patient, the development of PH and its consequences was associated not only with the mechanical compression of vascular structures, but also the replacement of the liver tissue, leading to secondary liver failure.
The diagnosis of hepatic haemangiomas is often made incidentally, when performing imaging tests such as abdominal ultrasound. However, because of their low specificity they have to be confirmed by CT or MRI.4 Other techniques such as contrast ultrasound, scintigraphy with Tc-99m-labelled red blood cells or angiography may be necessary in exceptional cases.1–3,5
In terms of management, monitoring small-sized haemangiomas is not necessary in patients with a low risk of malignancy who do not have chronic liver disease or evidence of malignant extrahepatic disease.2 Radiological follow-up yearly or every two years is recommended in asymptomatic large haemangiomas, pregnant women and patients on oestrogen hormone therapy.2,6,7
Results following medical treatment with beta-blockers or monoclonal antibodies such as bevacizumab (anti-VEGF) have been inconclusive, although satisfactory outcomes have been reported in paediatric patients.6 Other techniques such as radiotherapy, radiofrequency or transarterial embolisation have been used in patients with high surgical risk, or to decrease the size of the lesion or increase the residual liver parenchyma prior to surgery.6
Surgery should be the treatment of choice in cases of rapid growth, persistent clinical signs, localised risk or complications (thrombosis, rupture or bleeding). The intervention most recommended is enucleation, except in deep or large lesions, when liver resection should be considered.7,8
There are cases in the literature of liver transplantation in giant haemangiomas, haemorrhage due to rupture of the haemangioma (incidence 1–4%) and Kasabach–Merritt syndrome.9 In the study published by Ercolani et al., up to 2010, only 12 cases of liver transplantation had been recorded in the United Kingdom in patients with HH, most of them resulting from Kasabach–Merritt syndrome and its complications.9 However, the indication for liver transplantation due to terminal liver failure and/or development of complications induced by portal hypertension secondary to HH, as in our case, is completely exceptional.10
Please cite this article as: Hidalgo Romero Á, Gómez Domínguez E, Muñoz Gómez R, Muñoz Codoceo C, Fernández Vázquez I. Hipertensión portal secundaria a hemangiomatosis hepática múltiple. Gastroenterol Hepatol. 2018;41:323–324.