Hydatidosis is a zoonosis caused by Echinococcus.
This parasite lives in the intestines of dogs. Humans act as an intermediate host. In the intestine, the eggs release oncospheres, which cross through the intestinal mucosa and, through the portal circulation, reach the liver, affecting it in 75% of cases.1 Many of these hepatic cysts maintain a state of agent/host equilibrium, with the patient remaining asymptomatic, and they are detected incidentally in imaging tests.2
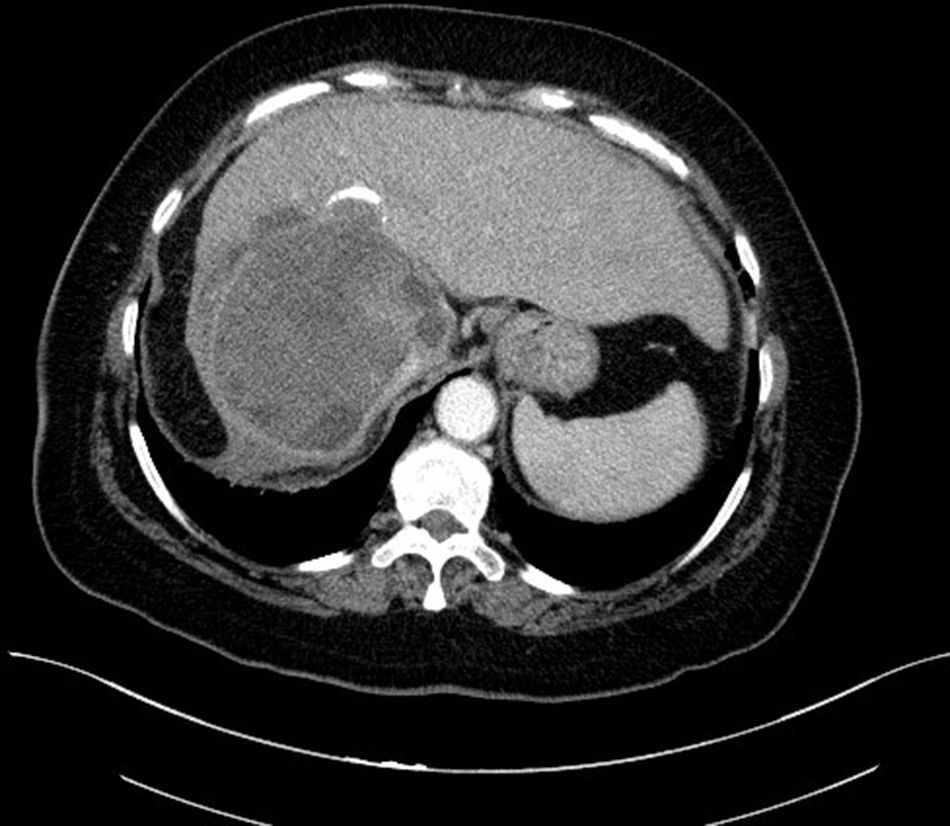
Case reportThis was a 68-year-old woman who worked as a cattle farmer in the rural area of Salamanca. She consulted with a two-week history of right upper quadrant pain. She had no jaundice or choluria, pyrexia, skin rashes, pruritus or other relevant symptoms. Blood tests showed total bilirubin 1.40mg/dl, GPT 138IU/l and CRP 101mg/ml, with normal procalcitonin and no leucocytosis, eosinophilia or coagulation disorder detected. A computed tomography (CT) scan of the abdomen and pelvis revealed a large multilocular cystic lesion occupying liver segments VI, VII and VIII, with maximum diameters of 10×8cm, with small locules in the periphery suggestive of rupture of the hydatid cyst (Fig. 1). The patient was immediately started on treatment with oral albendazole 15mg/kg/day and was assessed by the surgical team, opting for priority elective surgery.
During the surgical intervention the hydatid cyst with calcified wall was identified surrounding the right portal pedicle and the right suprahepatic vein on its interior/posterior side, with this being confirmed by intraoperative ultrasound. With the aim of eradicating the echinococcus, hyperosmolar saline was instilled, aspirating the contents of the cyst to avoid hyperpressure, repeating this procedure several times until the absence of vesicles was verified. Contact with the great vessels increases the complexity of the surgery, so instead of pericystectomy (radical treatment) it was decided to de-roof and resect the anterior aspect of the cyst (corresponding to liver segments V, VI, VII and VIII), leaving the inner side in contact with the great vessels.
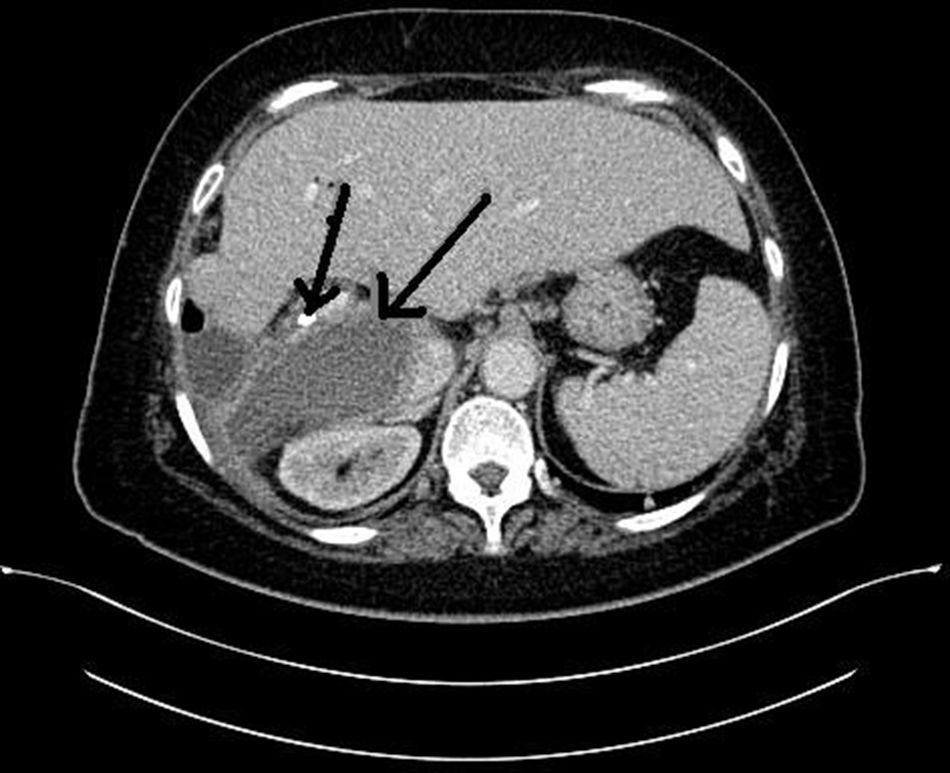
In the immediate postoperative period, due to output of bile in drain, biliary fistula was suspected. An endoscopic retrograde cholangiopancreatography (ERCP) was performed, detecting a bile leak in the right side of the liver (section surface); a 12cm-long 10F plastic prosthesis was inserted, with distal end in the duodenum (Fig. 2).
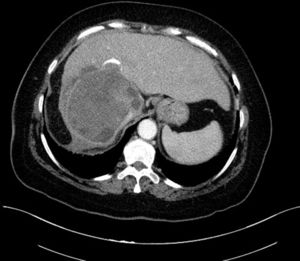
The patient made a good recovery, completing a one-month course of antiparasitic treatment. The follow-up CT scan one and a half months after discharge showed a small collection adjacent to the prosthesis (Fig. 3), but, as the patient was asymptomatic and afebrile, it was decided to take a “watch and wait” approach.
DiscussionAmong the complications of hepatic hydatid disease are fistulisation or rupture into the peritoneal or pleural cavity. This can lead to both the spread of the infection and anaphylactic reactions.
The WHO/IWGE (World Health Organisation Informal Working Group on Echinococcosis)3 classification is the most used and differentiates the lesions found in the abdominal ultrasound, being very useful for establishing the best treatment: CL (active, cystic lesion without wall); CE1 (active, lesion with wall and stones); CE2 (active, multivesicular lesion with daughter cysts); CE3 (transitional, unilocular lesion with detachment of the laminar membrane); CE4 (inactive, heterogeneous lesion without daughter cysts); CE5 (wall calcification).
The therapeutic indication also depends on the morphological classification, the location in the liver, its relationship with large vessels and the risk of rupture.
We should also mention the difficulty with the clinical-radiological correlation and the lack of correspondence between calcification and sterile cyst, as calcification does not correlate with activity.4
The treatment is based on four main options depending on the characteristics of the cyst: surgery, percutaneous drainage, antiparasitic agents or “watch and wait” strategy (follow-up with periodic ultrasound).5
Surgery is essential for large cysts (CE2-CE3 with multiple daughter cysts), complicated cysts (ruptured, fistulised, infected, etc.) or cysts at risk of rupturing. In all cases, treatment with oral albendazole is administered from one week before surgery to four weeks after.6
One option is to perform complete resection or pericystectomy. The other option is partial cystectomy, sterilising the cyst with hypertonic saline prior to extraction. It is important to remember that when the hydatid cyst communicates with the bile duct, the instillation of corrosive agents can cause caustic sclerosing cholangitis. Therefore, for large cysts, it is advisable to perform a preoperative MRI (magnetic resonance imaging) cholangiogram or intraoperative cholangiogram.
Please cite this article as: Prieto Elordui J, Heras Martin JI, Gómez García P, Blanco Sampascual S, Cabezudo Gil P, Erdozain Larrañaga I, et al. Dolor en hipocondrio derecho como manifestación de rotura contenida de quiste hidatídico hepático: abordaje terapéutico. Gastroenterol Hepatol. 2019;42:310–311.