Abdominal paracentesis is an area that every general physician should know about, and the current learning model is unsafe for patients. Simulation allows students to develop their skills prior to clinical confrontation with minimal risks. The aims of this study were to design and evaluate a paracentesis simulation workshop for undergraduate students.
MethodsA workshop was implemented using a specially designed and validated simulation model for abdominal paracentesis. The simulated technique considered the recognition of materials, operator equipment, asepsis, anesthesia, puncture and obtaining liquid, collecting samples for analysis, withdrawal of the material and occlusion. A 24-point direct observation checklist was administered to assess the student. We assessed two students at the beginning of the workshop and all the students at the end. A perception survey was applied to attendees at the end of the workshop.
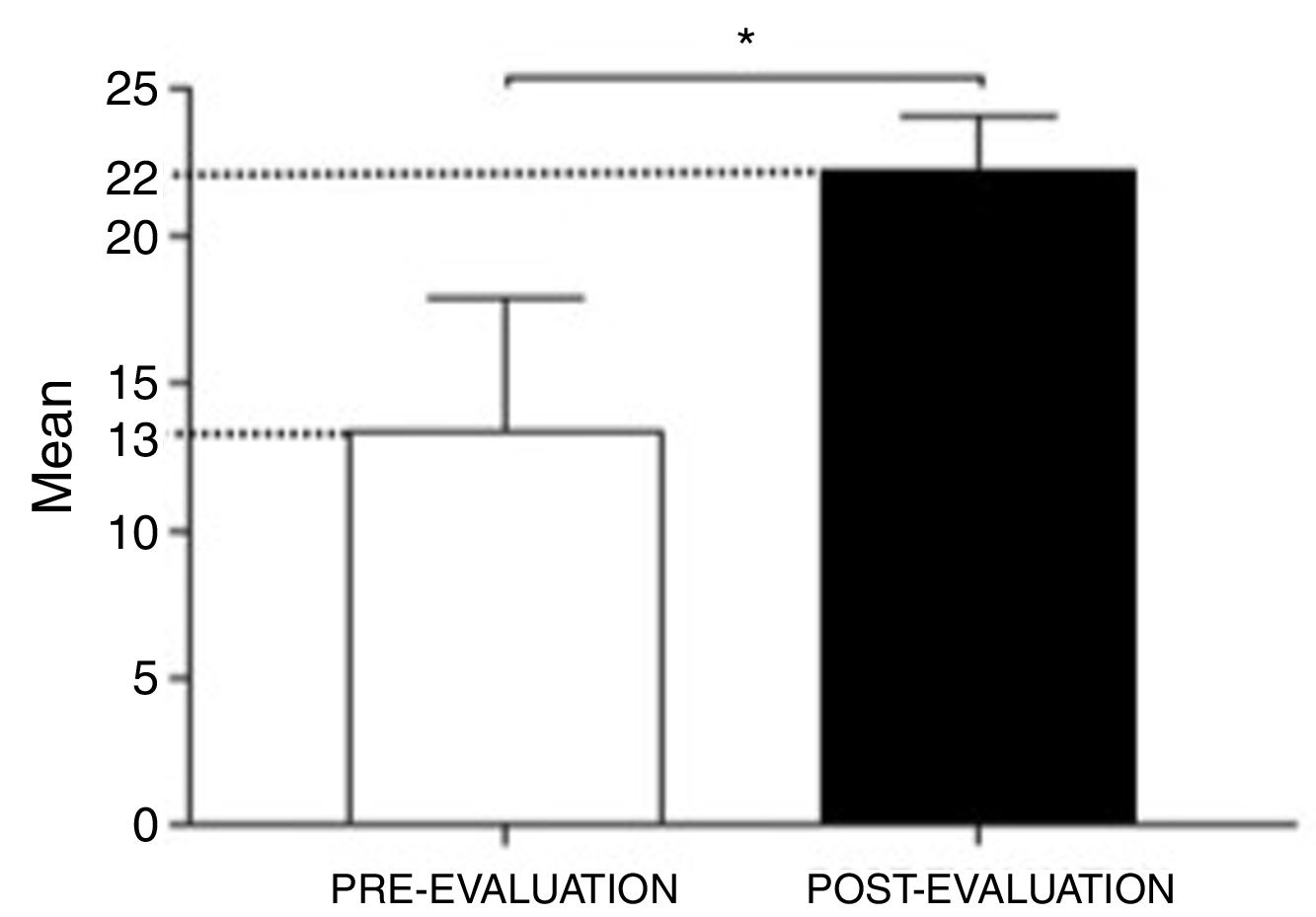
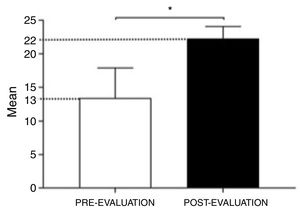
Results247 students were included and a workshop that involved 8 students per session was held. Students significantly improved their skills comparing pre- and post-evaluation results [13.36±4.46 (55.7%) vs. 22.3±1.83 (92.9%) respectively (n=69) p<0.001]. The students’ perception questionnaire (n=38) showed that the training sessions were highly valued, averaging 4.8±0.38 on a Likert scale of 1–5.
ConclusionsSimulated training in abdominal paracentesis is a very good teaching method. This teaching methodology should be highly recommended as an educational strategy in medicine because it could accelerate the acquisition of clinical skills in a safe learning environment.
La paracentesis abdominal es una competencia que todo médico general debe conocer, y el modelo de aprendizaje actual no es seguro para los pacientes. La simulación permite a los estudiantes desarrollar habilidades antes del enfrentamiento clínico minimizando riesgos. Los objetivos de este estudio han sido diseñar y evaluar un taller de simulación de paracentesis para estudiantes de pregrado.
MétodosSe implementó un taller de paracentesis abdominal, utilizando un fantoma especialmente diseñado y validado. La enseñanza de la técnica consideró el reconocimiento de materiales, equipo del operador, asepsia, anestesia, punción y obtención de líquido, recolección de muestras para análisis, extracción del material y oclusión. Para la evaluación se usó una pauta de observación directa (24 puntos). Dos estudiantes por grupo fueron evaluados al comienzo del taller y todos los alumnos se evaluaron al final. Al término del taller se aplicó una encuesta de percepción a los asistentes.
ResultadosSe incluyeron 247 estudiantes en un taller que involucraba 8 alumnos por sesión. Los estudiantes mejoraron significativamente sus habilidades al comparar los resultados de la pre-evaluación versus la postevaluación (13,36±4,46 [55,7%] vs. 22,3±1,83 [92,9%], respectivamente [n=69]; p<0,001]. El cuestionario de percepción de los estudiantes (n=38) demostró que las sesiones de entrenamiento fueron valoradas positivamente, con un promedio de 4,8±0,38 en la escala de Likert de 1-5.
ConclusionesEl entrenamiento simulado en paracentesis es un muy buen método de enseñanza. Esta metodología debe ser altamente recomendada como estrategia educacional en medicina, ya que podría acelerar la adquisición de habilidades clínicas en un ambiente de aprendizaje seguro.
Physicians commonly perform paracentesis procedure in patients with ascites. Inadequate technique can be associated with adverse events such as intestinal perforation, hemorrhage or puncture site infection, with a rate of 1.6% according to literature.1 The low-risk complications and incidents are frequently underreported.2 Furthermore, Sharzehi et al. describes in a systematic review about complications in paracentesis that hemorrhagic complications are more frequent in untrained professionals, which makes an early-simulated training essential to prevent the risk of complications.3
This technique has been taught with Halsted's traditional model of “See one, do one and then teach a procedure”, which is based on students watching their tutors and then practicing the procedure on patients under an expert supervision.4,5 The problem with this method is that students execute the first procedures in a non-standardized way in real patients with risk for both, patients and students, extended learning time and costs related to education.4,6,7 On the other hand, patient safety is the cornerstone of high-quality health care. The Joint Commission and other accreditation entities related to healthcare safety and quality demand lower rates of complications and needlestick injuries in procedures.8 Low rates of complications and incidents, including those of low risk, reflect high-quality health care, and nowadays, needlestick complications are part of the standards for hospitals’ accreditation.
In response to these challenges, simulated training emerges as an alternative within medical education, creating an ideal learning environment where activities can be designed to be predictable, consistent, standardized, secure and reproducible.9–11 Simulated training has shown to be effective for the acquisition of different medical-surgical skills such as sutures, intubations, pleural puncture and cardiopulmonary resuscitation.12–14 However, currently there are few simulated training programs in paracentesis. Although these programs have demonstrated a clear benefit in learning, they have only been tested in postgraduate students with low number of participants.15 The aims of the present study are: to design and implement a simulation-based teaching methodology for training undergraduate medical students in paracentesis technique; to evaluate students’ performance in abdominal paracentesis using a simulated model; and to determine the students’ perception of this workshop.
MethodsParticipantsFourth-year undergraduate medical students doing their mandatory clinical rotation in Gastroenterology (as part of the core curriculum at the integrated medical-surgical course) were included. Students who had previously performed a paracentesis simulated training program or at least one procedure in a real patient were excluded. This project was approved by the Ethics Committee of the Pontificia Universidad Católica de Chile.
Educational support materialA group of experts developed educational support material on paracentesis technique including theoretical and practical concepts. This educational support material included concepts about portal hypertension and its complications, as well as differential diagnosis and treatment of ascites. It also included a video entitled “ascites problem”, which explained in a didactic way the different stages of the technique of abdominal paracentesis.16 The participants were asked to review the educational support material prior to the training session in order to have homogeneous theoretical framework among the students.
Simulated modelA group of experts (gastroenterologists & surgeons) together with designer specialists in simulated models developed a model of abdominal paracentesis for educational purpose. A qualitative analysis of clinical teacher educational needs was carried out, including characteristics such as: fidelity, ease of washing and transportation, capacity for reuse, low cost and safety for students’ use. The prototypes were built using a special 3D printer system. The model was validated by serial tests of experts group. During each test, verbal and written feedback was requested regarding the strengths and weaknesses of the model to increase the fidelity between the prototype and the real patient.17 The two main conclusions were that the thickness of the patch had to be more realistic and that this patch should allow a pulling maneuver to correctly perform the Z track technique. The final model consisted of a rigid case with a bag that simulated intra-abdominal pressure and a puncture area with a patch of 10mm thickness with different layers, which allowed Z-traction of the skin (Fig. 1). The innovative characteristics of this paracentesis model leaded to a patent application. Its design methodology was published elsewhere.18
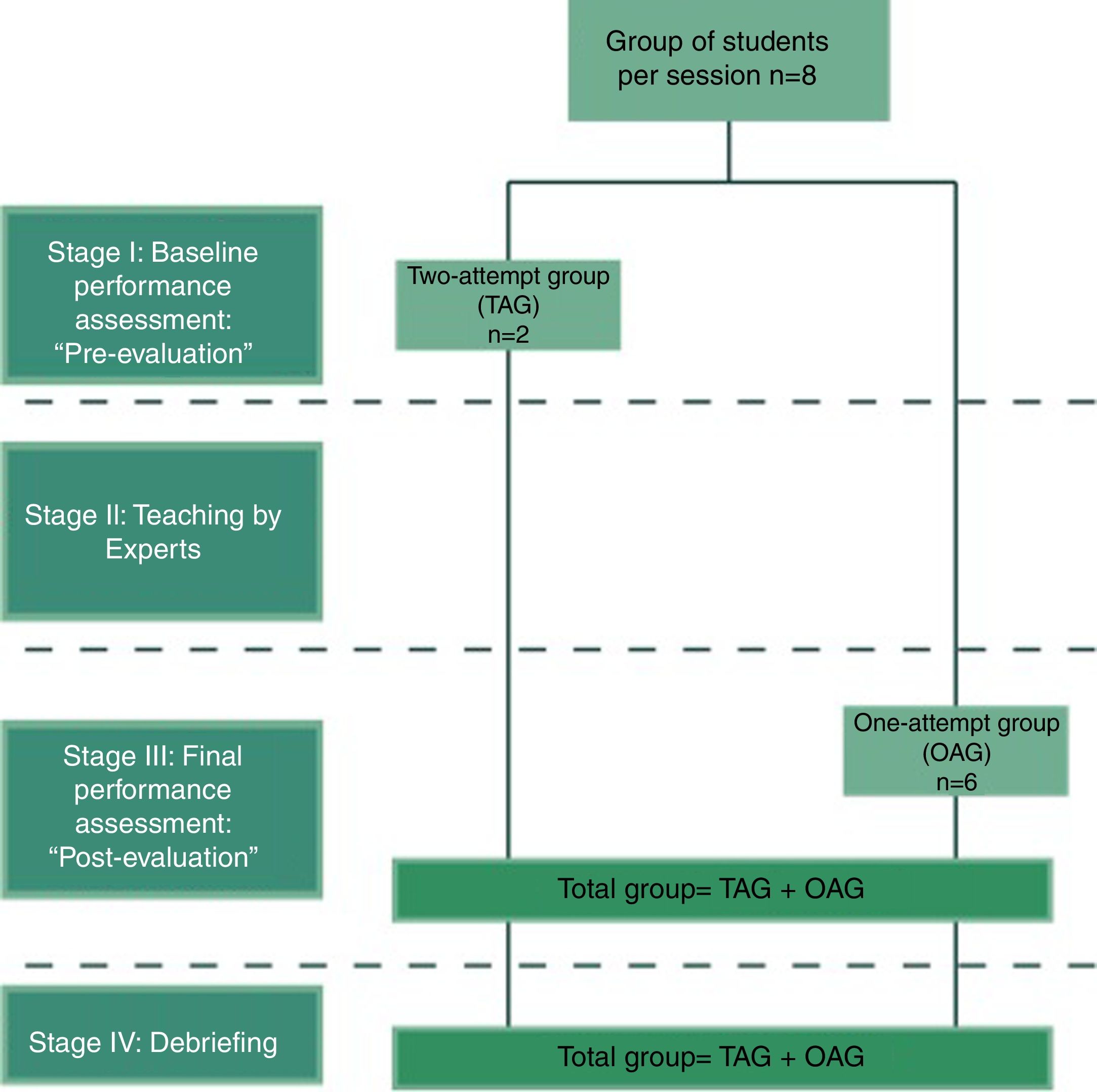
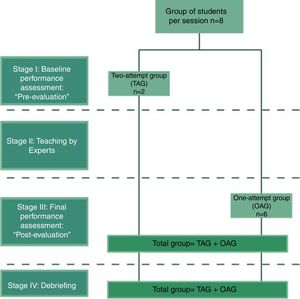
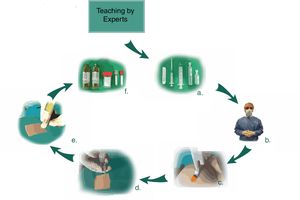
Training sessionA 3-hour-workshop was implemented for 8 students per session, structured in 4 stages (see Fig. 2):
(I) Definition of groups and determination of baseline level: Pre-evaluation at the beginning of the session, 2 students were randomly selected. These students were allocated to the group called two-attempt group given that they performed an initial evaluation prior to begin the training session, defined as “pre-evaluation” plus a final performance assessment, defined as “post-evaluation”. The rest of the students were allocated to the one-attempt group and performed only the post-evaluation without a baseline assessment. This group was composed of the remaining 6 students of each session.
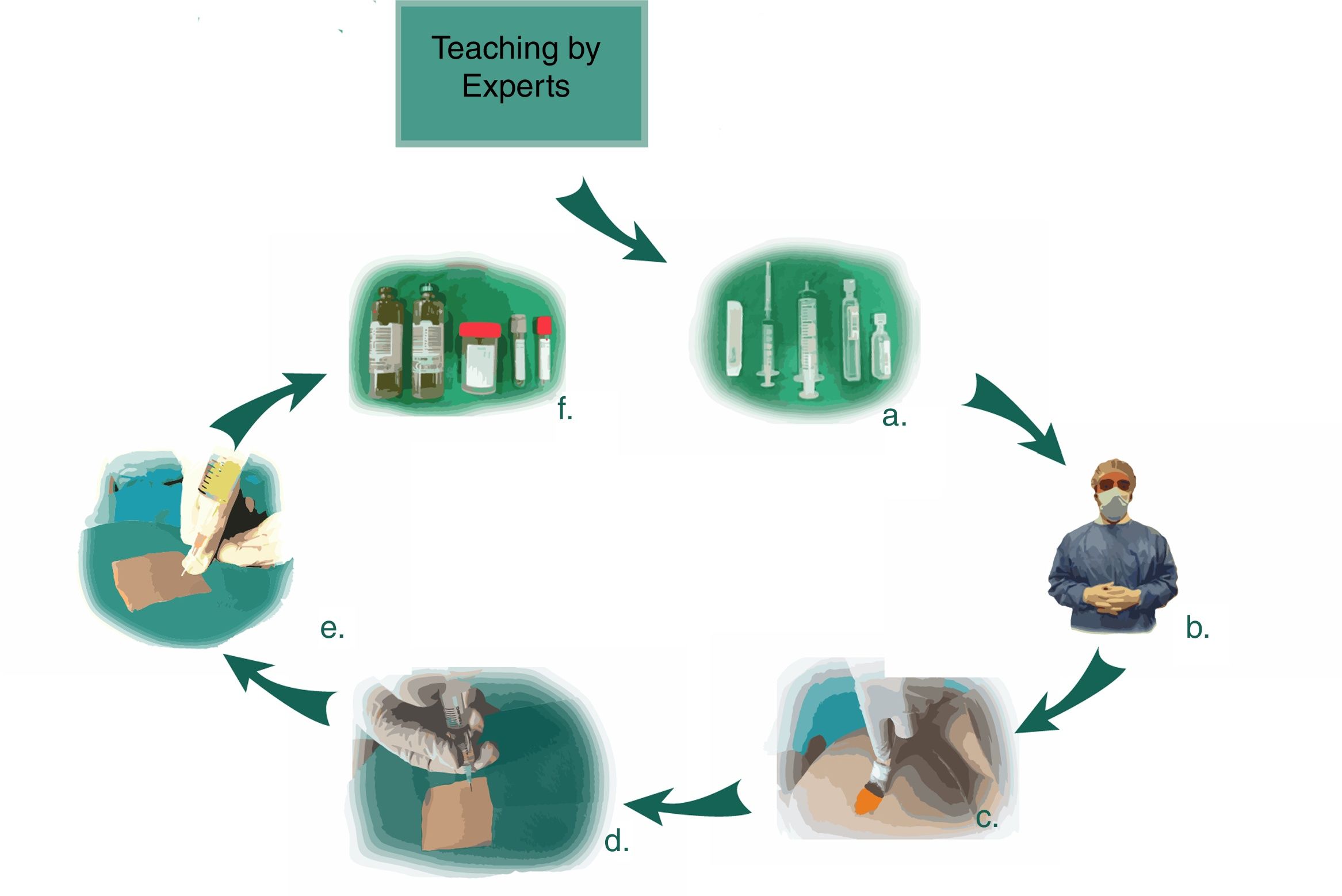
(II) Teaching by experts: This activity was based on 2 pillars. Initially there was a verbal explanation of the critical steps of the procedure, watching with the students the video “ascites problem”.16 Later the expert performed the technique of paracentesis in the simulated model emphasizing the critical steps of the procedure. Stages of the abdominal paracentesis are illustrated in Fig. 3.
Paracentesis simulation: instructions included the following steps of the procedure: (a) requested material; (b) wear apron, hat, mask and gloves; (c) clean skin with disinfectant; (d) setup a sterile field and infiltrate lidocaine; (e) aspirate ascitic fluid; (f) fill tubes with samples for analysis.
(III) Final performance assessment: It consisted in the assessment of the execution of an abdominal paracentesis in the simulated model after the teaching by experts. This stage was structured based on the methodology of “role playing”, in which all the students performed once each activity of the procedure: execution of the paracentesis in the simulated model, role of the technical assistant and peer assessment role of the procedure. An expert applied a direct observation checklist (see elsewhere) to the student that executed the paracentesis in the simulated model.
(IV) Debriefing: Finally the trainer carried out a session of debriefing for the effective delivery of feedback based in the plus-delta model.17
Checklist of direct observationA direct observation checklist (DOC) was created considering the key features of abdominal paracentesis, following the structure of a DOPS (Direct Observation of Procedural Skills) instrument, which is used in Workplace-Based Assessment with real patients.19 This instrument was developed by an experts’ panel following the Delphi technique methodology, determining 24 key-points, that allowed the trainers to assess the student (trainee) including communication skills (obtaining patient informed consent); sequential steps of the procedure (asepsis, anesthesia, puncture, and taking laboratory samples) and post-procedure instructions for the health team (Technical assistant and nurse; Teamwork skills). An expert applied this DOC during the pre-evaluation and post-evaluation with which objective scores were obtained. In this DOC, 1 point was assigned when the student met each key feature and 0 points if he/she did not (dichotomic items). The final score of the checklist was defined as the sum of the obtained points in each specific item/key feature. The percentage of checklist compliance was defined as the final score of the checklist/total score of the checklist (24 points). The global yield of the pre-evaluation and post-evaluation were expressed as the total score average of the students of each group.
Inter-observer agreement assessment (reliability)Peers also applied the DOC during post-evaluation for each student, but this evaluation was only for feedback and to assess the agreement between experts and peers. It was not considered to analyze the acquisition of competencies according to the DOC applied by the expert.
Assessment of the workshop perceptionA 7-item questionnaire was applied about the perception of simulated procedures. Barsuk15 designed this questionnaire for internal medicine residents, and it was adapted and translated into Spanish and administered in undergraduate students that participated in our study.20 The instrument consisted in 7 assertions about the perception of the simulated workshop; each student assigned a score from 1 to 5 (5-points Likert Scale) according to their grade of agreement with the proposed assertion.
Statistical analysisThe Student's t-test was used for related samples to compare each item of the DOC as well as the total results between the pre-evaluation and post-evaluation. It was applied for the comparisons between the final learning outcomes between the one-attempt group and two-attempt group and for the analysis of the perception based on the 7-item questionnaire scores. Chi square or exact Fisher test were used to compare the proportions between the groups. Bland–Altman analysis was used to assess inter-rater reliability of the DOC between expert and peers’ assessment.21 The SPSS version 17 (2009, Chicago IL, USA), Lavan (psych) and R softwares were used for the analysis of the previously described.
ResultsParticipantsA total of 247 students were included in this protocol. Students were allocated in 2 groups: two-attempt group (TAG/n=69) and one-attempt group (OAG/n=178). No significant differences were observed between the median ages or in the percentage of male participants between both groups [21 (20–23) years vs 21 (20–23) years and 45 (65%) vs 112 (63%) for TAG and OAG respectively]. We had two students with finger puncture (0.8%) as a mild adverse event without serious adverse events for the participants.
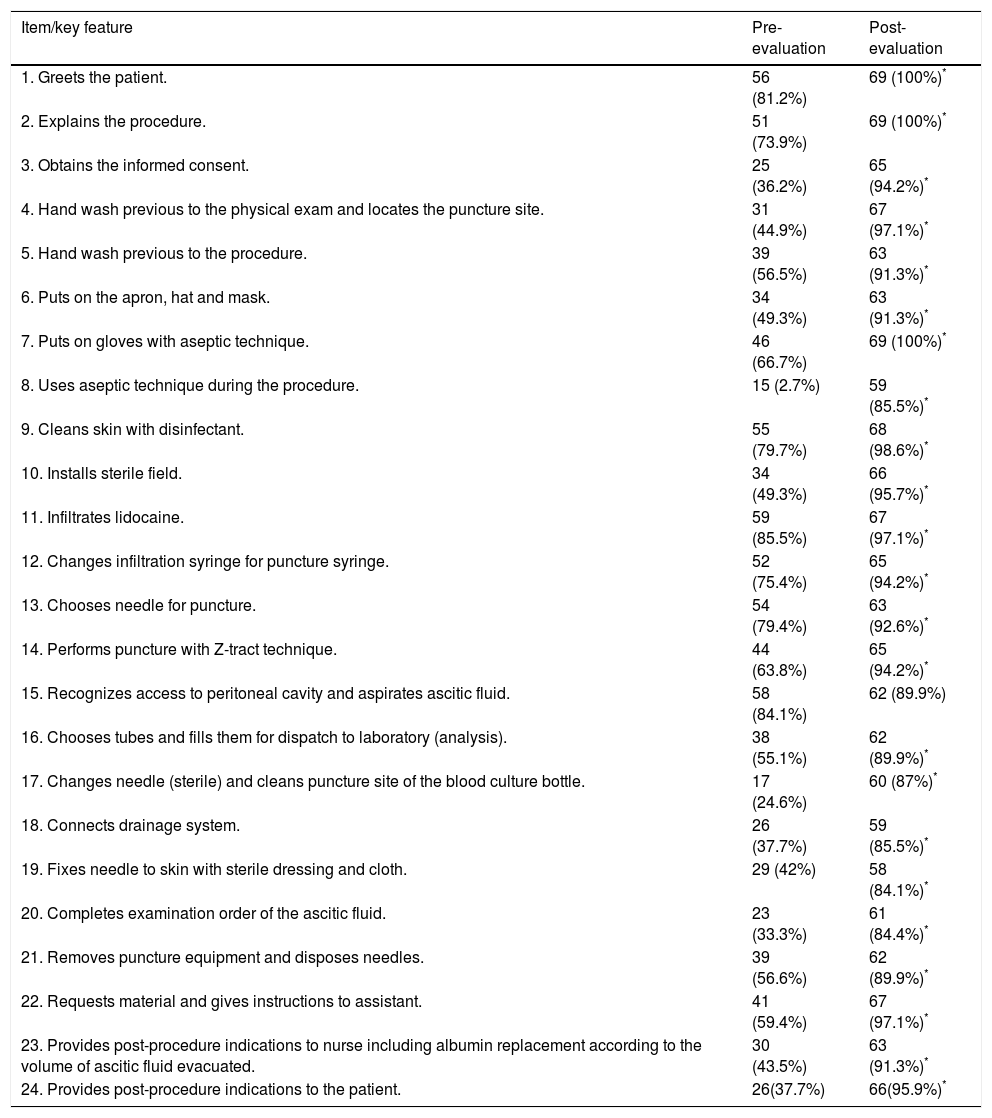
Progression of learningTable 1 shows the number and percentage of students that approved each specific key feature in the TAG during the pre-evaluation and post-evaluation. It is observed that during the execution of the post-evaluation the percentage of students that approves is statistically superior in comparison to the pre-evaluation in all the items/key features of the checklist.
Results obtained in the baseline performance assessment (pre-evaluation) and final performance assessment (post-evaluation). Number (percentage) of students that approved the key feature.
| Item/key feature | Pre-evaluation | Post-evaluation |
|---|---|---|
| 1. Greets the patient. | 56 (81.2%) | 69 (100%)* |
| 2. Explains the procedure. | 51 (73.9%) | 69 (100%)* |
| 3. Obtains the informed consent. | 25 (36.2%) | 65 (94.2%)* |
| 4. Hand wash previous to the physical exam and locates the puncture site. | 31 (44.9%) | 67 (97.1%)* |
| 5. Hand wash previous to the procedure. | 39 (56.5%) | 63 (91.3%)* |
| 6. Puts on the apron, hat and mask. | 34 (49.3%) | 63 (91.3%)* |
| 7. Puts on gloves with aseptic technique. | 46 (66.7%) | 69 (100%)* |
| 8. Uses aseptic technique during the procedure. | 15 (2.7%) | 59 (85.5%)* |
| 9. Cleans skin with disinfectant. | 55 (79.7%) | 68 (98.6%)* |
| 10. Installs sterile field. | 34 (49.3%) | 66 (95.7%)* |
| 11. Infiltrates lidocaine. | 59 (85.5%) | 67 (97.1%)* |
| 12. Changes infiltration syringe for puncture syringe. | 52 (75.4%) | 65 (94.2%)* |
| 13. Chooses needle for puncture. | 54 (79.4%) | 63 (92.6%)* |
| 14. Performs puncture with Z-tract technique. | 44 (63.8%) | 65 (94.2%)* |
| 15. Recognizes access to peritoneal cavity and aspirates ascitic fluid. | 58 (84.1%) | 62 (89.9%) |
| 16. Chooses tubes and fills them for dispatch to laboratory (analysis). | 38 (55.1%) | 62 (89.9%)* |
| 17. Changes needle (sterile) and cleans puncture site of the blood culture bottle. | 17 (24.6%) | 60 (87%)* |
| 18. Connects drainage system. | 26 (37.7%) | 59 (85.5%)* |
| 19. Fixes needle to skin with sterile dressing and cloth. | 29 (42%) | 58 (84.1%)* |
| 20. Completes examination order of the ascitic fluid. | 23 (33.3%) | 61 (84.4%)* |
| 21. Removes puncture equipment and disposes needles. | 39 (56.6%) | 62 (89.9%)* |
| 22. Requests material and gives instructions to assistant. | 41 (59.4%) | 67 (97.1%)* |
| 23. Provides post-procedure indications to nurse including albumin replacement according to the volume of ascitic fluid evacuated. | 30 (43.5%) | 63 (91.3%)* |
| 24. Provides post-procedure indications to the patient. | 26(37.7%) | 66(95.9%)* |
Fig. 4 shows the final learning results of group TAG in the pre-evaluation and post-evaluation. The students (n=69) significantly improved their skills after the simulated training [pre-evaluation: 13.36±4.46 points vs post-evaluation: 22.3±1.83 points; p<0.001]. The percentage of DOC fulfillment was 55.7% and 93% for the pre-evaluation and post-evaluation respectively. No considerable statistical differences were observed in the total time of procedure execution [pre-evaluation: 1001.9±374.7seconds vs post-evaluation: 956.9±297.3seconds, p>0.05].
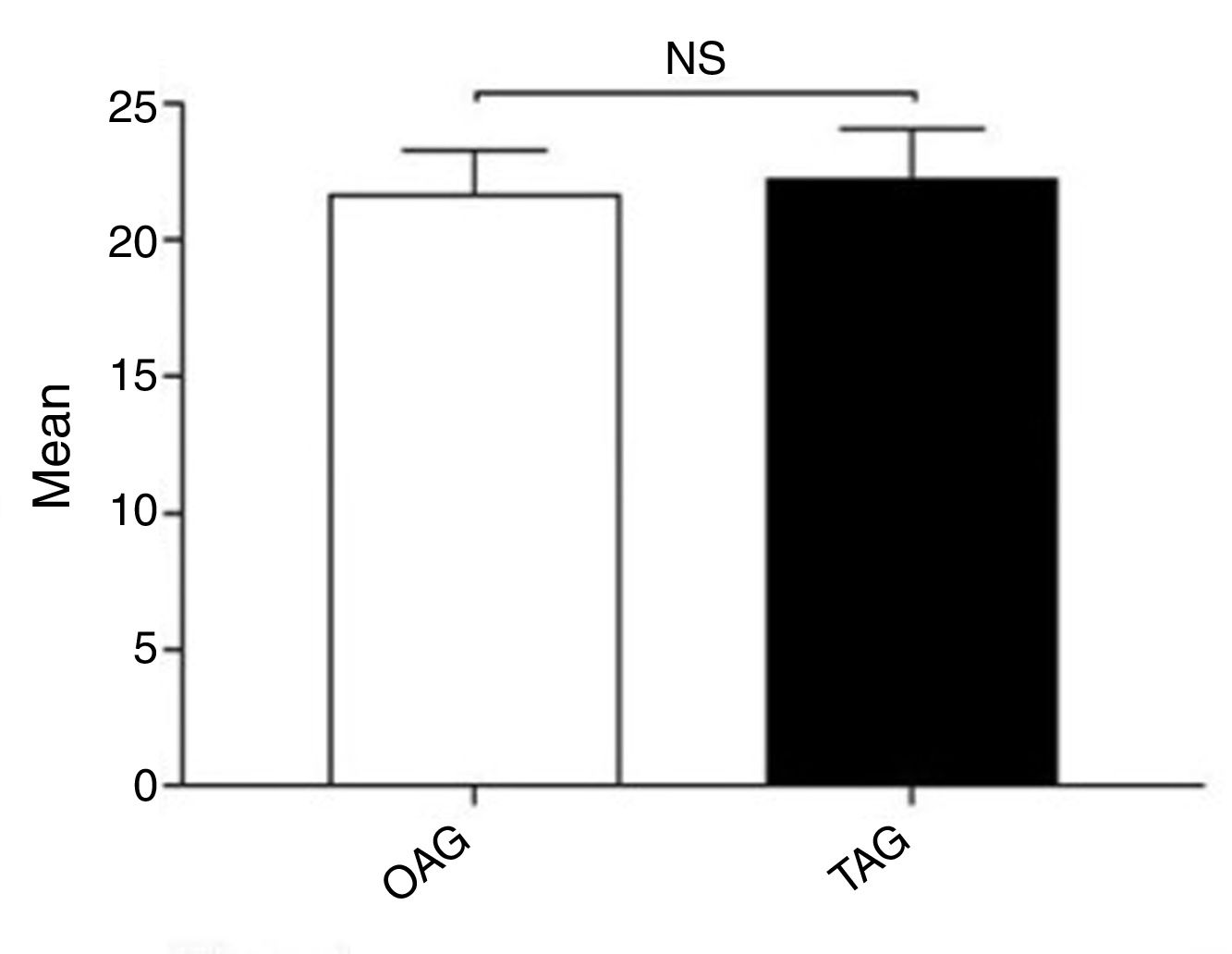
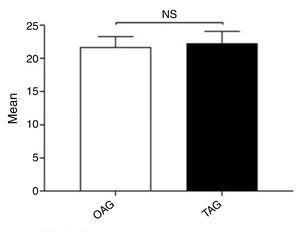
Determination of the impact of a basal skill testTo assess the impact of a higher number of punctures during the simulated training the results of the post-evaluation between the students of the OAG vs TAG were compared. As observed in Fig. 5, no significant statistical differences were observed between both groups [OAG: 21.7±2.79 vs TAG: 22.3±1.83 points, p>0.05].
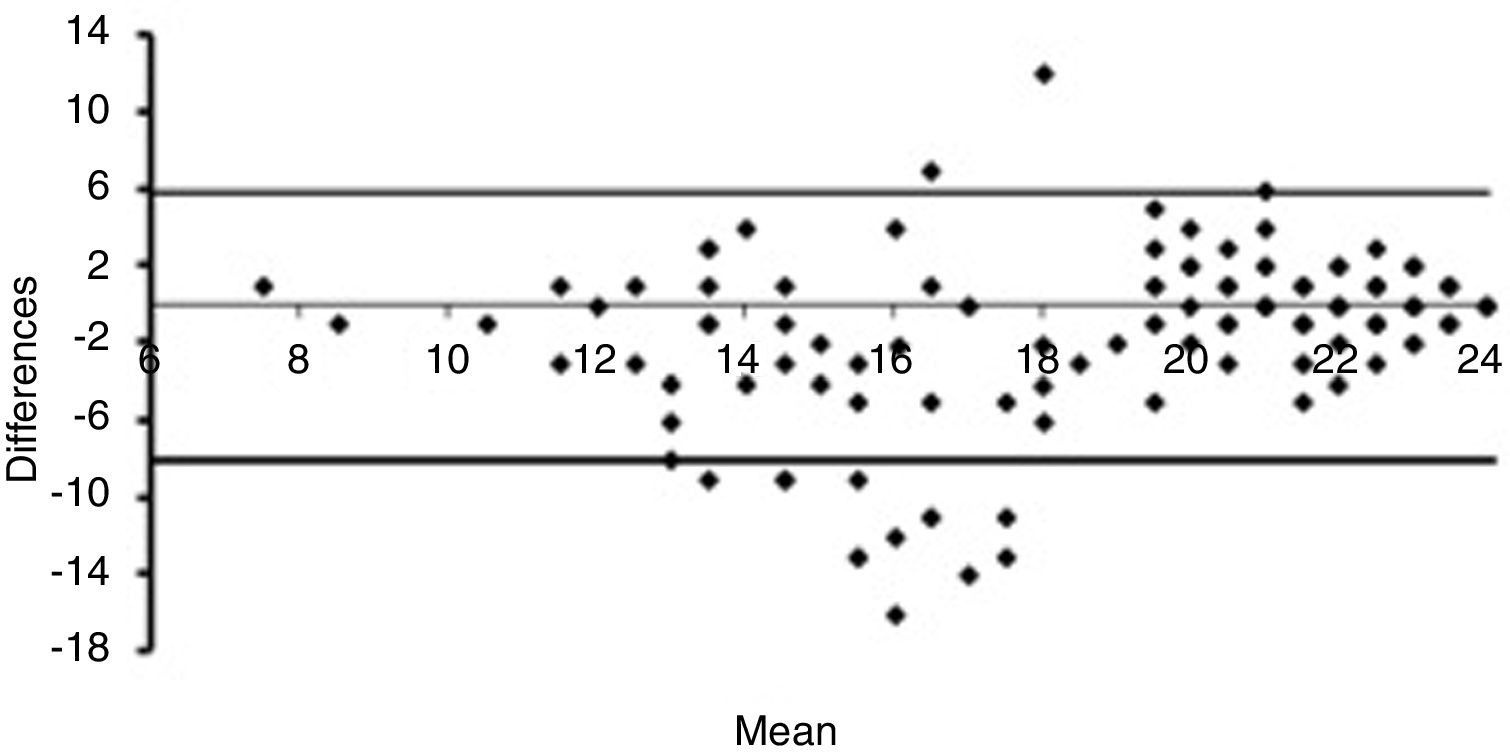
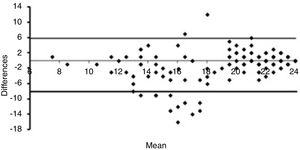
Inter-observer agreement assessmentThe agreement of the final learning outcomes was evaluated according to the Bland and Altman analysis.21 When the student obtains less than 11 points on DOC, there is a high agreement between experts and peers; in this case, we had a small number of students with less than 11 point. Between 12 and 18 points on DOC, the agreement is low, with a clear tendency of the pairs to evaluate with higher scores their classmates compared to experts. Above 18 on DOC, there is a high agreement between experts and peers (Fig. 6).
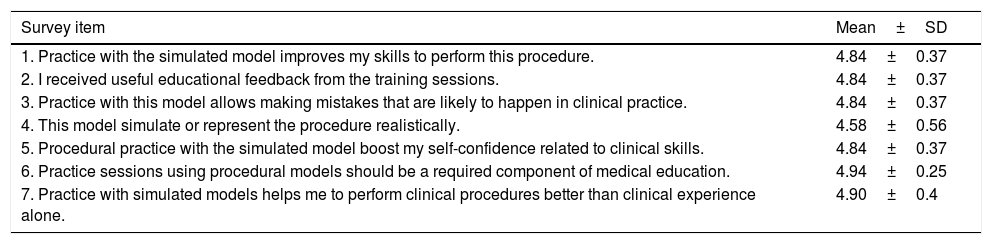
Assessment of the workshop perceptionThe students’ perception questionnaire showed that the training session was highly valued by the students, reaching an average of 4.8±0.38 points based on a 5-point Likert scale, where 1=strongly disagree, and 5=strongly agree (Table 2).
Results of the students’ perceptions questionnaire of the abdominal paracentesis workshop.
| Survey item | Mean±SD |
|---|---|
| 1. Practice with the simulated model improves my skills to perform this procedure. | 4.84±0.37 |
| 2. I received useful educational feedback from the training sessions. | 4.84±0.37 |
| 3. Practice with this model allows making mistakes that are likely to happen in clinical practice. | 4.84±0.37 |
| 4. This model simulate or represent the procedure realistically. | 4.58±0.56 |
| 5. Procedural practice with the simulated model boost my self-confidence related to clinical skills. | 4.84±0.37 |
| 6. Practice sessions using procedural models should be a required component of medical education. | 4.94±0.25 |
| 7. Practice with simulated models helps me to perform clinical procedures better than clinical experience alone. | 4.90±0.4 |
Simulated training has consistently shown its efficiency as a teaching tool for undergraduate medical student skills.12–14
The present work shows the development of an innovative teaching methodology about skills in paracentesis. To the date, the teaching of this competence has been performed using the traditional teaching model. A critical key point in this model is that if there are not enough inpatients with ascites during the rotation of the students, a significant percent finishes their rotations (even their clerkship) without the opportunity to see or perform a paracentesis in a patient. The acquisition of this skill is heterogeneous between the same generations of students, thereby is necessary moving from the opportunistic approach to a more systematic training process, according to the SPICES model.22 This training program is a concrete alternative to complement the traditional teaching model and guarantee an optimal performance from the future physicians.9,23
The feedback model used was based in the principles of the assessment for learning.24,25 In the same way, the “teaching by experts” phase plays a crucial role in the workshop as shown in Fig. 3. In this phase, one of the gastroenterology tutors performed a paracentesis in the paracentesis model, emphasizing the critical steps of the procedure. No significant differences revealed in the comparison of the final post-evaluation between TAG and OAG, could mean that the feedback provided by the experts during the simulated procedure is even more important than doing a simulated paracentesis twice.
The main difficulty for the creation of a program of these characteristics is to obtain simulated models that represent an abdomen with ascites. Even if there were commercial models available for this purpose, their main limitations were the low fidelity and high cost (above USD 9000). For that reason, our team developed a simulated model of ascites that fulfilled these educational gaps. The development of this low-cost paracentesis mannequin was possible due to an educational grant awarded by this working process. A new patent application was submitted (No. 201702133. Technology: “Device for simulation and training in different puncture techniques”. N/Ref.: 273025-CL).
Results obtained in relation to learning progression demonstrate the effectiveness of the simulated workshop in the teaching of paracentesis technique. This is the first work in assessing this teaching methodology of paracentesis in undergraduate students. This highlights the importance of a structured simulation workshop, with a team of experts dedicated to its implementation.
On the other hand, low baseline performance could be explained due to this workshop is one of the first clinical approaches during the first clinical year of the students (fourth-year undergraduate medical students at the PUC Medical School). Nevertheless, in similar studies of bedside procedures, the baselines for these critical features of direct observation checklists are lower as too.26,27
The analysis of correlation between the assessment by experts and students shows that the students do not manage to make a carry out a completely objective assessment of their peers. Although this implies that it is not possible to use the assessment by peers to obtain reliable measurements, we consider that it is an enriching element within the training session, for it induces the students to focus in the simulation and to reflect about the successes and errors of other partners. This could help to reinforce the learning and consolidate what was learned during the training session.
This study does not have the predictive validity to perform the procedure in a real environment. However, given experiences of previous authors and of our team work regarding the transfer of acquired abilities in simulation to real patients we believe that it will be a useful tool for the students during the clinical practice.28,29 According to literature, the early introduction to the clinical practice of students, accelerate the mastery of procedures during the internship and residency.30
One of the main deficiencies of the present study is the lack of long-term follow-up of students in order to assess the real performance in patients. The application of the direct observation checklist immediately after the workshop could overestimate the good results obtained. This was not considered an aim of this work because it was an initial experience to determine the effectiveness of simulated training in paracentesis skills acquisition. In the future, we are planning a follow-up protocol of students trained in our simulated program, in order to assess their performance in real patients (transference from simulated training program to real patients with ascites) including clinical skills, patients and trainee's safety outcomes.28
Another possible limitation of this study is the lack of validation of the direct observation checklist that was used. Given to date that there are not international validated instruments for the evaluation of this skill in undergraduate students, our team decided to develop an observation checklist based in Delphi methodology. This methodology is recommended by the literature for the generation of this kind of instruments. Although we acknowledge it was not previously validated in a structured way, we consider its application was satisfactory, attaining reliable results.
In conclusion, a teaching methodology based in simulation for the training of paracentesis for undergraduate medical students was designed and implemented. The present study proved that this simulated training program is an effective tool in the acquisition of necessary skills for the procedure of abdominal paracentesis and is a highly valued methodology by the undergraduate students of medicine as part of their curriculum.
SupportThis work was financed by Funds of the Project “Design, development and implementation of a simulated model for teaching & learning diagnostic abdominal paracentesis in undergraduate medical students”, FONDEDOC 2013 A.R.-I.C. “Standardized learning curves and transference to real patients of paracentesiś skills acquired through simulation” FONDEDOC 2016 A.R. and the “First patent & transference research grant”, Transference & Development Unit. PUC 2017 A.R. This work is part of the Master of Health Science thesis authored by Martin Inzunza.
Conflict of interestThe authors declare no conflict of interests.