Endoscopic retrograde cholangiopancreatography (ERCP) is an essential technique in the treatment of biliary and pancreatic disease. The overall complication rate of ERCP is approximately 6.9%.1 The development of a subcapsular hepatic haematoma is an uncommon event, although it is probably underdiagnosed. In most cases the outcome is favourable, but vascular embolisation and/or surgical intervention can be necessary.2
We first present the case of a 35-year-old woman referred with acute cholangitis secondary to choledocholithiasis. The patient had normal coagulation (platelets 181,000/μl and INR 0.95). ERCP was performed with selective channelling of the bile duct using a hydrophilic guidewire (Hydra Jagwire™, Boston Scientific, USA). The cholangiogram showed an extrahepatic bile duct measuring 15mm with multiple filling defects. After performing a biliary sphincterotomy and sphincteroplasty with balloon dilation using a CRE™ balloon (Boston Scientific, USA) of 15mm diameter for 1min, all stones were extracted with a Fogarty balloon (Extractor™ Pro, Boston Scientific, USA). Four hours later, the patient developed hypotension, decreased level of consciousness and anaemia, with haemoglobin of 6.9g/dl. Abdominal CT with intravenous contrast (IVC) identified a subcapsular haematoma measuring 140×45mm in the right lobe of the liver (RLL). The patient made a good recovery with conservative treatment, including antibiotic therapy, and was discharged after 18 days. A follow-up CT scan at four months showed a decrease in the size of the haematoma (49×22mm).
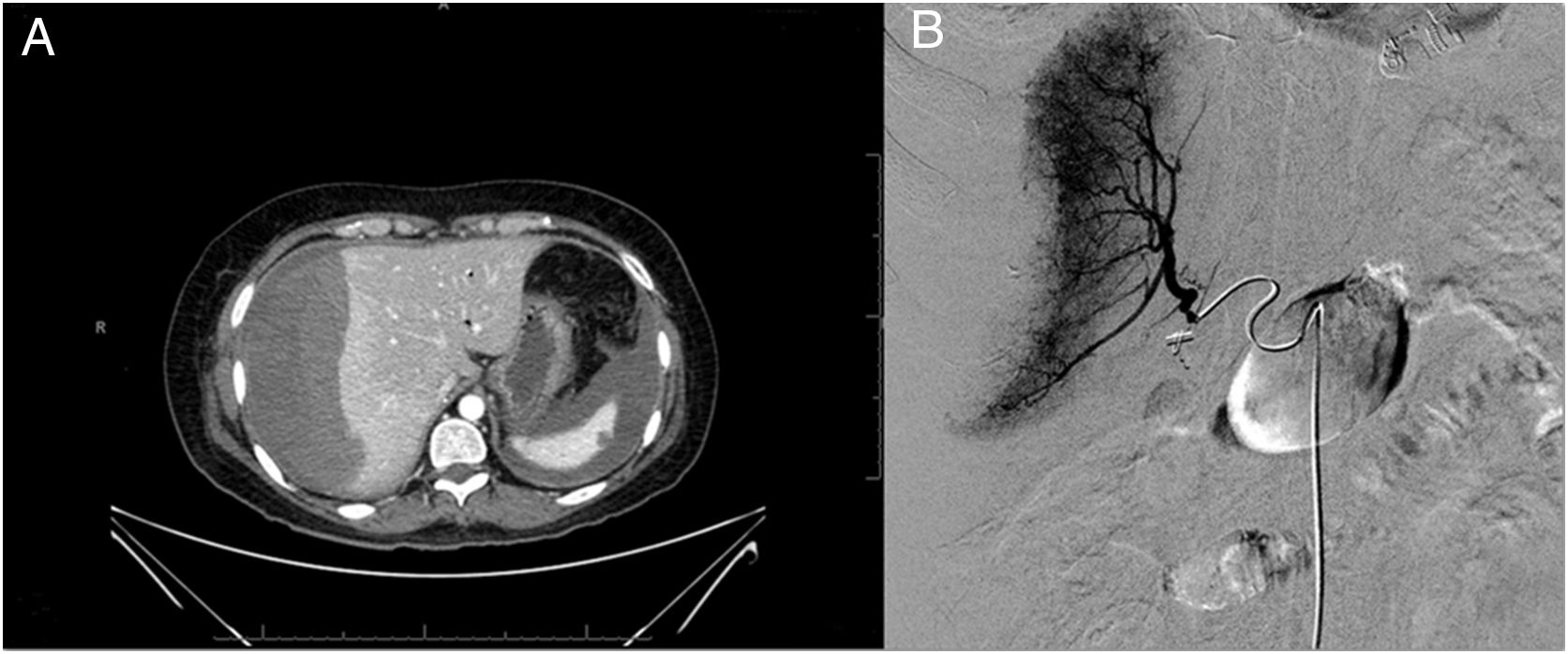
Next, we present the case of a 54-year-old woman with previous cholecystectomy admitted for choledocholithiasis with dilation of the bile duct. The patient had normal coagulation (platelets 233,000/μl and INR 0.94). An ERCP was performed where a papilla was visualised with previous sphincterotomy, the bile duct was selectively cannulated with sphincterotome, and multiple biliary casts were extracted. Two hours later, the patient developed abdominal pain, hypotension and anaemia with haemoglobin of 5.6g/dl with Fogarty balloon. Abdominal CT with IVC showed a subcapsular haematoma in the RLL (170×40×150mm) and a leak of contrast at that location, suggestive of active bleeding. As the bleeding was not confirmed by selective arteriogram, conservative treatment was maintained (transfusion, IV fluids and broad-spectrum antibiotic therapy). At 72h, the patient had a recurrence of the bleeding and abdominal CT with IVC showed that the haematoma had grown in size (100×120×190mm), with findings (Fig. 1) suggestive of active bleeding in segment V. In a repeat angiographic study, multifocal active punctate arterial bleeding was confirmed on the surface of the RLL (in relation to rupture of (Fig. 1) small vessels between the liver surface and the capsule after primary distension due to the initial haematoma) associated with severe vasospasm of the right hepatic artery, which was resolved with glyceryl trinitrate and embolisation with Spongostan® particles. As with the first case, she made a good recovery.
The most common haemorrhagic complication after an ERCP is post-sphincterotomy bleeding (1.3%).1 One complication within this subgroup which is underdiagnosed is intrahepatic bleeding, leading to the formation of a subcapsular hepatic haematoma, predominantly in the RLL.
The aetiopathogenic mechanism is not fully understood. The main theory suggests the presence of a mechanical component associated with the use of the guidewire, which would seem to cause trauma in the biliary tree and adjacent small intrahepatic vessels.3 In some cases, it seems to be associated with the traction caused by the endoscope itself or by the Fogarty balloon.4 In terms of the distribution of the haematoma, it is suggested that this is determined by the filtering of blood through the hepatic parenchyma in a centrifugal direction, and the pathophysiology is completed by the presence of a solid hepatic capsule containing the haematoma.5
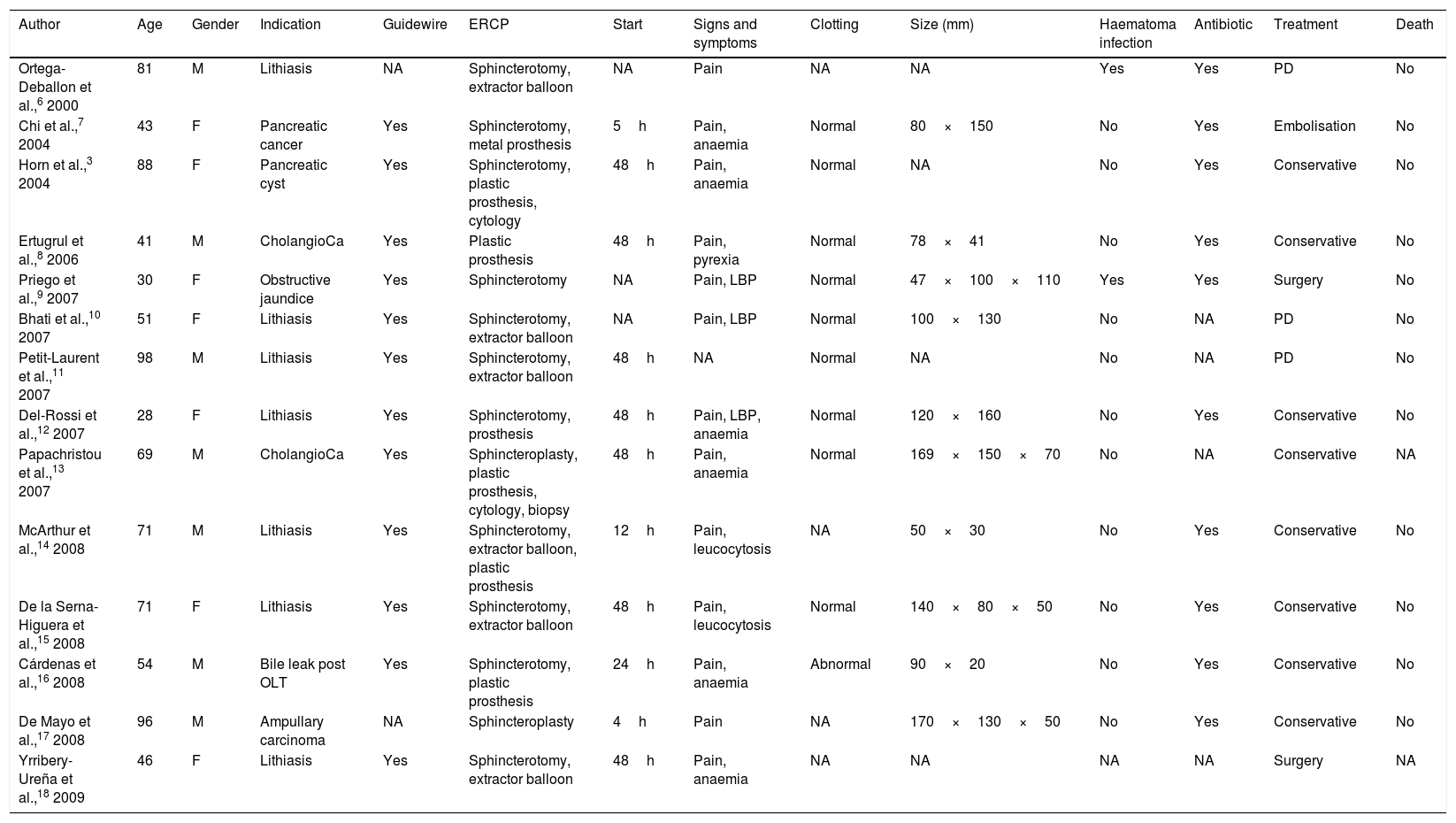
Up to 2016, 42 cases had been documented in the literature (Table 1). There are no significant differences in terms of gender or age, and choledocholithiasis is the most common indication. In most cases, the onset of symptoms occurs in the first 48h and abdominal pain is the predominant manifestation. Management is usually conservative, with surgery required in less than 30% of cases. Morbidity and mortality rates may be overestimated given that the documented cases are probably more serious and many cases are pauci-symptomatic.
Reported cases of subcapsular hepatic haematoma after ERCP.
| Author | Age | Gender | Indication | Guidewire | ERCP | Start | Signs and symptoms | Clotting | Size (mm) | Haematoma infection | Antibiotic | Treatment | Death |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ortega-Deballon et al.,6 2000 | 81 | M | Lithiasis | NA | Sphincterotomy, extractor balloon | NA | Pain | NA | NA | Yes | Yes | PD | No |
| Chi et al.,7 2004 | 43 | F | Pancreatic cancer | Yes | Sphincterotomy, metal prosthesis | 5h | Pain, anaemia | Normal | 80×150 | No | Yes | Embolisation | No |
| Horn et al.,3 2004 | 88 | F | Pancreatic cyst | Yes | Sphincterotomy, plastic prosthesis, cytology | 48h | Pain, anaemia | Normal | NA | No | Yes | Conservative | No |
| Ertugrul et al.,8 2006 | 41 | M | CholangioCa | Yes | Plastic prosthesis | 48h | Pain, pyrexia | Normal | 78×41 | No | Yes | Conservative | No |
| Priego et al.,9 2007 | 30 | F | Obstructive jaundice | Yes | Sphincterotomy | NA | Pain, LBP | Normal | 47×100×110 | Yes | Yes | Surgery | No |
| Bhati et al.,10 2007 | 51 | F | Lithiasis | Yes | Sphincterotomy, extractor balloon | NA | Pain, LBP | Normal | 100×130 | No | NA | PD | No |
| Petit-Laurent et al.,11 2007 | 98 | M | Lithiasis | Yes | Sphincterotomy, extractor balloon | 48h | NA | Normal | NA | No | NA | PD | No |
| Del-Rossi et al.,12 2007 | 28 | F | Lithiasis | Yes | Sphincterotomy, prosthesis | 48h | Pain, LBP, anaemia | Normal | 120×160 | No | Yes | Conservative | No |
| Papachristou et al.,13 2007 | 69 | M | CholangioCa | Yes | Sphincteroplasty, plastic prosthesis, cytology, biopsy | 48h | Pain, anaemia | Normal | 169×150×70 | No | NA | Conservative | NA |
| McArthur et al.,14 2008 | 71 | M | Lithiasis | Yes | Sphincterotomy, extractor balloon, plastic prosthesis | 12h | Pain, leucocytosis | NA | 50×30 | No | Yes | Conservative | No |
| De la Serna-Higuera et al.,15 2008 | 71 | F | Lithiasis | Yes | Sphincterotomy, extractor balloon | 48h | Pain, leucocytosis | Normal | 140×80×50 | No | Yes | Conservative | No |
| Cárdenas et al.,16 2008 | 54 | M | Bile leak post OLT | Yes | Sphincterotomy, plastic prosthesis | 24h | Pain, anaemia | Abnormal | 90×20 | No | Yes | Conservative | No |
| De Mayo et al.,17 2008 | 96 | M | Ampullary carcinoma | NA | Sphincteroplasty | 4h | Pain | NA | 170×130×50 | No | Yes | Conservative | No |
| Yrribery-Ureña et al.,18 2009 | 46 | F | Lithiasis | Yes | Sphincterotomy, extractor balloon | 48h | Pain, anaemia | NA | NA | NA | NA | Surgery | NA |
| Nari et al.,19 2009 | 15 | F | Pancreatitis | NA | NA | NA | Pain, pyrexia | NA | 135×49×35 | No | Yes | Conservative | No |
| Saa et al.,20 2010 | 92 | NA | Lithiasis | NA | Sphincterotomy | 24h | Anaemia | NA | NA | Yes | NA | PD+surgery | Yes |
| Revuelto Rey et al.,21 2010 | 41 | M | Lithiasis | NA | Sphincterotomy | 6h | Pain, anaemia | NA | 130×90×110 | NA | Yes | Conservative | No |
| Baudet et al.,4 2011 | 69 | F | Lithiasis | Yes | Sphincterotomy, extractor balloon | 4h | Pain, anaemia, pyrexia, LBP | NA | 160×65×21 | Yes | Yes | Embolisation+surgery | No |
| Pérez-Legaz et al.,22 2011 | 72 | F | Lithiasis | NA | Sphincterotomy | 2h | Pain, anaemia, LBP | NA | 80 | NA | NA | Surgery | No |
| Del Pozo et al.,23 2011 | 76 | F | Lithiasis | Yes | Sphincterotomy, extractor balloon | 5d | Pain | Abnormal | NA | NA | Yes | Conservative | No |
| Orellana et al.,24 2012 | 96 | M | Periampullary tumour | Yes | Plastic prosthesis, biopsies | 4h | Pain | NA | 170×130×50 | NA | Yes | Conservative | No |
| Orellana et al.,24 2012 | 49 | M | Occlusion of biliary prosthesis | Yes | Plastic prosthesis | 2h | Pain, LBP | NA | 50% of liver volume | NA | NA | Embolisation+PD | No |
| Orellana et al.,24 2012 | 55 | F | Dysfunction of bile duct prosthesis | Yes | Plastic prosthesis | NA | Pain | NA | 30% of liver volume | NA | NA | Conservative | No |
| Bartolo-Rangel et al.,25 2012 | 62 | F | Cholangitis | Yes | Sphincterotomy, extractor balloon | NA | LBP, anaemia | Normal | NA | NA | NA | Surgery | Yes |
| Patil et al.,26 2013 | 50 | M | Cholangitis | Yes | Sphincterotomy, extractor balloon | 48h | Pain | NA | 50×30 | No | Yes | PD | No |
| Oliveira-Ferreira et al.,27 2013 | 84 | M | Lithiasis | Yes | Extractor balloon | 10d | Pain, anaemia | Abnormal | 90×100 | Yes | Yes | PD | Yes |
| Fei et al.,28 2013 | 56 | M | Lithiasis | Yes | Sphincterotomy, basket | 2h | Pyrexia | NA | 130×60 | NA | Yes | PD | No |
| Carrica et al.,29 2014 | 37 | F | Lithiasis | Yes | Sphincterotomy | 72h | Pain, anaemia, pyrexia | NA | 124×93 | Yes | Yes | PD | No |
| Yoshii et al.,30 2014 | 86 | F | Lithiasis | NA | Lithotripsy and extraction in 4 sessions | 30h | Pain | NA | NA | NA | Yes | Conservative | No |
| González-López et al.,2 2015 | 30 | F | Benign choledochal stenosis | Yes | Sphincterotomy, choledochal dilation, biliary prosthesis | NA | Pain, anaemia, LBP | NA | NA | NA | NA | Surgery | Yes |
| Klìmovà et al.,31 2014 | 54 | M | Pancreatic lithiasis | Yes | Biliary and pancreatic sphincterotomy | 6h | Pain, anaemia, LBP | NA | 190×178×69 | Yes | Yes | Embolisation+surgery+PD | No |
| Solmaz et al.,32 2016 | 55 | M | Lithiasis | Yes | Sphincterotomy, extractor balloon | 6h | Pain | Normal | 140×67 | No | Yes | Conservative | No |
| Servide et al.,33 2016 | 83 | M | Cholangitis | NA | NA | 15d | Pain | NA | NA | NA | NA | Conservative | No |
| Zizzo et al.,5 2015 | 52 | F | Lithiasis | Yes | Sphincterotomy, nasobiliary drainage | 24h | Pain, anaemia, LBP | Normal | 150×110 | NA | NA | Embolisation | No |
| Zappa et al.,34 2016 | 58 | F | Lithiasis | Yes | Sphincterotomy | 12h | Pain, anaemia, LBP | NA | 140×60×190 | NA | NA | Embolisation | No |
| Kilic et al.,35 2016 | 69 | F | Lithiasis | NA | Sphincterotomy, extractor balloon, basket | 12h | Pain, LBP | Normal | 40×20 | Yes | Yes | Surgery+PD | No |
| Curvale et al.,36 2016 | 78 | M | Choledochal adenoma | Yes | Sphincterotomy, extractor balloon, basket, polypectomy | 1h | Pain, anaemia, LBP | Normal | NA | NA | NA | Surgery | No |
| Fiorini et al.,37 2016 | 47 | F | Lithiasis | Yes | Sphincterotomy, extractor balloon | 8h | Pain, pyrexia | NA | 45×45 | Yes | Yes | PD | No |
| Areopaja Escobar et al.,38 2016 | 47 | NA | Lithiasis | Yes | Sphincterotomy+prosthesis | 10d | Pain | NA | NA | NA | Yes | PD | No |
| Tamez et al.,39 2016 | 25 | F | Lithiasis | Yes | Sphincterotomy, extractor balloon | 12h | Pain, anaemia, LBP | Normal | 152×104×36 | NA | NA | Surgery | No |
| Present case 1 | 35 | F | Lithiasis | Yes | Sphincterotomy, sphincteroplasty, extractor balloon | <12h | Anaemia, LBP, drowsiness | Normal | 140×45 | No | Yes | Conservative | No |
| Present case 2 | 54 | F | Lithiasis | Yes | Extractor balloon (sphincterotomy previously) | 2h | Pain, anaemia, LBP | Normal | 100×120×190 | No | Yes | Embolisation | No |
CholangioCa: cholangiocarcinoma; ERCP: endoscopic retrograde cholangiopancreatography; d: days; h: hours; PD: percutaneous drainage; F: female; M: male; LBP: low blood pressure (hypotension); OLT: orthotopic liver transplant; NA: not available in the article.
Please cite this article as: de la Maza Ortiz J, García Mulas S, Ávila Alegría JC, García Lledó J, Pérez Carazo L, Merino Rodríguez B, et al. Hematoma subcapsular hepático tras colangiopancreatografía retrógrada endoscópica. Una complicación rara y con elevada morbimortalidad. Gastroenterol Hepatol. 2019;42:23–27.