Inflammatory bowel disease (IBD) is a chronic and relapsing disorder with significant medical, social and financial impacts. IBD patients require continuous follow-up, and healthcare resource use in this context increases over time. In the last decade, telemedicine has influenced the treatment of chronic diseases like IBD via the application of information and communication technologies to provide healthcare services remotely. Telemedicine and its various applications (telemanagement, teleconsulting and tele-education) enable closer follow-up and provide education resources that promote patient empowerment, encouraging treatment optimisation over the entire course of the disease. We describe the impact of using telemedicine on IBD health outcomes and discuss the limitations of implementing these systems in the real-life management of IBD patients.
La enfermedad inflamatoria intestinal (EII) es una dolencia crónica y recidivante con un importante impacto sanitario, social y económico. Los pacientes con EII requieren un seguimiento continuo y el uso de recursos sanitarios en este contexto está aumentando progresivamente. En la última década, la telemedicina ha transformado el manejo de enfermedades crónicas como la EII mediante la aplicación de atención sanitaria a distancia a través de las tecnologías de la información y la comunicación. Las diferentes aplicaciones de la telemedicina (telemonitorización, teleconsulta y teleeducación) favorecen un seguimiento más estrecho, además de promover la autonomía del paciente y mejorar el conocimiento de su enfermedad, lo que permite optimizar el tratamiento en cada momento evolutivo de la enfermedad. En esta revisión se describe el impacto de las aplicaciones de la telemedicina sobre los resultados en salud de los pacientes con EII, así como las limitaciones para su implantación en la vida real.
Because it is a chronic condition, inflammatory bowel disease (IBD) has significant medical, social and economic repercussions, particularly as it tends to affect young people at the peak of their personal and professional activities. This is why IBD patients require continuous and personalised follow-up to control disease activity and prevent medium- and long-term complications, which give rise to greater sick leave from work and school.1 The last decade has seen changes to information and communication technology (ICT) systems to support the more efficient provision of medical services, known as eHealth. These technologies are being applied in different ways, from online information services (institutional websites and portals) and computer applications (hospital information systems) to medical services (telemedicine).2 Telemedicine uses ICT to offer remote healthcare services without the need for face-to-face contact with the patient. Monitoring chronic diseases like IBD using programmes based on different telemedicine applications could be cost-effective at a time when national health systems are facing funding and sustainability challenges.3 Until now, telemedicine has been used to facilitate patient access to medical services, promoting closer monitoring and better communication between IBD patients and healthcare professionals.4 It is well known that the patient's active participation in controlling their disease increases their knowledge of the condition and promotes autonomy and greater treatment adherence. The purpose of this review is to describe the various telemedicine applications that have been used in IBD, patient acceptance of their use and their impact on health outcomes (disease activity, quality of life, treatment adherence, knowledge of the disease and healthcare costs). Based on these concepts, multiple useful telemedicine resources have been developed and applied to IBD, taking into account the physical limitations of each site in which they are used, the areas to which they are applied and the purpose of their use. This review focuses on the three telemedicine applications used in studies published to date in the field of IBD: telemonitoring, teleconsultation and tele-education5 (Table 1).
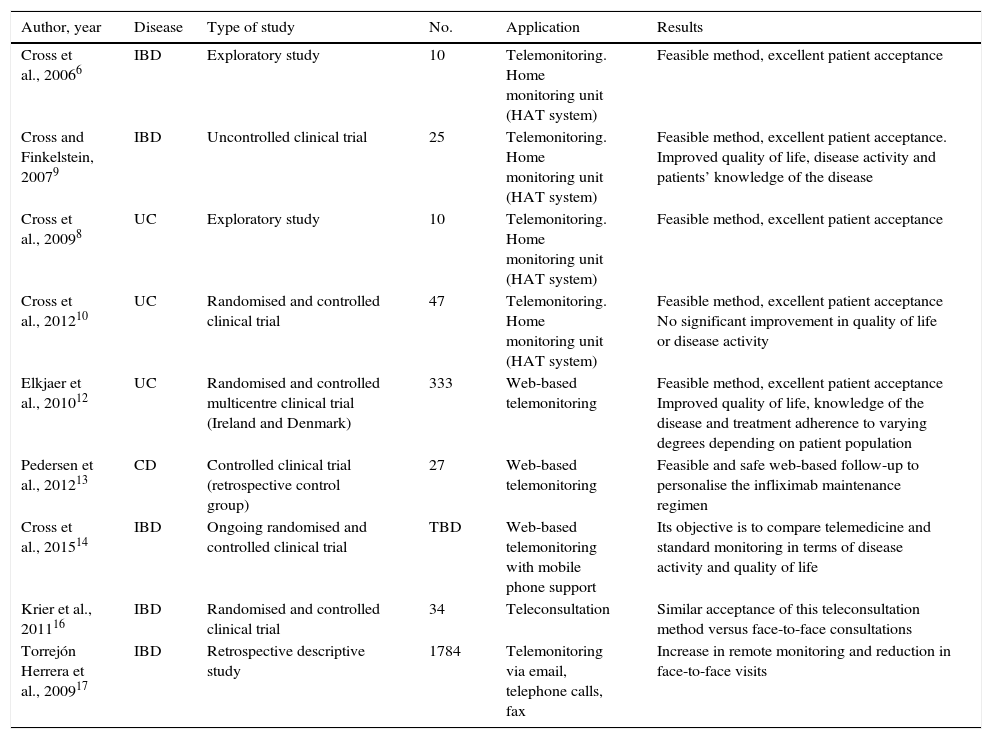
Results of using the different telemedicine applications in inflammatory bowel disease.
| Author, year | Disease | Type of study | No. | Application | Results |
|---|---|---|---|---|---|
| Cross et al., 20066 | IBD | Exploratory study | 10 | Telemonitoring. Home monitoring unit (HAT system) | Feasible method, excellent patient acceptance |
| Cross and Finkelstein, 20079 | IBD | Uncontrolled clinical trial | 25 | Telemonitoring. Home monitoring unit (HAT system) | Feasible method, excellent patient acceptance. Improved quality of life, disease activity and patients’ knowledge of the disease |
| Cross et al., 20098 | UC | Exploratory study | 10 | Telemonitoring. Home monitoring unit (HAT system) | Feasible method, excellent patient acceptance |
| Cross et al., 201210 | UC | Randomised and controlled clinical trial | 47 | Telemonitoring. Home monitoring unit (HAT system) | Feasible method, excellent patient acceptance No significant improvement in quality of life or disease activity |
| Elkjaer et al., 201012 | UC | Randomised and controlled multicentre clinical trial (Ireland and Denmark) | 333 | Web-based telemonitoring | Feasible method, excellent patient acceptance Improved quality of life, knowledge of the disease and treatment adherence to varying degrees depending on patient population |
| Pedersen et al., 201213 | CD | Controlled clinical trial (retrospective control group) | 27 | Web-based telemonitoring | Feasible and safe web-based follow-up to personalise the infliximab maintenance regimen |
| Cross et al., 201514 | IBD | Ongoing randomised and controlled clinical trial | TBD | Web-based telemonitoring with mobile phone support | Its objective is to compare telemedicine and standard monitoring in terms of disease activity and quality of life |
| Krier et al., 201116 | IBD | Randomised and controlled clinical trial | 34 | Teleconsultation | Similar acceptance of this teleconsultation method versus face-to-face consultations |
| Torrejón Herrera et al., 200917 | IBD | Retrospective descriptive study | 1784 | Telemonitoring via email, telephone calls, fax | Increase in remote monitoring and reduction in face-to-face visits |
Telemonitoring is the branch of telemedicine dedicated to the remote diagnosis, treatment, follow-up and education of the patient. Its implementation requires an appropriate technological infrastructure based on effective communication systems to facilitate the acquisition, storage and transmission of images and sound in real time. This type of telemedicine can be implemented in two basic ways: one method based on the use of a home telemanagement system (i.e. that requires home installation) and the other that operates over web-based systems.
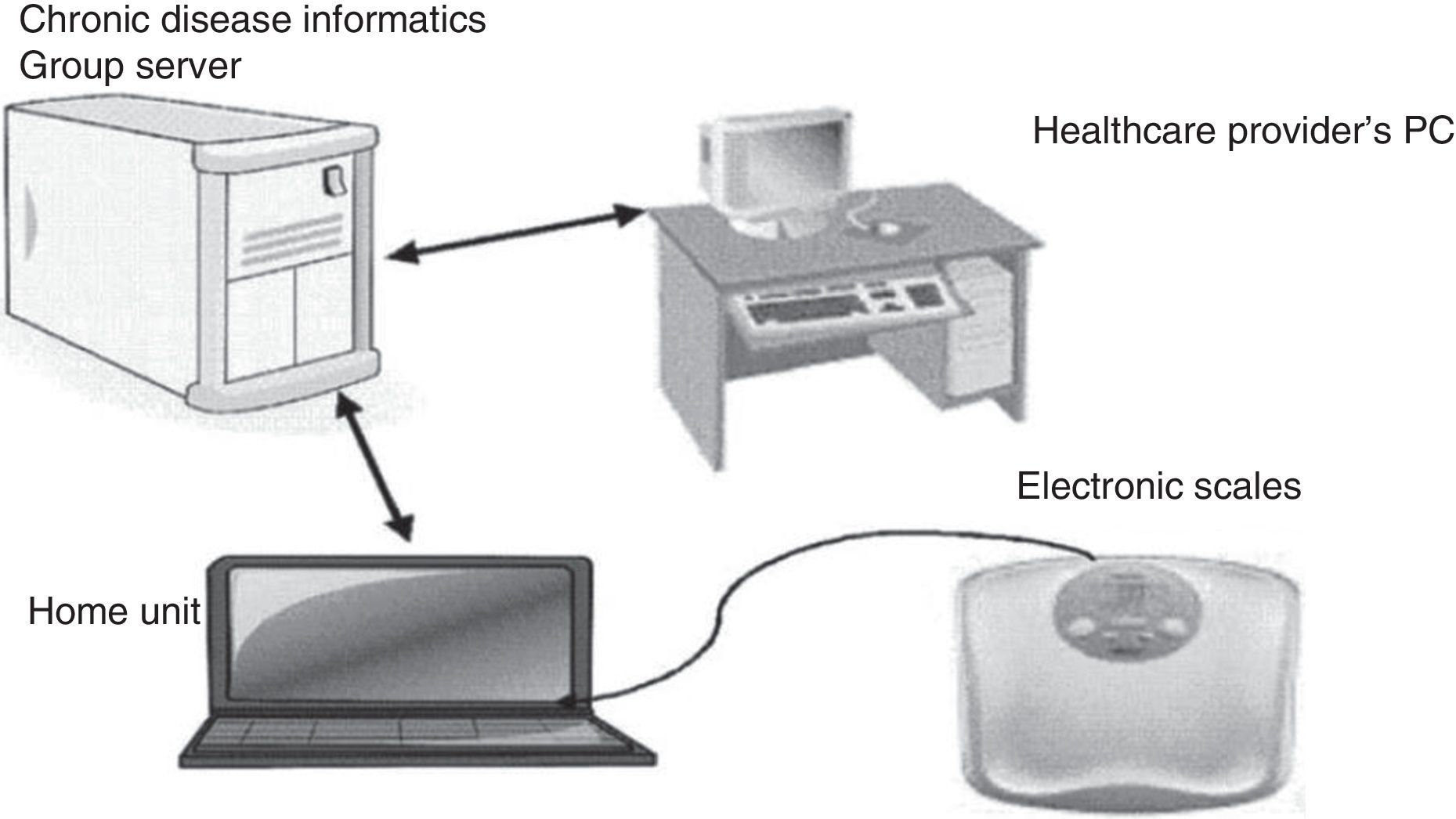
Home telemanagement systemCross et al. were among the first to use ICT in adult patients with IBD, primarily ulcerative colitis (UC), although some of their studies also included patients with Crohn's disease and indeterminate colitis. They developed a home automated telemanagement system (HAT system) based on a three-station home unit, namely a laptop to collect patient data. These data are subsequently sent to a support server that connects to the healthcare provider's computer. The healthcare provider's computer then generates profiles with different warning levels for each patient in accordance with the data collected from an online portal6 (Fig. 1).
Telemonitoring system for patients with inflammatory bowel disease.
Adapted from Cross et al.6
The first two pilot studies assessed acceptance of this monitoring system in 10 and 23 patients with IBD, respectively. All the patients from both studies found it easy to use, and also gained greater knowledge of their condition.6,7 Another exploratory study on 10 patients with UC produced similar results.8
To assess the acceptability of the system and medium-term compliance, another six-month study involving 25 patients was conducted. 91% of patients completed the weekly questionnaires and adhered to their usual treatment, while 84% of patients achieved adherence to their prescribed medication in excess of 80%. This study found better treatment adherence compared to that previously reported for patients with IBD, which coincided with a trend towards improved disease activity and quality of life and a statistically significant improvement in knowledge of the disease.9
Given these good results, it was predicted that the HAT system would be feasible for the remote monitoring of these patients. To confirm this hypothesis, a randomised and controlled clinical trial was designed that included 47 patients with mild-moderate ulcerative colitis. 25 patients were monitored with the HAT system while the remaining 22 patients formed the control group, attending their usual face-to-face appointments and provided with printed educational programmes and personalised action plans to make the two groups more comparable. Despite the favourable results in the assessed endpoints, the follow-up drop-out rate was higher in the experimental group and no statistically significant differences in disease activity or quality of life were found between the two groups after 12 months of follow-up.10
Online systemsOnline telemonitoring programs are easy to use and are cheaper than methods that require home installation, like the HAT system.
The Elkjaer et al. group was the first to assess the web-based “constant care” follow-up concept. The web-based system was initially validated in a pilot study that included 21 patients with UC, observing increased knowledge of the disease and patient autonomy.11 On this basis, a randomised and controlled clinical trial was designed that included 333 patients with UC administered 5-aminosalicylic acid (5-ASA) in hospitals in Denmark and Ireland. The experimental group was monitored online while the control group attended usual face-to-face appointments for 12 months. The objectives of the study were to assess follow-up compliance, knowledge of the disease, quality of life and disease activity, as well as safety and costs associated with disease control. In this case, patients entered their clinical and analytical data on a web-based platform accessed via the Internet. Similar to the platform proposed by Cross et al., changes in the patient's follow-up plan or treatment were established based on the data collected. After 12 months of follow-up, 88% of the online group in Denmark considered the system to be feasible and a statistically significant improvement in compliance and quality of life was seen compared to the control group. Approximately 50% of patients from both groups had at least one flare-up, but duration was significantly less in the online group. This was correlated with the use of high doses of 5-ASA in 100% of patients in the experimental group versus 10% in the control group. In Ireland, 88% of patients also considered the web-based system to be feasible, treatment adherence at four weeks was significantly higher and the duration of flare-ups was shorter in the online group. However, in this population only 15% of patients from the experimental group were treated with high-dose 5-ASA versus 10% in the control group. Furthermore, web-based follow-up did not lead to improved quality of life or knowledge of the disease. With the use of the telemonitoring system, the Danish population had fewer visits to the emergency department, more consultations over the phone and via email and a saving of €189 per patient per year, while these same changes were not seen in the Irish group. In conclusion, this study found the web-guided approach to be feasible, safe and cost-effective despite population-based differences in its reproducibility.12
A similar web-based system was used by Pedersen et al. in a 52-week study that included 27 patients with Crohn's disease treated with anti-tumour necrosis factor (infliximab) to personalise the treatment interval. The patients were monitored online in addition to regular face-to-face appointments, and the results were compared with the control group that was included retrospectively. The experimental group saved €699 per patient per year, but no statistically significant differences in quality of life or disease activity were observed.13
Our research group has developed a web-based platform called TECCU (Telemonitorización en la Enfermedad de Crohn y Colitis Ulcerosa, Telemonitoring in Crohn's Disease and Ulcerative Colitis) to manage patients with highly complex IBD who start treatment with systemic corticosteroids, immunosuppressants and/or biological drugs. A randomised and controlled clinical trial with three parallel arms comparing this remote monitoring system with specialised nursing telephone support and with a control group of routine face-to-face care has recently been completed. The preliminary results show that the TECCU platform is a safe and effective tool for remotely monitoring the activity of patients with highly complex inflammatory bowel disease while also representing a saving in face-to-face outpatient appointments and nurse-led telephone consultations.
Along similar lines, Cross et al. are currently conducting a randomised, multicentre clinical trial to assess a web-based telematic monitoring system for patients with inflammatory bowel disease (TELE-IBD) using text messages sent to mobile phones. A controlled study with three parallel arms was designed (weekly TELE-IBD, fortnightly TELE-IBD and standard control group), which included patients with IBD who had experienced at least one flare-up in the last two years. The objective of the trial is to assess the system's feasibility to monitor disease activity and quality of life after 12 weeks of follow-up and to address the problems generated by the HAT system used in their previous studies.14
The patient enrolment period for both trials ended in June and July 2016, respectively. The efficacy and safety results associated with these remote web-based monitoring systems will soon be available.
TeleconsultationThis application of telemedicine uses ICT to enable healthcare professionals to contact their patients in real time, without them having to attend the medical centre.15 Teleconsultation systems promote comprehensive and rapid patient care as well as self-care through educational programmes.
Video consultationKrier et al. used a video consultation method called the Collaborative System to enable healthcare professionals of various specialisms to communicate with their patients from their medical centre. These video conferences offered patients multidisciplinary follow-up from a medical centre without direct access to the various subspecialties involved in the treatment of patients with IBD. A randomised and controlled clinical trial involving 34 patients with IBD was designed to compare the treatment of patients with the video consultation system versus face-to-face consultation at the hospital. Although the new video consultation system was broadly accepted by the patients, no differences were found in terms of satisfaction with the care received or perceived skill level of the doctor compared to routine face-to-face consultations.16
New teleconsultation programmesThe development of new remote monitoring methods has given rise to the implementation of teleconsultation programmes in specialist IBD units.
The Hospital Universitari Vall d’Hebron Crohn's-Colitis Care Unit (UACC) published its experience with a remote care system used at the unit for the first nine years (1999–2007). The unit implemented a continuous care model for patients with IBD that used remote means of communication (primarily telephone, fax and email) supported by a website (http://www.ua-cc.org), in addition to routine face-to-face consultations. It involved a multidisciplinary team (nursing staff, doctors specialising in IBD and other specialists) to provide comprehensive care and promote patient self-care through educational programmes. This study retrospectively collected activity data generated from both face-to-face and remote consultations over a nine-year period. A progressive increase in remote consultations and the number of patients monitored using this system was recorded, with a considerable reduction in face-to-face visits. It was concluded that the UACC offers continuous and dynamic care that promotes patient participation and remote monitoring while optimising the healthcare of IBD patients.17
In a similar vein, an international collaborative project between six Nordic countries was recently launched to provide remote healthcare services via the Internet, smartphones and video conferences. This programme includes 10 subprojects applied to 10 different medical specialties, including IBD. The aim of this model is the sustainable development of eHealth using telematic means to reach rural and remote areas and regions in the North of Europe that have limited access to medical care.18
Tele-educationTele-education is another key application in the field of telemedicine for the treatment of patients with IBD. It is usually Internet-based thanks to the use of high-quality web portals and online courses, or as part of telemonitoring programmes.19,20 Most studies on remote and web-based monitoring programmes, as well as the teleconsultation systems described above, have included remote educational elements to improve patients’ knowledge of the disease and promote self-care.7,17 However, an online survey of IBD specialist gastroenterologists in Europe found that only 56% had access to educational resources at their hospital and just 34% had established patient support programmes, thus representing an opportunity to improve standardised access to treatment and quality of care in our setting.21 There are currently 27 integrated IBD units participating in Spain's educational platform www.educainflamatoria.com, which was launched in 2013. Through a forum that facilitates interaction with a multidisciplinary medical team, this website offers educational resources and support programmes to patients to complement their medical care.
DiscussionIBD morbidity requires close monitoring that can interfere in the social and professional lives of affected patients. In this regard, telemedicine is a new tool that offers a range of potential applications to support patient care. These new technologies provide patient follow-up that is adapted to the clinical course of the disease at any given time, whilst also fostering patient autonomy and self-care and improving their knowledge of the disease.
Telemonitoring and teleconsultation systems are the main telemedicine applications to have been evaluated in this context. Cross et al. were the first to develop a remote telemonitoring platform (HAT) using a home installation system. The various studies conducted found this remote monitoring method to be feasible and acceptable to patients. However, the main drawback of the HAT system was the need to install and potentially repair it in the home, which could affect its uptake and persistent use. This explains the higher long-term drop-out rate of controlled patients recorded in these studies using this follow-up method.8–10 To address these problems, the Elkjaer research group developed a web-based monitoring system that was easier to maintain and cheaper than the HAT system. This remote monitoring system was validated and found to improve quality of life, disease activity and knowledge of the disease compared to routine face-to-face consultations to varying degrees depending on the population.12
Teleconsultation systems promote doctor–patient communication and collaboration amongst healthcare professionals, particularly where physical access to specialised care is difficult, with similar patient acceptance and satisfaction levels as face-to-face consultations. In this regard, a British study evaluating the preferences and needs of IBD patients found that they prefer flexible follow-up with integrated remote treatment and self-care.22 The advantages reported in the studies conducted to date have led to the development of teleconsultation platforms in IBD units, both in Spain and around the world.17,18 These have focused on the provision of medical services in both urban and rural areas to promote and improve knowledge of the disease among patients and healthcare professionals alike. What is more, published pilot studies on the management of IBD patients using telemonitoring and teleconsultation systems have found them to be cost-effective, although to date no study has assessed this potential benefit as its primary endpoint.12,13
Despite the advantages and opportunities that the different telemedicine applications offer, there are barriers to their expansion in current health systems. Firstly, a lack of well-designed studies with an appropriate sample size to reproduce the results of the pilot studies (both patients in remission as well as with active inflammatory bowel disease) gives rise to a lack of confidence in their actual utility in clinical practice. What is more, secure servers are required to guarantee data confidentiality and not all institutions have the necessary infrastructure or financial resources, particularly given that the implementation of telemedicine demands a very high initial cost, both in financial terms as well as the structural changes involved. These problems could be partially offset by installing web-based systems, which are cheaper and easy to use. It is also important to select patients who are suited to this type of follow-up and offer other monitoring methods to those less capable of using these technologies.
In conclusion, the management of IBD patients using telemedicine applications, like telemonitoring and teleconsultation, is safe, feasible and broadly accepted by patients. These remote monitoring systems increase patient autonomy and their knowledge of the disease and improve treatment adherence. However, controlled studies are needed that evaluate the real efficacy of telemonitoring in inflammatory control and the benefits of this application in patients with highly complex IBD. With this in mind, our research group has developed TECCU, a remote monitoring platform that consists of a web-based follow-up program accessed by computer, tablet or mobile phone for patients with complex IBD who require systemic corticosteroids, immunosuppressants and/or biological drugs. This application has been found to be a safe and effective way of remotely monitoring highly complex patients and is currently in the integration phase to validate the platform for all patient profiles, both active and in remission. Future studies are needed to establish whether remote monitoring is cost-effective in clinical practice and to ascertain whether using the different telemedicine applications could change the disease's clinical course compared to conventional face-to-face follow-up.
FundingThis study was supported by grants from the Instituto de Salud Carlos III [Carlos III Health Institute]-Medical Research Fund (FIS PI12/00277) and was co-financed by the European Regional Development Fund (ERDF).
Conflict of interestThe authors have no conflicts of interest.
Please cite this article as: Aguas M, Del Hoyo J, Faubel R, Valdivieso B, Nos P. Telemedicina en el manejo de pacientes con enfermedad inflamatoria intestinal. Gastroenterol Hepatol. 2017;40:641–647.