Analizar el efecto de la demora atribuible al sistema sanitario en una cohorte consecutiva de pacientes diagnosticados de forma ambulatoria de cáncer colorrectal (CCR) en el área sanitaria de Ourense.
Pacientes y métodosEstudio observacional de cohortes retrospectivo en el que se incluyeron los pacientes diagnosticados entre 2009 y 2017. Se definió la demora atribuible al sistema sanitario como el tiempo entre la primera consulta por síntomas y la confirmación diagnóstica. Se determinó si existía una relación independiente entre la demora diagnóstica y el CCR estadio IV mediante una regresión logística. Finalmente, realizamos una regresión de riesgos proporcionales para determinar qué variables se asociaban con la mortalidad global y por CCR.
ResultadosSe incluyeron 575 pacientes (hombres 64.5%, edad 71.9±11.5 años) con una demora atribuible al sistema sanitario de 115±153 días. Ninguna de las variables analizadas se asoció con el estadio tumoral al diagnóstico. Durante un seguimiento de 30.6±21 meses fallecieron 121 pacientes (79.3% en relación al CCR). Las variables asociadas de forma independiente con la mortalidad atribuible al CCR fueron el estadio IV al diagnóstico (HR 50.65, IC 95% 12.28-209), la edad (HR 1.04, IC 95% 1.02-1.05) y la solicitud de la colonoscopia desde Atención Primaria (HR 0.55, IC 95% 0.37-0.88).
ConclusionesLa demora diagnóstica atribuible al sistema sanitario no se relacionó ni con el estadio ni con el pronóstico del CCR. Sin embargo, la solicitud de la colonoscopia desde Atención Primaria se asoció a una reducción en el riesgo de mortalidad.
To analyse the effect of a delay attributable to the healthcare system on a consecutive cohort of outpatients diagnosed with colorectal cancer in the healthcare area of Ourense (Spain), covering 274,000 inhabitants.
Patients and MethodsWe performed a retrospective cohort study that included patients diagnosed between 2009 and 2017. Delay attributable to the healthcare system was defined as the time between the first consultation with symptoms and the diagnostic confirmation. A logistic regression model was performed to evaluate the relationship between stage IV CRC and diagnostic delay. To analyse which variables were associated independently with overall mortality and mortality due to CRC we used a Cox regression model.
Results575 patients were included (men 64.5%, age 71.9±11.5 years), with a delay attributable to the healthcare system of 115±153 days. None of the variables analysed were associated with tumour stage at diagnosis. With a mean follow-up of 30.6±21 months, 121 patients died, 79.3% due to CRC. The variables independently associated with CRC-related mortality were metastatic CRC (HR 50.65, 95% CI 12.28–209), age (HR 1.04, 95% CI 1.02–1.05) and colonoscopy requested from the primary healthcare level (HR 0.55, 95% CI 0.36–0.88).
ConclusionsDiagnostic delay attributable to the healthcare system is not related to the prognosis or stage of CRC. However, a direct referral to colonoscopy from the primary healthcare level reduces the risk of mortality in our patients.
Colorectal cancer (CRC) is the third most common cancer worldwide and the second leading cause of cancer-related death,1 which makes it one of the main current health challenges in the western world. Its main prognostic factor is the stage at diagnosis,2 which is why it is vitally important to detect the tumour in the early phases of the disease. There are two strategies to achieve this goal: population screening for CRC3–5 and early diagnosis in symptomatic patients. The diagnostic process in symptomatic patients is complex. It is determined mainly by the high prevalence of gastrointestinal symptoms in the general population, normally related to benign pathology and the high number of health resources involved in the evaluation of these patients. The total time that this process takes is called diagnostic delay.
Numerous studies6–14 have looked for the causes of diagnostic delay in its different stages. However, the data which relate the diagnostic and/or therapeutic delay to survival15,16 or the tumour stage at diagnosis17 are not conclusive and are even contradictory. One study related the delay between the first consultation and the start of treatment after more than 60 days with a worse prognosis in rectal tumours.15 Furthermore, a prospective study carried out in primary care determined that patients with warning symptoms and diagnostic delays of less than five weeks had a lower mortality rate.18 In contrast, in patients with symptoms who fulfilled fast-track criteria of the National Institute for Health and Care Excellence, a delay of less than thirty days improved the prognosis.19 Being able to definitively establish a prognostic relationship with the length of delay would reinforce the need to optimise the speed of diagnosis within our health systems.
The objective of this study was to analyse the effect of the delay attributable to the health system in the tumour stage at diagnosis and in the prognosis of a retrospective cohort of patients with a diagnosis of CRC assessed on an outpatient basis in our clinic. In addition, we sought to determine which factors are associated with the prognosis of patients diagnosed with CRC on an outpatient basis.
Patients and methodsPopulation and periodA retrospective observational cohort study was performed in which data were collected from patients diagnosed with CRC on an outpatient basis in the Gastrointestinal Tests Unit and referred to the High Risk and Gastrointestinal Oncology Clinic of the Hospital Universitario de Ourense (Ourense University Hospital) between 2009 and 2017. The study was assessed and approved by the site’s Ethics Committee.
All patients over the age of 18 diagnosed with CRC by means of a colonoscopy requested by their primary care doctor or by a colonoscopy requested by the hospital specialist physician after a referral from primary care or from the accident and emergency department in light of symptoms suggestive of CRC were included. The request for colonoscopy in symptomatic patients is based on the indications and levels of priority of the colonoscopy of the Servizo Galego de Saúde [Galician Health Service], which have already been reported. The family medicine specialist had the possibility both of requesting the colonoscopy directly based on the established items or referring to the clinic of the digestive system specialist.20
The following were considered to be exclusion criteria: 1) absence of pathology compatible with adenocarcinoma; 2) referral of the patient from anywhere other than primary care: screening programme, monitoring of polyps, diagnosis outside the public health system; 3) opportunistic screening or screening due to family history; and 4) hospital admission.
Diagnostic delay attributable to the health systemThe delay attributable to the health system was defined as the time between the first contact with the health system due to symptoms and diagnostic confirmation. To establish this, the following data were collected: the date of the first consultation in primary care or hospital A&E department; and the date the colonoscopy was performed in which the diagnosis was confirmed. The delay time was analysed both as a continuous quantitative variable and qualitative variable establishing three periods: less than 30 days, between 31 and 180 days, and more than 180 days. In the case of referral to hospital care clinics, the referral and consultation dates were collected. Finally, the date of the colonoscopy request and the requesting level of care -primary care or hospital care- were collected.
In addition, data were collected related to the demographic variables, the location of the tumour and the tumour stage at diagnosis using the 7th version of the TNM staging system21 and, finally, the patient's health at the time of collecting the data and the cause of death.
Statistical analysisFirst of all, a descriptive analysis of the data obtained was performed: the quantitative variables were represented by means and standard deviations, while the qualitative variables were represented in absolute numbers and frequencies. To determine the existence of statistically significant relationships, the chi-square test was used for qualitative variables and the Student’s t-test for quantitative variables.
To determine if the diagnostic delay was associated with the stage at diagnosis, a logistic regression was performed, controlling for the independent variables. The relationship between the different variables and the presence of metastatic disease at diagnosis was expressed as odds ratio (OR) and its 95% confidence interval (95% CI). Finally, it was analysed which variables were independently associated both with all-cause mortality and with mortality attributable to CRC by proportional hazards regression. The association was expressed as hazard ratio (HR) and 95% CI.
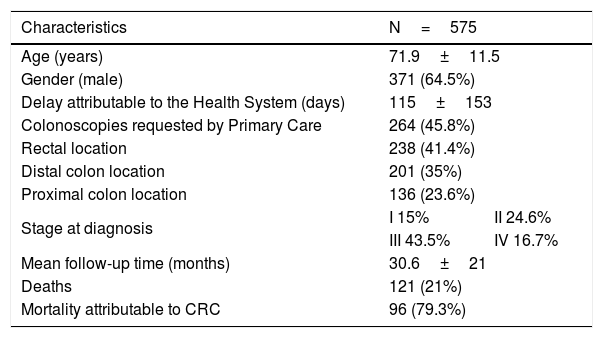
ResultsData descriptionIn the period analysed, 3862 patients with colorectal lesions were referred to the High Risk and Gastrointestinal Oncology Clinic, of whom 575 patients fulfilled the criteria to join the study and from whom it was possible to obtain all the necessary data. As shown in Table 1, 371 (64.5%) of the patients recruited were male. The mean age of our sample was 71.9±11.5 years. The diagnostic delay attributable to the health system was 115±153 days. In 145 patients (25.2%), the delay was less than one month, in 326 (56.7%) it was between one and six months and in 104 (18.1%), the diagnostic delay was more than 180 days.
Characteristics of the sample of patients obtained in our study.
| Characteristics | N=575 | |
|---|---|---|
| Age (years) | 71.9±11.5 | |
| Gender (male) | 371 (64.5%) | |
| Delay attributable to the Health System (days) | 115±153 | |
| Colonoscopies requested by Primary Care | 264 (45.8%) | |
| Rectal location | 238 (41.4%) | |
| Distal colon location | 201 (35%) | |
| Proximal colon location | 136 (23.6%) | |
| Stage at diagnosis | I 15% | II 24.6% |
| III 43.5% | IV 16.7% | |
| Mean follow-up time (months) | 30.6±21 | |
| Deaths | 121 (21%) | |
| Mortality attributable to CRC | 96 (79.3%) | |
In total, 45.8% of the colonoscopies were requested directly by primary care. The location of the tumour was rectal in 238 patients, of the sigmoid and descending colon in 201, and of the transverse colon and caecum in 136 patients. The stage at diagnosis was: stage I 15%, stage II 24.6%, stage III 43.5% and stage IV 16.7%. The mean follow-up was 30.6±21 months. During this period, 21% (121) of the patients died. Death was attributed to CRC in 79.3% of these patients.
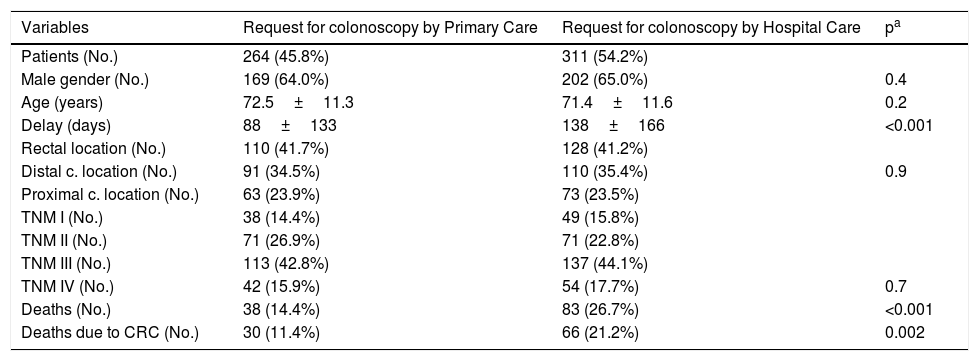
Variables related to diagnostic delayTable 2 shows the characteristics of the patients according to who requested the colonoscopy. The diagnostic delay time was not related to gender, the location of the tumour or the stage at diagnosis, although it was related to the level at which the colonoscopy was requested. The delay in patients with colonoscopies requested by primary care was 88±133 days. In patients in whom the colonoscopy was requested by hospital care, the total diagnostic delay was 138±166 days (p<0.001). In these patients, the length of delay before the first hospital appointment was 83±129 days, and the delay in the conduct of the colonoscopy was 56±98 days.
Characteristics of the patients according to the care level requesting the colonoscopy.
| Variables | Request for colonoscopy by Primary Care | Request for colonoscopy by Hospital Care | pa |
|---|---|---|---|
| Patients (No.) | 264 (45.8%) | 311 (54.2%) | |
| Male gender (No.) | 169 (64.0%) | 202 (65.0%) | 0.4 |
| Age (years) | 72.5±11.3 | 71.4±11.6 | 0.2 |
| Delay (days) | 88±133 | 138±166 | <0.001 |
| Rectal location (No.) | 110 (41.7%) | 128 (41.2%) | 0.9 |
| Distal c. location (No.) | 91 (34.5%) | 110 (35.4%) | |
| Proximal c. location (No.) | 63 (23.9%) | 73 (23.5%) | |
| TNM I (No.) | 38 (14.4%) | 49 (15.8%) | |
| TNM II (No.) | 71 (26.9%) | 71 (22.8%) | |
| TNM III (No.) | 113 (42.8%) | 137 (44.1%) | |
| TNM IV (No.) | 42 (15.9%) | 54 (17.7%) | 0.7 |
| Deaths (No.) | 38 (14.4%) | 83 (26.7%) | <0.001 |
| Deaths due to CRC (No.) | 30 (11.4%) | 66 (21.2%) | 0.002 |
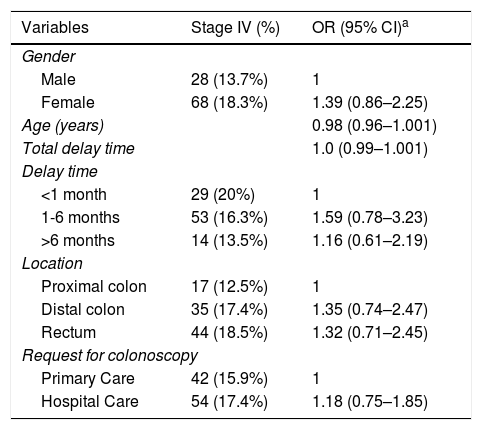
In the analysis of the effect of the delay on the stage at diagnosis, no statistically significant differences were found in the proportion of stage IV tumours between the patients diagnosed with delays of less than one month (20%), between one and six months (16.3%) and more than six months (13.5%). There was also no correlation found between the length of diagnostic delay and advanced tumour stage. Table 3 shows the logistic regression results to determine if any of the baseline variables were related to an advanced tumour stage (TNM IV) at diagnosis. No relationship was identified with any of the independent variables: gender, age, location of the tumour or request for colonoscopy by primary care.
Association between independent variables and the tumour stage (TNM IV) at diagnosis.
| Variables | Stage IV (%) | OR (95% CI)a |
|---|---|---|
| Gender | ||
| Male | 28 (13.7%) | 1 |
| Female | 68 (18.3%) | 1.39 (0.86–2.25) |
| Age (years) | 0.98 (0.96–1.001) | |
| Total delay time | 1.0 (0.99–1.001) | |
| Delay time | ||
| <1 month | 29 (20%) | 1 |
| 1-6 months | 53 (16.3%) | 1.59 (0.78–3.23) |
| >6 months | 14 (13.5%) | 1.16 (0.61–2.19) |
| Location | ||
| Proximal colon | 17 (12.5%) | 1 |
| Distal colon | 35 (17.4%) | 1.35 (0.74–2.47) |
| Rectum | 44 (18.5%) | 1.32 (0.71–2.45) |
| Request for colonoscopy | ||
| Primary Care | 42 (15.9%) | 1 |
| Hospital Care | 54 (17.4%) | 1.18 (0.75–1.85) |
CI: confidence interval; OR: odds ratio.
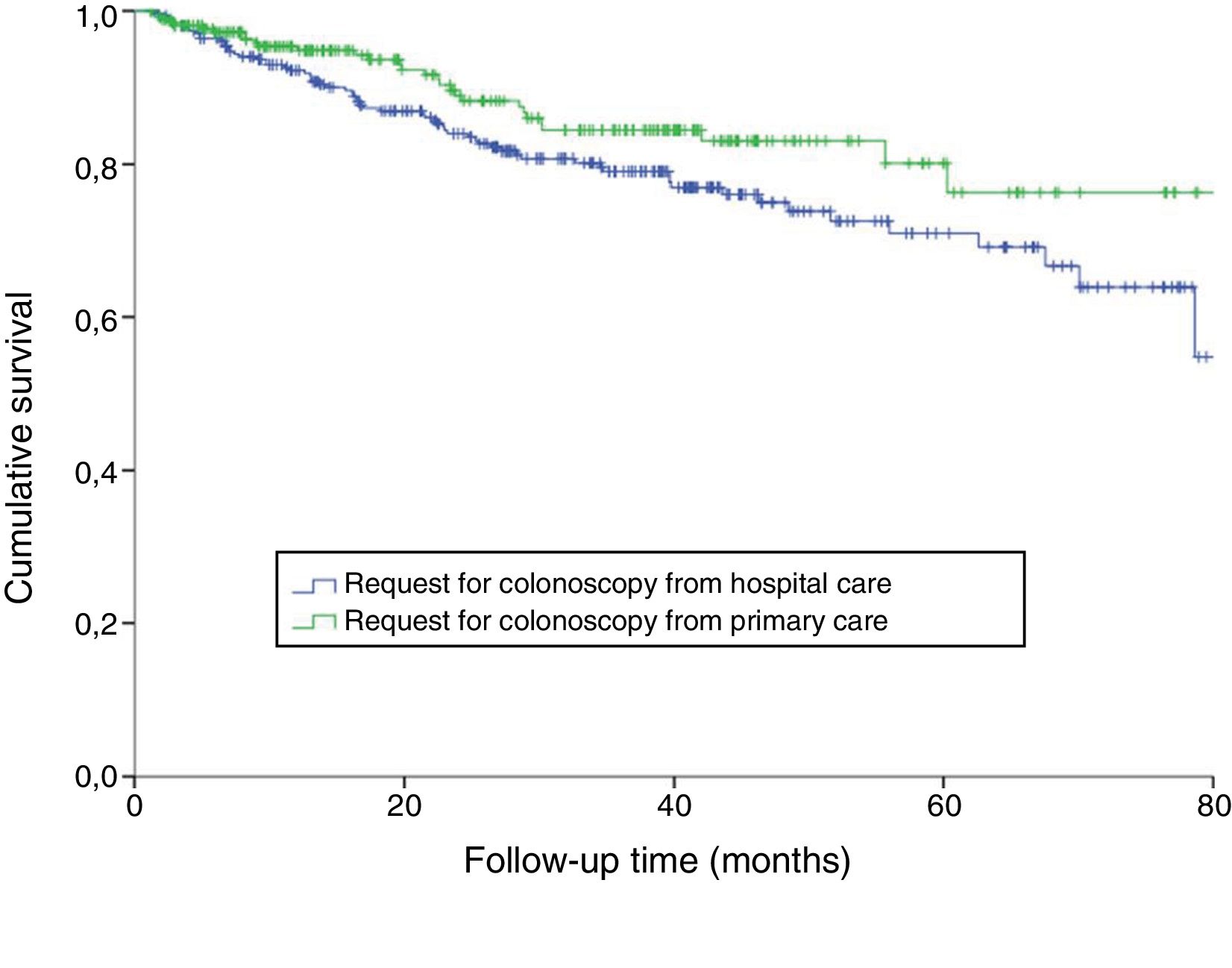
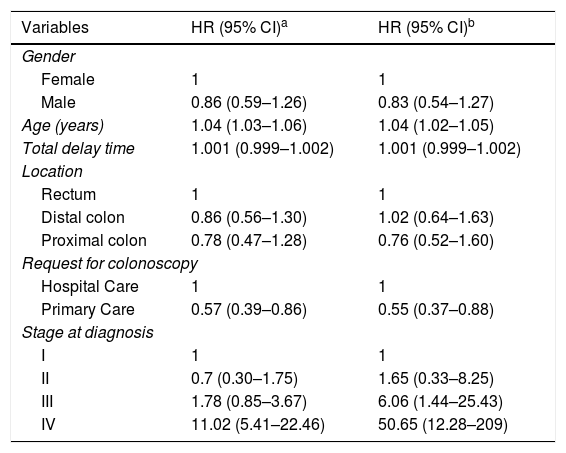
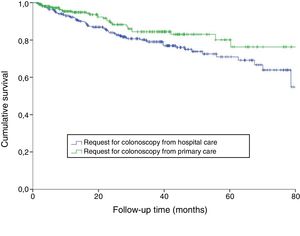
Table 4 shows the relationship between the independent variables and all-cause mortality. Three variables which were independently associated with the risk of all-cause mortality were identified: age (HR 1.04; 95% CI, 1.03–1.06), tumour stage IV (HR 11.02; 95% CI 5.41–22.46) and, finally, the request for colonoscopy by primary care (HR 0.57; 95% CI 0.39-0.86) (Fig. 1).
Variables associated with mortality, both all-cause mortality and associated with colorectal cancer, in the multivariate proportional hazards regression.
| Variables | HR (95% CI)a | HR (95% CI)b |
|---|---|---|
| Gender | ||
| Female | 1 | 1 |
| Male | 0.86 (0.59–1.26) | 0.83 (0.54–1.27) |
| Age (years) | 1.04 (1.03–1.06) | 1.04 (1.02–1.05) |
| Total delay time | 1.001 (0.999–1.002) | 1.001 (0.999–1.002) |
| Location | ||
| Rectum | 1 | 1 |
| Distal colon | 0.86 (0.56–1.30) | 1.02 (0.64–1.63) |
| Proximal colon | 0.78 (0.47–1.28) | 0.76 (0.52–1.60) |
| Request for colonoscopy | ||
| Hospital Care | 1 | 1 |
| Primary Care | 0.57 (0.39–0.86) | 0.55 (0.37–0.88) |
| Stage at diagnosis | ||
| I | 1 | 1 |
| II | 0.7 (0.30–1.75) | 1.65 (0.33–8.25) |
| III | 1.78 (0.85–3.67) | 6.06 (1.44–25.43) |
| IV | 11.02 (5.41–22.46) | 50.65 (12.28–209) |
CI: confidence interval; HR: hazard ratio.
Finally, it was specifically analysed which variables were associated with mortality attributable to CRC (Table 4). In this analysis, the three variables related to all-cause mortality were confirmed as being independently associated with mortality attributable to CRC: age (HR 1.04; 95% CI 1.02–1.05), CRC stage IV at diagnosis (HR 50.65; 95% CI 12.28–209) and request for colonoscopy by primary care (HR 0.55; 95% CI 0.37–0.88).
DiscussionSummary of findingsIn our study, no association was found between the diagnostic delay attributable to the health system and the prognosis of CRC. This relationship was not observed when grouping the delay into time intervals or when studying the delay as a whole. However, the request for colonoscopy by primary care was associated with a reduction in the risk of mortality in our patients, compared to requests by hospital care. This association does not seem to be related to the stage at diagnosis, as no such differences were found among the requesting levels. The other variables that were statistically significant as mortality risk factors were age and stage IV at diagnosis.
Similarities and differences with other studiesIn a recent population study in Canada,22 a diagnostic delay of 84 days (interquartile range of 39–223 days) was reported in 4115 symptomatic patients (with a non-urgent presentation). In this sample of patients, stage IV at diagnosis was 22%. These figures are similar to those of our study.
The absence of a prognostic relationship between the delay in diagnosis and CRC tumour stage are findings consistent with recent studies23 and meta-analyses17 in which patients with shorter diagnostic delays tend to present more advanced stages at diagnosis and, therefore, lower survival. These findings would support the hypothesis that the symptomatic stage of CRC is of short duration compared to the natural history of this disease.24 However, it will be difficult to precisely determine the speed of the tumour’s development, which is further hindered given the possible differences between the different oncogenic pathways. In our study, the rectal location of the tumour did not determine a shorter diagnostic delay, as occurred in other studies with a similar sample size, such as that carried out by Korsgaard et al.15 However, there are methodological differences, such as the use of different staging methods, or the definition of diagnostic delay, which was considered to be up to the start of treatment.
The association between patient age and the stage at diagnosis with CRC prognosis was already known.25 However, to date it had not been related with the request for colonoscopy by the primary care physician. It should be taken into account that the search for this relationship was not an objective of our study, meaning that other studies are required to confirm it.
Strengths and weaknessesAlthough we did not find a relationship between diagnostic delay and stage IV at diagnosis, we cannot rule out that this lack of statistical relationship may be related to a lack of statistical power. However, in the data analysed, the percentage of patients with metastatic stage at diagnosis was higher among patients with delays of less than one month. Therefore, one of the possible reasons for not detecting a relationship between the delay and the stage could be the clinical presentation of the advanced stages with warning symptoms. These symptoms would influence the direct request for colonoscopy, thereby reducing the delay in advanced stages, unlike patients with mild or intermittent symptoms, who are subjected more frequently to blood tests or preliminary studies. However, the exclusion of patients who were admitted during the diagnostic process would enable this bias to be controlled to a large extent, excluding patients with more severe symptoms. Likewise, patients with urgent, occlusive or sub-occlusive presentations and, therefore, with minimal delays in advanced stages, were excluded from our study. Finally, as it was a retrospective study, we were not able to collect the symptoms with which the diagnostic process started, nor the patient’s comorbidity.
Implications for physicians and managersThe individual attitude of patients with regard to their symptoms, and the search for medical assessment, are important factors to consider to reduce the overall diagnostic delay. The date of symptom onset was not collected in our study, as it was only intended to study the delay due to the health system. Although the length of delay in relation to the patient varies widely from subject to subject,7 it has also not been shown to influence the prognosis.16,17
Once the symptoms have been established, the prognostic influence demonstrated by the delay times is weak.17 This is reflected in our study in a similar distribution of stages in each delay period. The effect of rapid referral criteria in patients with a high suspicion of CRC on prognosis is controversial. These routes have been shown to associate certain warning symptoms and signs with the existence of a tumour. In this context, a delayed diagnosis seems to affect survival, particularly in delays of more than six months.18 In our study, patients were not differentiated by the priority of the colonoscopy, given the difficulty obtaining these data in our sample. Therefore, the symptoms do not seem to help in the objective of improving prognosis in patients with CRC, which is why the detection of CRC is of greater importance in pre-symptomatic periods.
In our study, a clear reduction in diagnostic delay times is shown when the colonoscopy is requested by the primary care physician, mainly because there are no intermediate delay times in the referral to the hospital specialist. Nevertheless, more than half of the colonoscopies in our study were requested by hospital care after the referral of the patient from primary care. The association detected between the prognosis and the request for colonoscopy by primary care is not related to the delay or to the stage at diagnosis. This association is probably related to overall care quality criteria. The use of protocols requesting complementary tests20 by primary care physicians would indicate better quality in the overall care of patients treated by these physicians.
ConclusionsOur study failed to detect a relationship between the diagnostic delay attributable to the health system and the metastatic stage at diagnosis or the survival of patients with a diagnosis of CRC. However, a reduction in the diagnostic delay attributable to the health system and greater survival in patients in whom the request for colonoscopy came directly by primary care was detected.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank the Instituto de Investigación Sanitaria Galicia Sur [Galicia South Health Research Institute].
Please cite this article as: Fernández-de Castro JD, Baiocchi Ureta F, Fernández González R, Pin Vieito N, Cubiella Fernández J. Efecto de la demora atribuible al sistema sanitario en el pronóstico del cáncer colorectal. Gastroenterol Hepatol. 2019;42:527–533.
A summary of this study was presented in the form of a poster communication at the twenty-first Annual Meeting of the Asociación Española de Gastroenterología [Spanish Association of Gastroenterology].