Turner syndrome is characterised by short stature, gonadal dysgenesis and typical phenotypic findings associated with partial or complete monosomy of the X chromosome.1 The clinical spectrum is very broad and it can be associated with hypothyroidism, autoimmune diseases, coarctation of the aorta, valvular heart disease, diabetes mellitus, etc. It is common for people with Turner syndrome to have hypertransaminasaemia, and this has classically been associated with toxicity from hormone therapy or hepatic steatosis caused by the associated factors; diabetes mellitus, dyslipidaemia, etc. There have been few documented cases of liver cirrhosis in these patients.
We present the case of a 24-year-old woman whose history included diagnosis at the age of 10 months with Turner's syndrome, as a result of her short stature. At the age of 4, because of deficiency, she began growth hormone treatment, which she continued for 12 years. As associated disorders, the patient had been diagnosed at the age of 7 with Hashimoto's thyroiditis, for which she was on replacement therapy with levothyroxine, and she had Gilbert's syndrome. She was started on oestrogen treatment at the age of 11 and later progesterone for the development of secondary sexual characteristics. In a follow-up analysis at the age of 21, an abnormal liver profile was detected, with hypertransaminasaemia and mild cholestasis (AST 43U/l, ALT 40U/l, GGT 139U/l, alkaline phosphatase 134U/l, total bilirubin 2.8mg/dl and conjugated bilirubin 0.8mg/dl). As it was initially attributed to oestradiol/norgestrel toxicity, that was replaced by ethinyloestradiol/drospirenone. However, when the abnormal liver function tests persisted, the patient was switched to levonorgestrel/ethinyloestradiol. When there continued to be no improvement in her liver parameters, she was referred to hepatology for assessment.
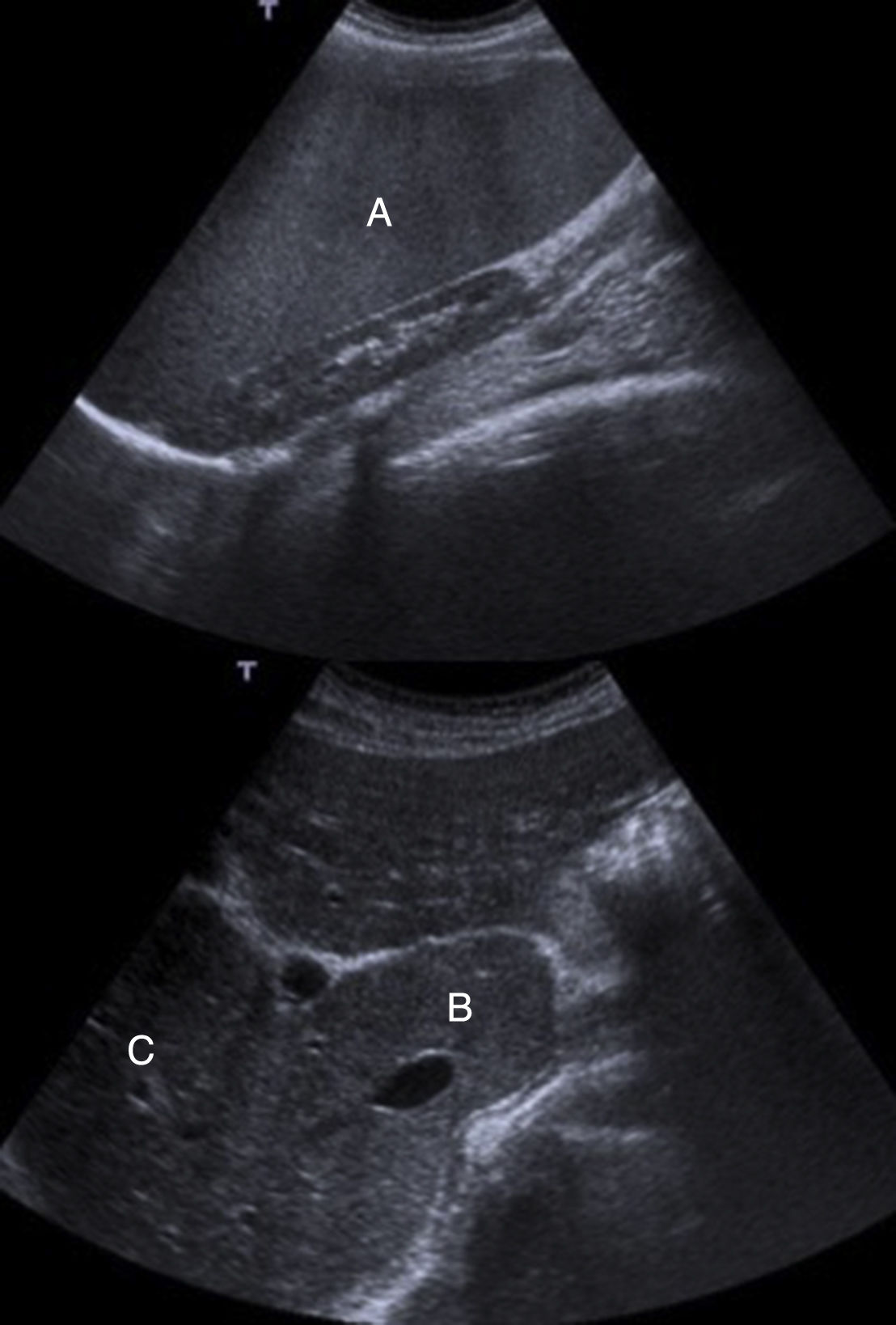
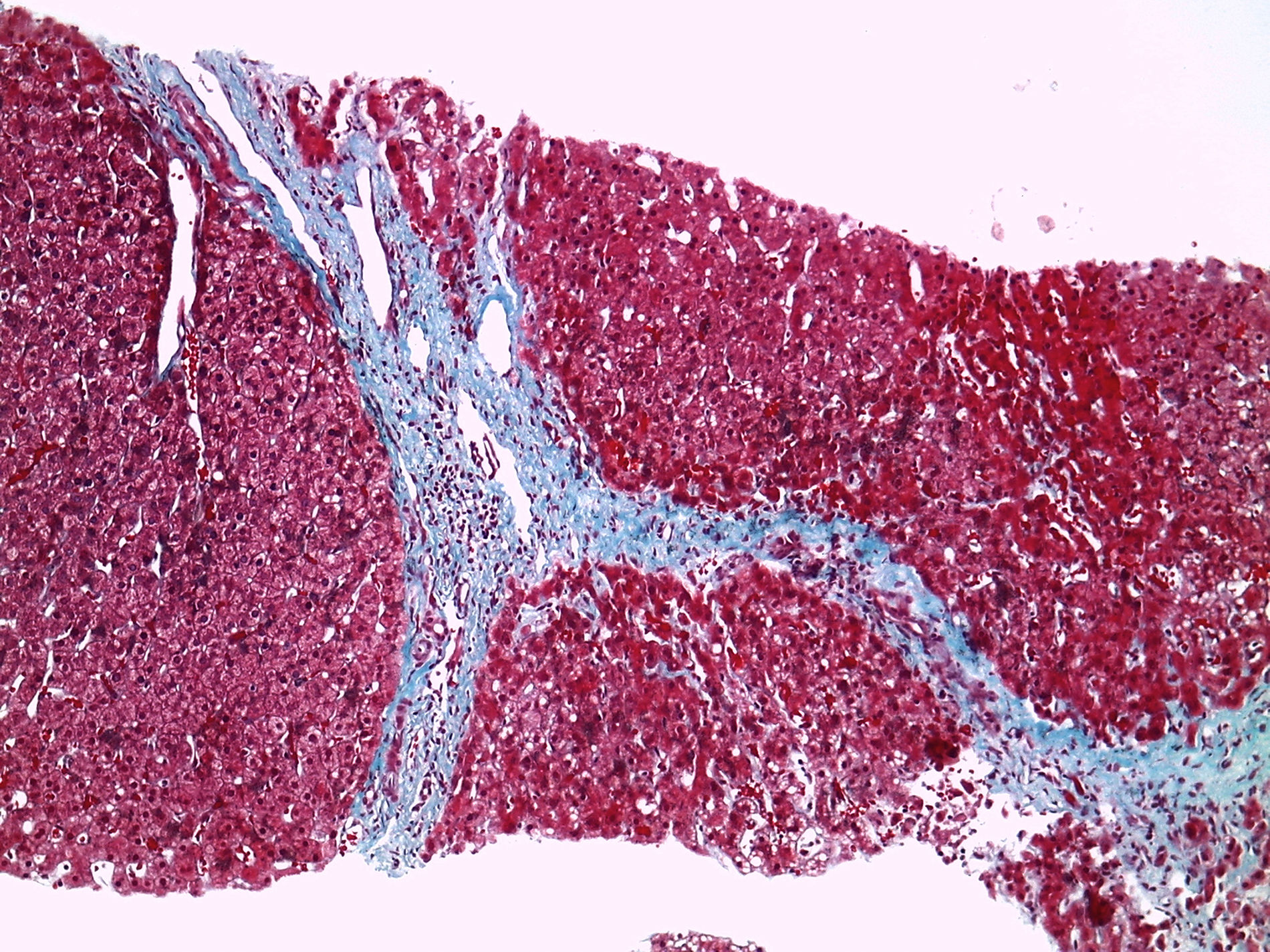
At the hepatology clinic, the patient reported no alcohol consumption, smoking, or taking any medication other than those previously mentioned. There were no abnormalities of note on physical examination. She had a BMI of 23.5kg/m2. A complete aetiological study was performed with serology negative for viral hepatitis (HBsAg and HCV-antibodies [Ab] negative), negative autoimmunity profile (anti-mitochondrial and M2 Ab, anti-LKM 1 Ab, antinuclear Ab [ANA], anti-SLA and LC1 Ab, anti-gp210 Ab and anti-parietal cell Ab). Wilson's disease, haemochromatosis and alpha-1 antitrypsin deficiency were ruled out. We also carried out a genetic test for coeliac disease, which was negative for all the alleles. Metabolic study showed cholesterol, triglycerides, glucose and insulin within normal parameters. Liver ultrasound showed a heterogeneous liver with signs of portal hypertension, hypertrophy of the caudate lobe and large splenomegaly of 184mm, without ascites (Fig. 1). Liver biopsy showed fibrosis bridges delimiting macro and micro nodules with mild necro-inflammatory lobular activity and mild steatosis, which confirmed the diagnosis of liver cirrhosis, but without any abnormalities to suggest the aetiology (Fig. 2). Upper gastrointestinal endoscopy did not show oesophageal varices.
It is common for patients with Turner syndrome to have abnormal liver function test results, for various different reasons.2 Abnormal liver function results have traditionally been attributed to hepatic steatosis because of the higher incidence of obesity and diabetes mellitus in these patients and to toxicity from the treatment with oestrogens,3 even though they have not been shown to cause liver toxicity.4,5
When non-alcoholic steatohepatitis progresses to liver cirrhosis the hepatic steatosis is known to disappear. This could therefore be the origin of the cirrhosis in our patient. However, as she was not overweight and did not have diabetes or dyslipidaemia, she had none of the associated factors.
A liver biopsy was performed directly on our patient because of the clear signs of cirrhosis on the ultrasound. However, it is important to consider the potential utility of transient elastography to determine the possible presence of liver fibrosis as an early method of detection in patients with Turner syndrome.
Turner syndrome is considered a rare and little-known cause of liver cirrhosis. However, a risk five-fold higher than that of the general population has been reported.6 Once other causes have been ruled out, the pathophysiological mechanism proposed in the aetiopathogenesis is that changes in the hepatic microvascularisation cause local tissue hypoxia, fibrotic changes and atrophy, associated with the hypothesis that this is due to the monosomy of the X chromosome. Depending on the distribution of the lesions, it may be associated with presinusoidal or sinusoidal portal hypertension.2,5
There are two cases reported in the literature with established liver cirrhosis related to Turner syndrome, one a Russian woman and the other an Israeli woman, but we were unable to analyse them because they are only in the original languages. However, four liver transplants have been reported in patients with Turner syndrome.7 In two of the explants, idiopathic portal hypertension is reported and, of all microvascularisation abnormalities, this probably plays an important role in the development of cirrhosis.2,7 In the third case, atrophy of the liver without fibrosis is described, associated with hypotrophy of the intrahepatic portal venous system, known as Cruveilhier–Baumgarten syndrome, which presents with presynusoidal portal hypertension.8,9 In the fourth case, no information is published on the explant; the patient had pulmonary sarcoidosis and non-caseating granulomas were found in the liver biopsy.10
In conclusion, patients with Turner syndrome have a higher risk of liver cirrhosis than the general population. Therefore, in the absence of more studies, stricter liver monitoring should be considered, particularly in patients with impaired liver function.
Please cite this article as: Machlab S, Miquel M, Voltà T, Escoda MR, Vergara M. Síndrome de Turner como causa de cirrosis hepática. Gastroenterol Hepatol. 2018;41:308–309.